SUBJECT KNOWLEDGE
• Physical effects of immobility
• Spinal anatomy
• Risk factors associated with back pain and injury
• Risks related to moving and handling
• Ergonomics
• Psychological and social aspects of mobility
CARE DELIVERY KNOWLEDGE
• Multidisciplinary assessment of mobility
• Principles of load handling
• Assessment of clients’ mobility for moving and handling
• Planning to assist with mobility and movement
• Implementation and evaluation of assistance with mobility and movement
PROFESSIONAL AND ETHICAL KNOWLEDGE
• Facilities for mobility care
• Laws relating to disability
• Laws related to moving and handling
• Impact of Human Rights Act
• Professional guidelines
• Barriers to safe moving and handling
PERSONAL AND REFLECTIVE KNOWLEDGE
• Experiencing impaired mobility
• Caring for yourself
• Case studies
INTRODUCTION
Moving and handling and assisting patient mobility are often addressed separately, yet in practice an interdependent relationship exists. It is therefore useful to clarify our understanding of these terms from the outset. Dictionary definitions describe mobility as having the freedom or ability to move, whereas moving involves a change of place, situation or posture. Health professionals use ‘mobility’ to denote functional capacity, which means being able to get up, bend down, sit, stand, walk, run, dance, etc. and to perform such movements without assistance. ‘Moving and handling’ is reserved for interventions which assist moving or transferring people (or objects) from one situation to another. Essentially, ‘mobility’ and ‘mobilizing’ refer to patient or client activity while ‘moving and handling’ emphasize the carer’s involvement. These two fundamental components of nursing are considered together in this chapter, as their related skills and knowledge are often combined to achieve goals of care.
Most people take mobility for granted, yet life’s essential activities depend on it. In the first few weeks of life humans are incapable of independent movement but as small children learn to balance, they progress through sitting, standing, walking and more advanced moves. Beyond early childhood most individuals wake up each morning without restrictions or limitations, but for those whose mobility is impaired basic tasks such as getting out of bed or walking to the toilet require great effort or may be impossible without assistance. Impaired mobility may be experienced temporarily when health issues occur in life or as a progressive deterioration in response to disease or the ageing process. For some it is a routine and permanent way of life.
Definitions tend to depict mobility in purely physical terms, yet loss of function impacts on normal human development and quality of life. The concept of an optimum level of mobility changes throughout the lifespan and is not necessarily the same in all cultures. Where an environment caters primarily for those with optimum capacity, anything less tends to be regarded as a disability and may have consequences for a person’s psychological and social health. As well as inherent physical, psychological or social issues, mobility may be compromised by therapeutic and diagnostic interventions. Caring for people with impaired mobility is therefore applicable to all branches of nursing and poses significant challenges.
As with mobility, handling situations are experienced in all aspects of life. Adults automatically lift babies and children, and processes of fetching, carrying, moving and rearranging are part of maintaining a functional environment. Back pain is associated with mechanical loading of the spine yet this chapter presents evidence of numerous factors affecting human performance. The nature of nursing work logically suggests that nurses are particularly at risk of back injury. The adult human form is an awkward load to move; it weighs several times more than a heavy bag of shopping, has no handles, lacks rigidity, may be uncooperative, and is liable to severe damage if mishandled or dropped. Add to this the confinements of clinical and community settings and the requirement to move people between beds, trolleys and toileting facilities, and nurses are faced with a situation that would be tolerated by few industrial workers. Injuries and accidents attributed to moving and handling constitute an enormous and costly problem in the health service (Department of Health 2004).
The overwhelming focus of literature relating to manual handling is staff health and safety, yet poor practice inevitably threatens the safety and potential recovery of patients. Legislation, supported by guidance from professional organizations, continues to be introduced, updated and amended to provide a framework for moving and handling practice. You will learn that this may pose conflicting demands in your day-to-day work. New methods rapidly evolve as knowledge in this field develops and innovative equipment continues to be manufactured. Moving and handling therefore represents a dynamic and rapidly developing area of health care that has implications for the safety and well-being of all involved.
The purpose of this chapter is to unravel some of the complexities surrounding moving and mobility and provide direction to your practice. It is important to recognize that practising patient handling in a skills laboratory or reading about recommended techniques is not enough to equip you with the skills required in clinical practice. This chapter does not describe specific manoeuvres but emphasizes principles of patient handling, incorporating an ergonomic approach, to promote safer practice.
OVERVIEW
Subject knowledge
For knowledge related to human mobility, the musculoskeletal system is examined. The effects of exercise and impaired mobility on the individual are explored, including perceptions and attitudes towards disability in society. Anatomy of the spine is described in relation to the causes of back injury and associated risks for moving and handling clients.
Care delivery knowledge
Explanation of practical aspects in assisting people to move and mobilize is covered, including information on assessment tools and procedures to select the most appropriate methods, equipment and human resources. Strategies for planning care, implementing and evaluating interventions are discussed.
Professional and ethical knowledge
Relevant legislation and professional guidelines are presented. Issues such as accountability and responsibilities in mobility care are addressed while recognizing and exploring barriers to safe and effective practice.
Personal and reflective knowledge
The exercises and case studies in this section will help you to understand some of the problems faced by people with mobility difficulties and to consider appropriate interventions. On pages 146–147 there are four case studies, each relating to one of the branch programmes. You may find it helpful to read one of them before you start the chapter and use it as a focus for your reflections.
SUBJECT KNOWLEDGE
BIOLOGICAL ASPECTS OF HUMAN MOBILITY
THE MUSCULOSKELETAL SYSTEM
Active movements of the body require coordination of connective, muscular and skeletal tissues (the musculoskeletal system) via the central and peripheral nervous systems (Palastanga et al 2004). Impairment of any one of these will interfere with or prevent normal mobility.
The skeleton has many functions, as listed in Box 6.1. It comprises two types of specially modified connective tissue, bone and cartilage. The human skeleton is made up of 206 bones which are categorized into five types (Tortora & Derrickson 2007):
• long bones
• short bones
• irregular bones
• flat bones
• sesamoid bones.
Box 6.1
Support function
The skeleton is made up of two major bony components. The trunk or axial skeleton – comprising the spine, skull, ribs and sternum – and the limbs or appendicular skeleton. The axial skeleton is partly responsible for the upright posture of the body. It supports the appendicular skeleton, muscles, ligaments and tendons.
Movement function
The muscles that are attached to the bones move the skeleton. Bones also provide a system of levers (rigid rods that can be moved about a fixed point) on which a group of specialized tissues (muscles) act to produce motion. The fixed points around which the levers move are the joints.
Protection function
Bones protect internal organs from injury: the skull protects the brain, the rib cage protects the heart and lungs, the spine protects the spinal cord and the pelvis protects the lower bowel, bladder and the womb in females.
Blood-forming function
Through a process called haematopoiesis, the red marrow tissue contained within some bones produces red blood cells or erythrocytes; some white blood cells or leukocytes and platelets are also produced. The red blood cells transport oxygen around the body, leukocytes are vital to the immune system and platelets are vital to the clotting mechanism.
Storage functions
Bones store minerals (calcium, magnesium, sodium and potassium) and energy in the form of fat (yellow marrow). 97% of the body’s calcium is stored in bone. Calcium may be removed from bone to maintain a normal blood calcium level, which is essentially for blood clotting and proper function of muscles and nerves. Yellow marrow is mostly fat and an important energy reserve. It can be converted to red marrow if necessary (e.g., after severe blood loss).
(adapted with kind permission from Sarah Crowther 2008 The PH1 Handbook (functions of the skeleton), unpublished student handbook)
Each bone is enclosed in an outer layer of tissue called the periosteum, has an outer layer of compact bone and an internal network of cancellous bone (Palastanga et al., 2004 and Tortora and Derrickson, 2007). Compact bone is also known as Haversian bone because of the Haversian canals/tunnels running through it. These are surrounded by concentric rings of hard calcified lamellae. Nerves and blood vessels enter the bone through Volkmann’s canals which connect to the Haversian canals. Spaces between the lamellae (lacunae) contain mature bone cells called osteocytes. Lacunae are interconnected by micro canals called canaliculi. The canal network facilitates nutrition and waste removal. The compact bone serves as attachments for muscles via tendons, thereby facilitating movement.
Cancellous bone is sponge-like in appearance. It has an internal network of mesh-like substance called trabeculae. Red bone marrow lies between the mesh. This produces red blood cells. Two types of cells are associated with the trabeculae: the osteoclasts which reabsorb bone and the osteoblasts which lay down new bone. These cell types contribute to the formation of new bone after a fracture and the remodelling of bone in the later stages of healing.
Bone is very hard due to a matrix of fibrous connective tissue impregnated with calcium and phosphorus. Cartilage is supplementary to bone and is found wherever a combination of strength, rigidity and elasticity is required (Palastanga et al 2004).
Joints
The bones of the body come together to form articulations or joints. The articular surfaces at the end of bones are covered in cartilage which allows smooth movement. The type and extent of the movement depend upon the structure and function of the joint. Other functions of joints include providing stability during movement as well as maintaining body posture.
There are many types of joints in the body; not all are movable. To focus on mobility, only synovial joints will be considered. (For a full description of bones and joints see Tortora & Derrickson 2007: 7–16).
Synovial joints
Synovial joints are fundamental to full mobility and are termed ‘freely movable’. They are enclosed within a fibrous capsule of connective tissue. Articular or hyaline cartilage lines the ends of the bones. Joint stability is enhanced by ligaments which connect one bone to another, and by surrounding muscles which are attached, via tendons, to bones. While providing stability, these same structures guide and limit movement. The nerve supply to joints comes from the surrounding muscles. The joint capsule is lined with synovial membrane containing microscopic villi, which secrete synovial fluid to lubricate and nourish the articular surfaces. All synovial joints have a similar structure to one another, but they vary in terms of their shape and range of movement (Drake et al 2005; Fig. 6.1).
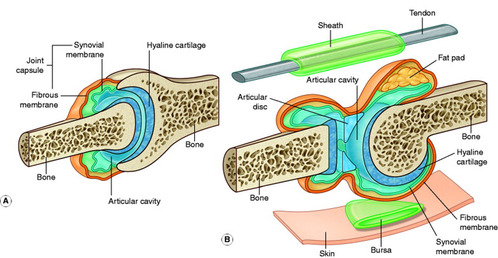 |
| Figure 6.1 (from Drake et al 2005, with kind permission of Elsevier). |
There are basically seven types of synovial joints:
• ball and socket joint
• hinge joint
• pivot joint
• plane joint
• saddle joint
• ellipsoid joint
• condyloid joint (Drake et al 2005).
It is important to learn about synovial joints in order to identify normal movement and the range that exists. However, classification of joints is not always consistent. For example the knee is referred to as a hinge joint, but this is not an accurate description since it moves in rotational directions. In older varieties of artificial knee joints, this led to a problem of loosening since they were designed only to act as a hinge and did not take into account the rotational forces exerted on the knee.
Gain access to a skeleton within your school or department and attempt the movements identified above on the skeleton.
• Attempt some of the common movements yourself.
• Make a note of the range that you may go through in a gym or exercise class when doing a ‘warm up’ or ‘cool down’ stretch.
• Sit on a chair and then flex and extend your knee; the movement created is that of a hinge. Now stand with your foot firmly fixed to the floor, try (within your limitations) to rotate at the knee joint. Notice how there is some rotational movement, but bear in mind that the ankle joint is also rotating.
Muscles
Skeletal muscles are attached to bones. Muscle is a unique connective tissue; it has specialized cells that allow contraction, which produces movement. Skeletal muscles are responsible for voluntary active movements which are coordinated by the nervous system. They are striated (striped) in appearance. For stability to be maintained and movement to occur, muscles need to work effectively. Muscle contractions not only allow movement but also maintain body posture. Another function of skeletal muscle is to produce heat, thus contributing to the body temperature (Drake et al 2005).
Active skeletal muscles require a great deal of energy. The nutritional aspects, especially sugar and carbohydrate intakes, are therefore of paramount importance. The full potential of mobility improvement or maintenance cannot be reached if there are nutritional deficits.
Blood and nerve supply of muscles
There is a rich blood and nerve supply to the skeletal muscles. Each muscle is supplied by at least one nerve that contains motor and sensory fibres. Impulses are transmitted to and from the muscles by chemical neurotransmitters. For further details see Evolve 6.1.
THE PHYSIOLOGY OF MOVEMENT
Body levers
In order for movement to take place a system of levers is used incorporating the structures of muscles, bones and joints. Muscles cross at least one joint between their attachments and movement is produced through a system of levers. These levers transmit energy through muscular contraction to move different parts of the body. All levers have a fulcrum, an effort arm and a resistance arm, and are classified according to the differing arrangement of these. By shortening the resistance arm, less effort is required to lift a weight. The relevance of this in assisting people to move is that holding the patient closer to your body reduces the muscular effort required to move them. (For a full description and explanation of the different body levers, see Palastanga et al 2004: 4–5).
Range of motion
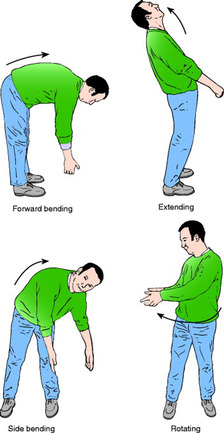
The total amount of movement available at any joint is termed the range of motion. To be effective in care and protect our patients we need to know the extent of movement and the limitations that exist. Therefore it is important to know the normal ranges of motion, as given below and in Figure 6.2:
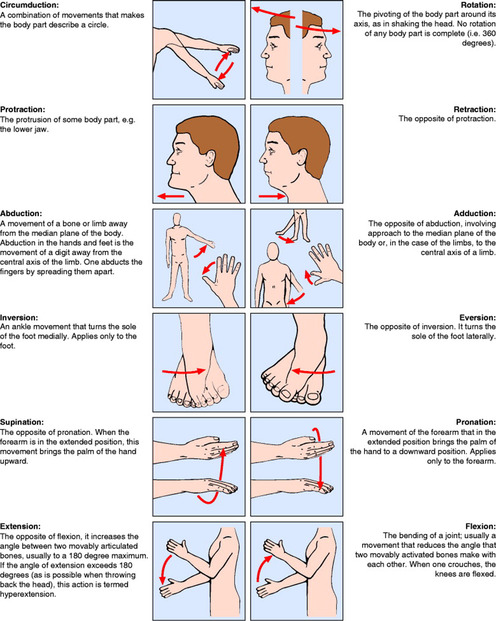 |
| Figure 6.2 (from Montague et al 2005, with kind permission of Elsevier). |
Single (plane) movements:
• flexion
• extension
• eversion
• pronation and supination
• abduction and adduction
• dorsiflexion and plantar flexion
• rotation.
Combined movements:
Movement at synovial joints is limited by the shape of the articulating bones and the structure of extracapsular (and sometimes intracapsular) ligaments. Other limiting factors are strength and tension of adjacent muscles or where two soft tissue surfaces come into contact with each other (Palastanga et al 2004).
PURPOSE AND BENEFITS OF MOBILITY AND EXERCISE
Joint range, muscle power, coordination and proprioception (awareness of the spatial position and movement of the body) are all vital to independent mobility. Exercise is fundamental in maintaining functional mobility because it improves or maintains these factors and contributes to general fitness, function, coordination, balance, relaxation, circulation and stability. Exercise also has psychological benefits with evidence suggesting improved self-concept and reduced anger, depression, anxiety and stress. Exercise is therefore necessary to maintain or improve our health. The level of an individual’s physical fitness is determined mainly by their capacity for energy output, neuromuscular function, joint mobility, and psychological factors (e.g. motivation) (Bouchard et al 2007).
National trends towards decreased physical activity have been identified, particularly in childhood, for over a decade (Wanless et al 2007). This has been matched by rising obesity levels and raises concerns about long-term effects such as high blood pressure, elevated blood cholesterol levels and coronary heart disease. Since government recommendations in 1996, improvements have been recognized; for example, 80% of pupils from schools participating in a national school sports initiative participated in at least 2 hours of physical education or sport each week in 2004. However, it was also recognized that a sustained effort up to and beyond 2011 was required to meet targets for adults (Wanless et al 2007). As a result of evidence of poor health, Scotland was one of the first countries in the world to develop a strategy for the development of physical activity (Scottish Executive 2003).
PHYSICAL EFFECTS OF IMMOBILITY
Reasons for impaired mobility are diverse. Physically, mobility is restricted when specific structures involved in facilitating movement (bones, joints, muscles and the nervous system) are affected by disease or injury. However, illnesses or degenerative conditions (such as cardiorespiratory disorders, Parkinson’s disease or Huntington’s chorea) and psychological and social problems can indirectly reduce functional mobility. Equally, impaired mobility, whether temporary or permanent, affects other systems of the body. This has important implications for nurses since many potential complications can be prevented or minimized by nursing interventions (Box 6.2).
Box 6.2
| Musculoskeletal | Muscle weakness and atrophy Contractures |
| Cardiovascular | Reduced venous return Venous stasis Deep vein thrombosis Pulmonary embolus Stroke Pressure ulcers Postural hypotension Oedema |
| Respiratory | Decreased lung expansion Bronchial pneumonia |
| Gastrointestinal | Decreased appetite Dehydration Constipation (and diarrhoea) Fluid and electrolyte imbalance |
| Metabolic and hormonal | Decreased metabolic rate Altered hormone secretion patterns Altered sleep patterns Bone reabsorption and osteoporosis Hypothermia |
| Neurological | Sensory–motor deprivation Diminished proprioception Reduced balance and posture control Disorientation |
| Other | Urinary stasis |
Musculoskeletal changes
Muscular strength and endurance are essential for normal movement and performing everyday activities. However, deterioration of muscle mass and strength is influenced more by inactivity than other lifestyle factors (Brouwer & Olney 2004) and can occur in as little as 48 hours of disuse (Prentice 2001a). A limb that has been immobilized in a cast is an excellent example. Muscle atrophy and weakness can be identified through girth measurements of the limbs, exercise tolerance and levels of fatigue. Where immobility is prolonged, connective tissue surrounding the joints, such as ligaments and the joint capsule, tend to lose elasticity and actually shorten (Prentice 2001b). This results in a reduced range of motion known as a contracture. Hips, knees, ankles, wrists, elbows and shoulders are at risk. Deformities such as joint fixed flexion or tendon shortening may result in pain, altered balance, diminished proprioception and postural impairment.
Cardiovascular changes
Since muscular activity promotes return of venous blood to the heart, reduced activity inevitably increases risk relating to poor venous return and venous stasis. In particular, thrombosis (formation of a clot on the interior wall of a blood vessel) often occurs in the lower extremities. Signs and symptoms of deep vein thrombosis (DVT) include mild fever and pain, swelling and tenderness to the affected area. If portions of the clot detach, the mobile embolus can lodge in a distal blood vessel causing impaired circulation to major organs such as the lungs or brain.
Pressure sore development is exacerbated by numerous factors, but is essentially a result of two processes resulting in circulatory disruption; firstly, occlusion of blood vessels by external pressure and, secondly, damage to the microcirculation by friction and shearing forces. Where pressure is applied to the body, the resulting tissue ischaemia leads to discomfort. Individuals naturally respond by adjusting their position and posture to restore the blood supply. However, for those unable to move, ischaemia leads to tissue damage. Friction and shearing damage can be exacerbated by poor positioning and moving and handling techniques (see Ch. 15, ‘Skin integrity’).
When confined to bed, individuals may drop their blood pressure when assuming a standing posture (postural hypotension) leading to them feeling dizzy with potential to faint.
Respiratory changes
If, through immobility, recumbency (lying down) is increased, then the pressure of the abdominal contents pushing on the diaphragm reduces lung volume. Stress is placed on the muscles of inspiration, leading to inefficient respiratory muscular action. Reduced efficiency of the respiratory muscles can lead to an inability to cough effectively and subsequent accumulation of mucus. This creates a perfect medium for the growth and multiplication of bacteria. A chest infection is a major cause of sepsis which increases metabolic demand and systemic oxygen requirements. This affects oxygen supply to the skin making it more susceptible to pressure damage.
Gastrointestinal changes
Inactivity can affect gastrointestinal motility and appetite for food. Decreased food intake, also affected by a lowered metabolic rate, can result in constipation. ‘Overflow’ diarrhoea due to faecal impaction can, in turn, lead to dehydration and electrolyte imbalance.
Metabolic and hormonal changes
In periods of immobility, the basal metabolic rate decreases, since energy requirements are reduced, and protein is broken down due to muscle catabolism (demonstrated by increased urinary nitrogen). Both lead to increased body fat. Immobility is known to cause a range of other changes such as decreased bone density, calcium wastage, hypothermia and disruption of circadian rhythms (physiological patterns based on a 24 hour cycle such as sleeping, eating and secretion of hormones).
Neurological changes
Deprived of the ability to move, a person is also deprived of sensory–motor appreciation and control of posture and balance (Edwards 2001). An additional consequence is spasticity, a disorder of spinal reflexes that presents as increased muscle tone and overly brisk tendon reflexes (Edwards 2001).
Reflecting on your practice placements, use the information provided in this section thus far, along with personal knowledge, to:
• Review reasons why some of your patients/clients had impaired mobility.
• Decide whether their altered mobility was temporary or permanent.
• Review the rationale for patterns of care and treatment you have seen to improve mobility or overcome the effects of immobility.
BIOLOGICAL BASIS FOR MOVING AND HANDLING
In dealing with the dual aspects covered in this chapter – that is, the ‘mobility’ of the patient/client and ‘mobilizing’, which deals with moving and handling patients – the following section focuses on the potential effects of moving and handling activities on the health and well-being of nurses or carers. In order to have a better understanding of the mechanisms involved, it is important to have some knowledge of the human spine.
THE SPINAL COLUMN
The spinal column comprises 33 bones (vertebrae) with discs between them. Its functions include distributing forces, providing attachments for ligaments, muscles and ribs, and as a protective cover for the spinal cord. For descriptive purposes it is divided into five sections (Fig. 6.3) but mechanically it functions as a single unit. Each vertebra is composed of a main body of bone at the front (vertebral body), the vertebral foramen (the vertebral arch) which surrounds the spinal cord, bony projections (spinous processes) situated at the back and at the sides (transverse processes). These provide the attachment for muscles and ligaments (Palastanga et al 2004).
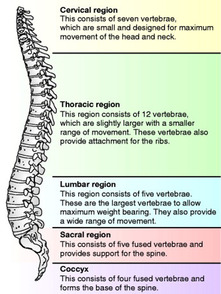 |
| Figure 6.3 |
The human spine, of which the spinal column and cord are component parts, forms a shallow ‘S’ shape when viewed from the side. These curves are a vital part of the way the spine functions and give it strength and stability. The vertebrae are different shapes and sizes according to their type and function. For instance, the cervical vertebrae are smaller and their shape is designed to facilitate movement of the head and neck, whereas the lumbar vertebrae have larger bodies to carry more weight. Disc structure follows a similar pattern. The whole structure is designed to resist compressive forces and to facilitate a variety of movements (Fig. 6.4; Palastanga et al 2004). The spine is flexible but is strongest when maintained in its normal alignment (‘S’ shape). Persistent poor posture, such as forward bending, twisting and slumped seated positions, and excessive, repetitive or awkward manual handling tasks increase the risk of back disorders; however, a strong back that has adapted to mechanical loading is less likely to become injured (Adams & Dolan 2005).
 |
| Figure 6.4 |
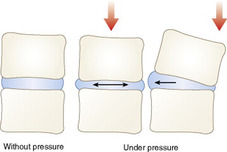
Intervertebral discs
Between each vertebra is an intervertebral disc which consists of an outer fibrous cartilagenous ring and a soft jelly-like nucleus. They are designed to resist compression and rotational forces and have a small shock-absorbing effect. However, sustained pressure on the anterior wall of the disc (forward flexion of the spine, slumped sitting) forces the nucleus backwards, causing excessive pressure on the posterior disc wall (the weakest part of the disc). This can cause cracks to occur and further sustained pressure can cause the wall to break down completely and the nucleus material to herniate. This is commonly referred to as a ‘slipped disc’. If the herniation compresses nearby nerves, acute pain and nerve damage can result. Figure 6.5 indicates how the disc modifies its position to take account of this pressure (Drake et al 2005).
BACK PAIN/INJURY
The relationship between back problems, poor posture and load handling techniques is explored along with the importance of an ergonomically friendly environment for moving and handling.
Precise data on the extent of back injury in our society are difficult to achieve since the pathology and associated risks are complex and diverse. For example, pain may be caused by disc herniation, muscle strain or bone degeneration; individuals may be at risk because of genetic and lifestyle factors as well as the nature of their work. However, evidence suggests that back pain is experienced by the majority of adults although most individuals cope without seeking treatment (May 2005). Episodes of back pain are often short-lived but they may be a precursor to more serious or prolonged disorders.
Certain predisposing factors help identify those who are at greatest risk of developing mechanical damage to spinal tissues (Adams & Dolan 2005) and these are listed in Box 6.3.
Box 6.3
Genetic inheritance
Advancing age
Repetitive loading
Excess weight
Smoking
Weak back or abdominal muscles due to absence of regular exercise
Extreme lordosis (increased degree of lumbar curvature in the back)
Loss of lordosis (normal lumbar curvature is decreased in flexed postures)
RISK FACTORS IN THE WORKPLACE
Risk factors refer to characteristics that make a person susceptible to a particular condition (May 2005). Although these are presented in a workplace context, they are equally relevant to other daily activities. In terms of low back pain, risk factors can be grouped into two major areas: biomechanical and psychosocial.
Biomechanical
Specific biomechanical risk factors have been identified from numerous studies. Key activities that result in back injury are described in Box 6.4. To summarize, during lifting or transferring, the weight of the load (and upper body if bending forward) generates compressive forces on the spine that can lead to damage. When these forces are combined with bending and twisting, the risks are increased. Individuals who have to work with their spine flexed forward (and rotated) for repeated or prolonged episodes are, therefore, more at risk.
Box 6.4
Stooping
Bending movements cause the spine to lose its natural curves and make it more vulnerable to injury. Normally, high levels of stress (external force) are only generated by bending forward to the maximum extent. However, when bending is repeated or continued, or after sustained spinal loading, bending stresses become high in more limited stooping positions
Twisting
Repeated activity that increases pressure on the intervertebral discs, particularly if the pressure is uneven, can ultimately lead to prolapsed discs. Adding torsion to bending and compression increases the risk of damage to discs and ligaments
Static or awkward postures
An environment that forces work to take place in non-neutral postures (see above) or at extremes of range of motion will increase stress to the tissues. Maintaining fixed postures is common in many healthcare settings and even if postures are neutral, fixed postures could lead to vulnerability
Cumulative strain
Most people think that trying to move an excessive weight, even if it be only once, is the situation most likely to result in injury. In fact this is rarely the case. Repeated movements of moderate weights have far greater potential for harm than a single maximal effort (Bridger 2002). This cumulative effect also relates to task duration since the longer tasks are performed the greater the applied loads. This concept is recognized as a contributing factor to injury among nurses. Poor practice, therefore, may not result in one identifiable injury but ongoing gradual wear and tear which may later cause pain and disability
Other work related physical stresses include moving heavy or uneven loads, generalized fatigue and environmental factors such as lighting, temperature and noise. Biomechanical factors have enormous implications for the way manual handling activities are performed (see Care Delivery section).
Psychosocial factors
Increasing evidence points to the significance of psychosocial factors (in particular, attitudes about work) in the onset or recovery from back pain and disability. Some perceptions of work that may act as barriers to recovery are listed in Box 6.5.
Box 6.5
Unable to make full use of skills
Low job satisfaction
Little control over nature and methods of work
Belief that work is harmful to the back
Insufficient rewards
Limited social interaction or support
Unhelpful management style
Repetitive or monotonous tasks where a pace is imposed
Taking measures to prevent back injury is important in nursing. Further information regarding taking care of yourself can be found in the Personal and Reflective Knowledge section.
RISKS ASSOCIATED WITH MOVING AND HANDLING
Risks to the client
Risks to those being assisted to move or transfer include the following:
Pain or discomfort
Most methods involve the person being held by handlers, equipment or both. Discomfort may be caused at the physical points of contact and careful attention should be paid to observing and preventing this. Research supports a relationship between nurses’ skills in patient transfers and the safety and comfort of patients (Kjellburg et al 2004).
Injury
Falls are common and present significant risks to both patient and handlers (Patient Safety Observatory 2007). The risk of injury to patients through falls is therefore considerable, especially in the absence of a thorough assessment. Depending on severity, injuries could include soft tissue damage, joint dislocation, shearing and friction to the skin, bone fracture or severe head injury.
Resistance to future procedures
Perceptions of being moved vary considerably. The procedure may promote comfort and security for some and a loss of control for others. Negative experiences of being moved can lead to loss of confidence, self-esteem, dignity and, ultimately, reduced patient cooperation in rehabilitative and self-care processes.
Risks to nurses and other carers
Manual handling, in any context, is associated with back injury and other musculoskeletal disorders. Handling people poses additional problems particularly for nurses. Statistics are likely to underestimate the issue due to unreported incidents but additional studies clearly suggest that it is one of international significance (see Evidence-based Practice). The association between patient handling activities and musculoskeletal problems is evident, but the impact of value systems, such as stress, perceived lack of support and unpleasant work environments, needs to be recognized as well as the mechanical factors (Johnson 2005). What cannot be calculated from statistics is the personal suffering and social and financial impact on individuals who have been injured.
The extent of work related back problems in UK
• A survey of self-reported work related illness (Health and Safety Executive 2007a) estimated that in 2005/6, 1% of people in Great Britain suffered from a back disorder that was caused or made worse by their work. This resulted in an estimated loss of 4.5 million working days.
• True costs to industry are difficult to ascertain, but at least 5 million adults consult their GP annually concerning back pain (Palmer et al 2000) and statistics from Back Care demonstrate that the financial burden of back pain is considerable (Back Care 2007).
• Health and social care is one of the occupations with above average prevalence rates of work related back disorders (Health and Safety Executive 2007b).
• In the health services, over 5000 manual handling injuries are reported each year which account for 40% of absence from work. Approximately half of these injuries occur during the handling of patients (Health and Safety Executive 2007b).
• The overall proportion of accidents related to moving and handling increased from 17% to 18% between 1996 and 2003, whereas a decrease of 6% was reported for slips, trips and falls (National Audit Office 2003).
• One in four nurses has taken time off work with a back injury sustained at work (Department of Health 2002).
ERGONOMICS
Since the publication of the Manual Handling Operations Regulations 1992, increasing emphasis has been given to ergonomic approaches to moving and handling (Nicholls, 1997 and National Back Exchange, 2002). The word ‘ergonomics’ is Greek in origin and means natural laws (‘nomo’) of work (‘ergo’). The guiding principle of this science is to optimize the match between the demands of a task, whether physical, social or psychological, and the capabilities of the individual performing it. This can be achieved by designing appliances, adapting the environment, introducing or reorganizing systems of work or changing the task.
Examples of ergonomic approaches to assisting people with mobility include:
• Provision of electric beds, hoists or other lifting/transferring devices to make the task easier and reduce risks.
• Designing hospital bed spaces and toilet areas to make the environment more appropriate to the task.
• Partnering practitioners in areas of high demand or storing ‘single patient use’ slide sheets at patients’ bedsides to maximize efficiency and effectiveness in the activities undertaken.
• Interdisciplinary risk assessment tools to promote compatibility between the task and those performing it.
Ergonomics, therefore, aims to ‘fit’ the work situation to the people to improve performance, safety, health and well-being (Bridger 2002).
PSYCHOSOCIAL
PSYCHOLOGICAL AND SOCIAL EFFECTS OF IMMOBILITY
In order to understand some of the personal and social impact of immobility in our society, it is important to appreciate the significance of ‘normality’. From birth, babies are assessed against criteria of normality. This continues as milestones are expected at specific points throughout the lifespan. Perceptions of normality vary according to cultural background but where criteria are delayed or not achieved people may be viewed as different or inferior. In societies that assume full mobility, reduced mobility can lead to stereotypical views and negative attitudes. Such stigmatization (acquiring an identity from the reactions of other people) can result in labelling (Walker et al 2007) which is often a false reflection of reality; for example, people with physical impairment can be perceived as having reduced learning capacity. Inappropriate interactions can lead to loss of self-esteem and subsequent withdrawal from society. (Further information on labelling and stigma can be found in Ch. 19, ‘Rehabilitation and recovery’.)
Social exclusion manifests itself as the reluctance or inability to engage in everyday activities such as interacting with people, visiting friends and relatives, accessing services and undertaking domestic activities. It is arguable that, in many respects, society assists withdrawal by providing centres, homes and schools for those with special mobility requirements. In developed societies, older people tend to be associated with immobility and non-productivity which is usually related to the age of retirement. Clarke & Warren (2007) point out that although the notion of ‘active ageing’ permeates national and international policies, it tends to be interpreted in relation to physical activity and capacity to work rather than ability to realise individual potential in other ways.
Altered mobility may also affect close relationships and partnerships since the dynamics may be upset by one partner becoming physically dependent on the other. Where employability is affected, there may also be financial dependence and loss of self-esteem. Either partner’s appetite for or enjoyment of sex can be affected by physical restrictions, fear of pain and doubts about attractiveness, and questions may be raised about the potential for pregnancy, childbirth or looking after young children (Arthritis Research Campaign 2004). Since most health professionals require full mobility to pursue their chosen career, it can be difficult to appreciate the practical and emotional challenges of reduced mobility. By examining psychological and social dimensions, insights into associated problems such as depression, isolation and loss of self-reliance and dignity can be gained.
PUBLIC PERCEPTIONS OF DISABILITY
In developed countries, full mobility is often viewed as the norm and impairment of this function as abnormal and undesirable. In other words, it is seen as a disability. This can create social, psychological and physical barriers in a society that is structured around ‘able-bodied’ people. Disability is a multifaceted concept (LoBianco & Sheppard-Jones 2007) and it is important to examine this to appreciate how it might impact on everyday lives.
There are two major models of disability, the medical model and the social model. The first identifies a disabled person as someone with a physically limiting condition or impairment. For example, the Disability Discrimination Act (DDA) 2006 defines a disabled person as someone having a physical or mental impairment that has a substantial and long-term adverse effect on his or her ability to carry out normal day-to-day activities. (Further information on laws relating to disability can be found in the Professional Knowledge section.) The World Health Organization (WHO; 2008) defines impairment as any loss or abnormality of psychological, physiological or anatomical structure or function. These definitions would include, for example, people with learning difficulties, non-standard forms of communication, hearing or visual impairment or those requiring mobility aids. The impairment, therefore, is the physical or psychological deviation from ‘normal’ and the disability is what results from that change. A limitation of the medical model is that impairment and disability are not always directly related. It is possible to have a high degree of impairment (biomedical change) with a low degree of disability (loss of function) and vice versa. Consider an example where two individuals suffer from a prolapsed intervertebral disc. Scans may reveal the same degree of ‘impairment’, that is identical degrees of anatomical damage, but the disability or extent of function could vary greatly.
The social model of disability focuses on society’s response to disability rather than the individual. It proposes that disability only exists because society refuses to remove environmental barriers that people with impairments encounter. As such it offers a very different meaning of disability. Public perceptions of disability do not distinguish between these concepts and the terms ‘impairment’ and ‘disability’ are used interchangeably. Goffman (1963) considers that the greatest problem faced by people with a disability is not their functional limitations but society’s response to them (see Ch. 19 for further discussion).
From birth to adulthood, mobility related goals are perceived as part of normal development, not only by health professionals but also by the community. We need only to look at our own environment, where there are steps, narrow doorways and cramped workplaces, to see the boundaries created for a person with impaired mobility. Arguably, schools have been designed with the expectation that children are fully mobile and therefore ‘disabled’ children were expected to attend a special school. In the past, and to an extent today, institutions were designed to house those with disabilities for most of their lives which served to marginalize them from the rest of society. The introduction of the Special Education Needs and Disability Act 2001 makes it illegal for educational establishments, in particular in further and higher education, to discriminate against students with a disability. In general, progress has been made to ensure provision of access and facilities in schools and other public places. Recently, attempts have been made to integrate children with special needs into mainstream schools. This remains a controversial topic of debate since, although the notion of normality is promoted through socialization, it is argued that resources are insufficient to meet the children’s particular needs.
Adolescence can be a challenging time for any individual and it brings the same bodily changes and sexual urges for those who are disabled as for anyone else. This is easily overlooked and a young person with mobility impairment may feel frustrated and inadequate because of their physical limitations.
People tend to experience more problems with mobility as they get older. Musculoskeletal system changes tend to cause people to walk slower, take shorter steps and become more unsteady. Consequently, older people become associated with disability. It is interesting to speculate how, with an increasingly ageing population, our concept of normality may change.
Next time you have an opportunity to observe a carer assisting a disabled person or pushing a person in a wheelchair in a public setting:
• Notice interactions between the disabled person, carer and others.
• Do others concentrate upon the carer or the disabled person?
• Is there any lack of interaction?
• Is there any inappropriate interaction such as staring?
• Recall, honestly, how you feel and react when you meet a disabled person, particularly of your own age, in a social setting.
• How could knowledge gained from this chapter affect your attitude and feelings in future?
CARE DELIVERY KNOWLEDGE
This section addresses multidisciplinary assessment of mobility and explores the principles of mobility care. It focuses in more detail on the assessment and safe management of moving and handling people.
MULTIDISCIPLINARY ASSESSMENT OF MOBILITY
Caring for people in hospital and community environments involves not just nurses but healthcare professionals from a range of disciplines. The terms ‘interprofessional working’, ‘integrated care’, ‘interagency working’ and ‘collaboration’ are all terms currently used to describe integrated approaches to health care (Atwal & Caldwell 2002). Integrated care pathways (ICPs) are structured, multidisciplinary care plans which outline essential steps in the care of a patient with a specific clinical problem (Campbell et al 1998). A single document may therefore be used to facilitate the management of patients or clients with mobility problems where several disciplines are involved. Where appropriate, individual care plans may be written by occupational therapists, physiotherapists or nurses. This is usually determined by whichever profession makes first contact. The ‘single assessment process’ is a key target in the National Service Framework for Older People (Department of Health 2001) that involves one person-centred assessment to which different disciplines contribute. This aims to facilitate integrated provision of services and effective management of care. Nurses play an important part in this coordinated approach because of their close, regular contact with patients.
Make a list of those professionals and non-professionals who may directly or indirectly contribute towards the care of people with limited mobility. From this list identify their different priorities in caring for:
• an adult
• a child
• a person with a mental health problem
• a person with a learning disability.
How could a nurse contribute to the decision-making process of this team?
Using tools and scales has become increasingly important in helping nurses to manage individual care more effectively. They assist in producing a more objective assessment of an aspect of care or provide a numerical measure of risk. In addition, they provide evidence that these processes have been undertaken. For example pain may impede a person’s mobility which may in turn place them at risk of developing pressure ulcers. In these instances tools such as pain scales and risk assessment tools for pressure ulcers would be useful in the overall management of this type of patient (see Ch. 11, ‘Pain’, and Ch. 15, ‘Skin integrity’, for full descriptions). Various tools exist to assess mobility. One example is the Barthel Activities of Daily Living (ADL) scale (Mahoney & Barthel 1965) which measures dependency on a 0 to 20 point scale. Another is the Assessment of Motor and Process Skills (AMPS) which is considered to be more sensitive in community settings (http://www.ampsintl.com/).
To provide a holistic approach to mobility assessment it is important to remember that factors such as the person’s beliefs, motivation and their perceptions of mobilizing need to be taken into consideration. Similarly, when assessing children or individuals with learning disabilities or mental illness their levels of understanding need to be taken into account. When preparing for discharge it is useful to undertake assessment in the patient’s own home or in very similar conditions. For more information please access Evolve 6.2.
MANAGEMENT OF MOBILITY CARE
Management of mobility care and rehabilitation requires knowledge and understanding of specific factors relating to functional capacity. These include:




• range of movement
• gait and body alignment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access