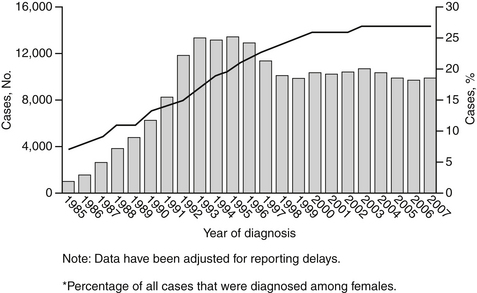
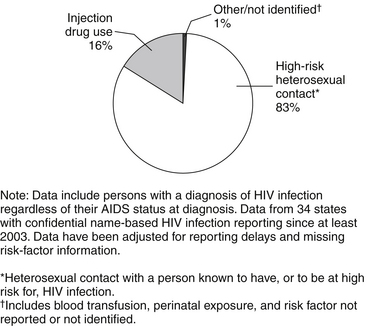
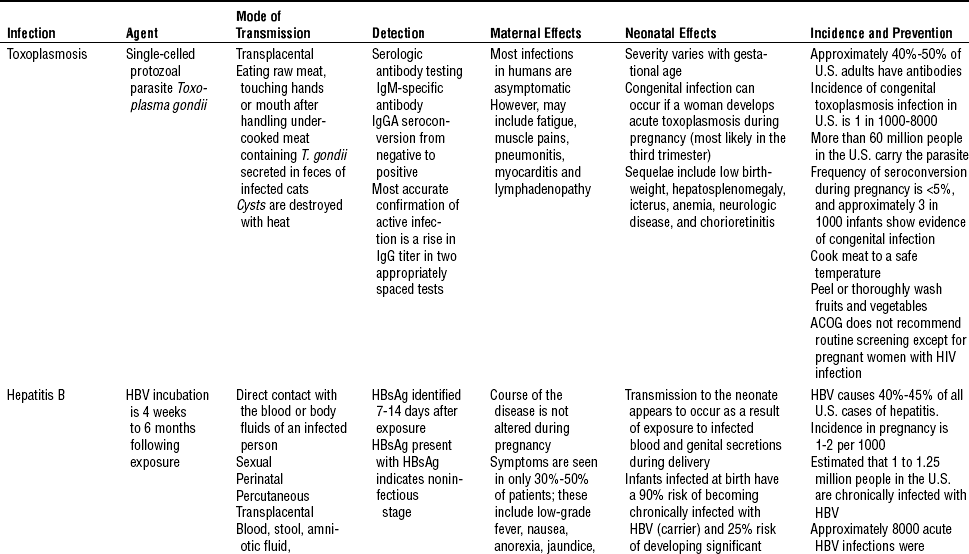
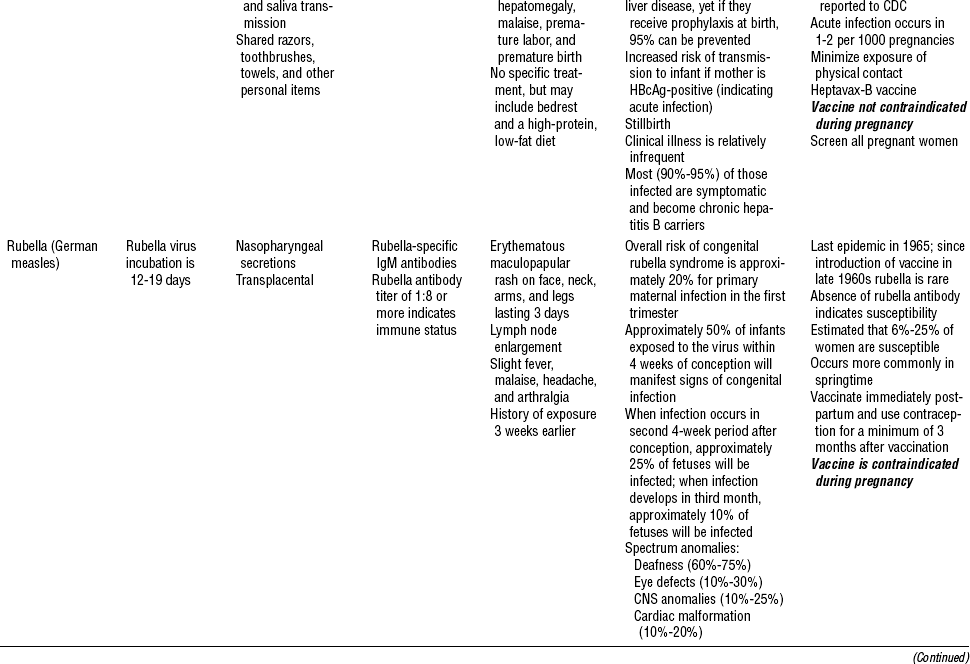
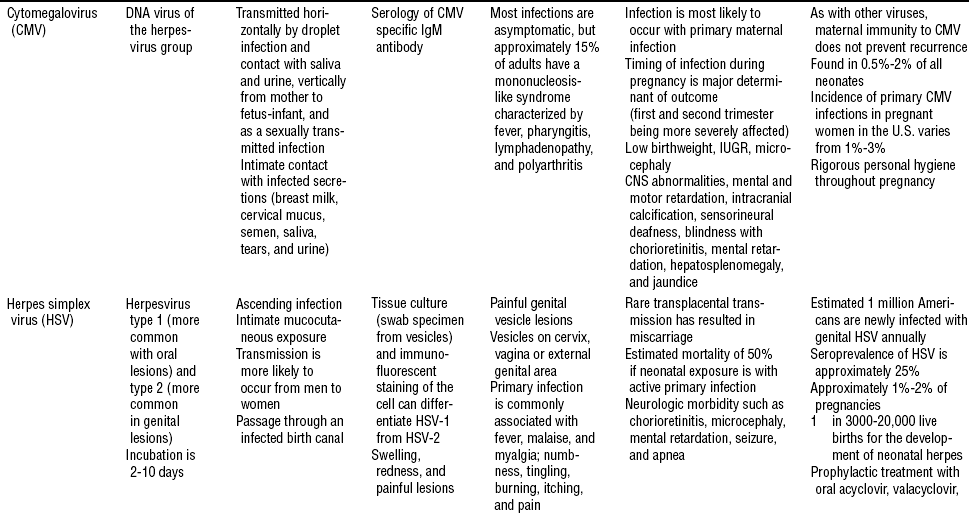
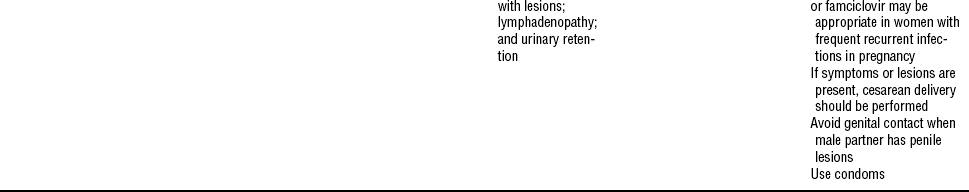
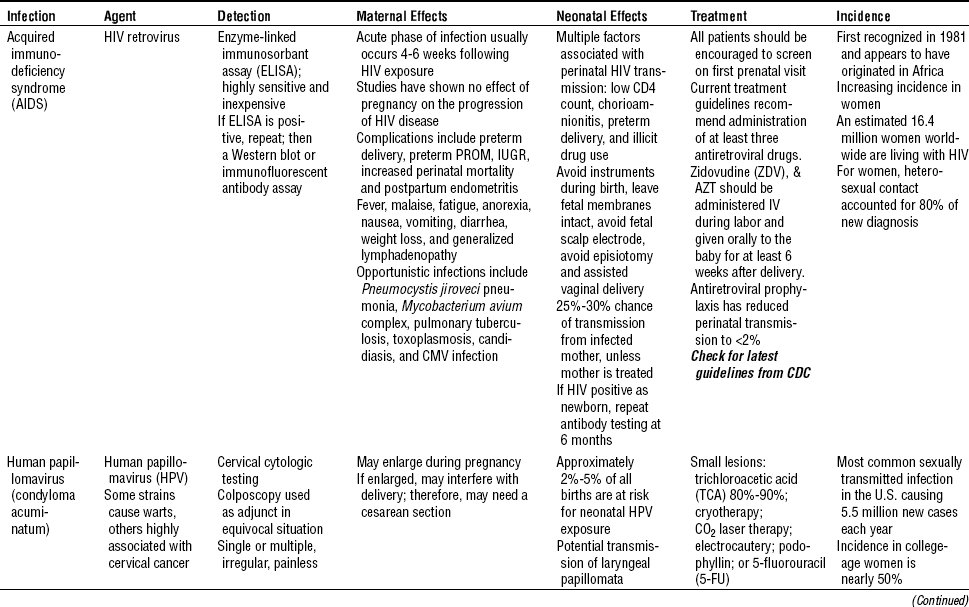
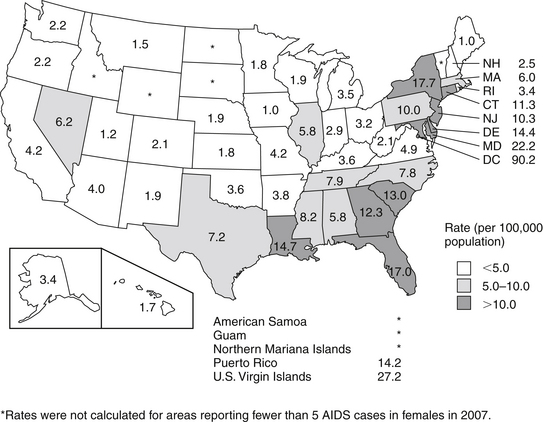
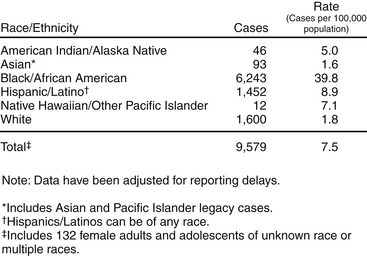
CHAPTER 20 1 Identify causative pathogens and describe primary signs and symptoms of perinatal infections. 2 Identify risk groups for acquired immunodeficiency syndrome (AIDS) and other sexually transmitted infections (STIs). 3 Correlate history and physical findings with early indicators of maternal infection. 4 Recognize clinical signs and symptoms of perinatal infections. 5 Discuss potential fetal complications associated with maternal infections. 6 Formulate nursing interventions from information obtained in the history. 7 Define health-education strategies to prevent maternal infections. Maternal and perinatal infections are common complications of pregnancy. Some infections affect only the mother, such as urinary tract infections (UTIs) and trichomonas infections. Others such as rubella, cytomegalovirus (CMV), and parvovirus infections have little effect on the mother but cause significant fetal injury; and others such as gonorrhea culture (GC), syphilis, toxoplasmosis, rubella, group B streptococcus, pyelonephritis, chorioamnionitis, and human immunodeficiency virus (HIV) may cause serious problems for mother and infant (Duff, 2007). Fetal infections may be acquired transplacentally; organisms may also ascend into the birth canal or be acquired during the passage through the vagina at the time of birth. Preconception counseling is imperative in preventing many infections such as rubella, rubeola and varicella. These vaccines should not be administered during pregnancy. The (CDC) recommends all pregnant women receive the influenza vaccine at any time during pregnancy because pregnant women often become more ill with influenza (www.cdc.gov/vaccines/vpd.html). A TORCH is an acronym for a group of five infectious diseases. TABLE 20-1 Centers for Disease Control and Prevention. (2009). Cytomegalovirus. Available online at: www.cdc.gov/cmv/pregnancy.html. Centers for Disease Control and Prevention. (2009). FAQ’s for health professionals. Available online at: www.cdc.gov/hepatitiis/HBV/HBVfaq.htm#oview.html. www.cdc.gov/cmv/pregnancy.html. www.cdc.gov/hepatitiis/HBV/HBVfaq.htm#oview.html. www.marchofdimes.com/professionals/14332_1201.asp. www.marchofdimes.com/professionals/14332_1225.asp. www.marchofdimes.com/professionals/14332_1226.asp. B Each disease is teratogenic. a. Lymphadenopathy: suboccipital, postauricular, cervical b. Rash: pink or red maculopapules c. Ulcerated, painful lesions on the cervix, vagina, and genital area 4. Diagnostic tests and findings c. Immunoglobulin G (IgG)–specific antibody (i.e., rubella-specific IgG to document prior infection) d. IgM-specific antibody (i.e., rubella-specific IgM to confirm recent infection; it becomes detectable approximately 1 week after onset of illness and persists for approximately 1 month). f. Hepatitis B surface antigen (HBsAg) is present in blood 30 to 50 days after exposure and 7 to 21 days before the onset of jaundice. g. Hepatitis B early antigen (HBeAg): the presence of early antigen denotes a high degree of infectivity. h. Enzyme-linked immunosorbent assay (ELISA) j. Serial sonography (to detect intrauterine growth restriction [IUGR]) 1. Encourage preconceptional counseling and advice on appropriate immunizations. 2. During prenatal visits, instruct the patient on good handwashing and cleaning of all kitchen surfaces, especially after handling raw meat; avoid eating insufficiently cooked meat; avoid contact with cat feces in litter boxes during pregnancy, and avoid gardening in soil contaminated with cat feces TABLE 20-2 Sexually Transmitted Infections Davies & Gibbs, 2008. p.340 Department of Health and Human Services, 2007, HIV/AIDS surveillance report Department of Health and Human Services, 2007, Sexually transmitted disease surveillance www.cdc.gov/hiv/resources/factsheets/us/html www.cdc.gov/hiv/topics/surveillance/incidence.html www.cdc.gov/hiv/topics/surveillance/resources/qa/surv_rep.html www.cdc.gov/std/stats07/trends.html www.cdc.gov/STD/STDfact-STDs&pregnancy.html www.marchofdimes.com/professionals/14332_1223.asp. www.marchofdimes.com/professionals/14332_1226.asp. 1. AIDS is caused by HIV, a virus passed from one person to another through blood and sexual contact. It was first recognized in 1981. The percentage of AIDS cases among female adults and adolescents (age >13 years) increased from 7% in 1985 to 27% in 2007 (Figure 20-1). The incidence of AIDS among female adults and adolescents rose steadily through 1993, when the AIDS surveillance case definition was expanded, and leveled off at approximately 13,000 AIDS cases each year from 1993 through 1996. In 1996, the incidence among women and adolescent girls began to decline, primarily because of the success of antiretroviral therapies. Cases have remained level since 2000 (www.cdc.gov/hiv/topics/surveillance/resources/slides/women/index.htm). 1. Agent: retrovirus (ribonucleic acid [RNA] virus) a. A virus containing RNA that has the ability to produce deoxyribonucleic acid (DNA) in its cellular host b. HIV destroys blood cells CD4 T cells (helper cells) that are crucial to the normal function of the human immune system; loss of these cells in people with HIV is an extremely powerful predictor of the development of AIDS. a. By exposure to blood and blood products or byproducts (1) Transfusions: This mode of transmission has dramatically decreased since screening of donated blood for HIV started in 1985. (2) Needle sharing among addicts c. Sexual contact factors that increase the rate of transmission include (Bernstein, 2007) (2) Sexual contact with an uncircumcised man (3) High number of sexual contacts (6) Presence of other sexually transmitted infections, particularly those that cause genital ulcers (herpes, syphilis, chancroid) d. Factors associated with increased perinatal HIV transmission (Bernstein, 2007) (3) Decreased maternal CD4 count (6) Blood exposure due to episiotomy, vaginal laceration, forceps delivery e. Highest concentrations of HIV have been isolated from blood, semen, and cerebrospinal fluid. f. HIV also is found in vaginal secretions, saliva, tears, breast milk, amniotic fluid, and urine; contact with saliva or tears has not been shown to result in infection. g. HIV is not transmitted through casual contact (e.g., water, food, environmental services). C Counseling and early diagnosis are recommended for the following: 1. Persons who consider themselves at risk for infection 2. Women of childbearing age who are at risk for infection 3. Persons attending STI clinics and drug abuse clinics 4. Women seeking family planning services 5. Tuberculosis patients and selected patients who received transfusions of blood and blood components between 1978 and 1985 6. The CDC operates a free telephone service that is available 24 hours a day, 7 days a week (800-342-2437); services for Spanish-speaking audiences and the deaf are also available. 1. In 2006 it was estimated that there were 56,300 new HIV infections (CDC, 2008). 2. Rates of reported AIDS cases (per 100,000) among female adults and adolescents are shown in Figure 20-2. The highest rates were found in the District of Columbia, U.S. Virgin Islands, Maryland, New York, and Florida. Rates were lowest in states in the Midwest. FIGURE 20-2 AIDS rates for female adults and adolescents reported in 2007—United States and dependent areas (www.cdc.gov/hiv/topics/surveillance/resources/slides/women/index.htm). 3. Today women account for more than one quarter of all new HIV/AIDS diagnoses. Women of color are especially affected by HIV infection and AIDS. For female adults and adolescents, in 2007, the AIDS diagnosis rate (AIDS cases per 100,000) for African-American females (39.8) was 22 times as high as the rate for white females (1.8). The estimated number of AIDS cases diagnosed among females in 2007 was similar for Hispanic/Latino and white females; however, the rate for Hispanic/Latino females (8.9) was nearly 5 times as high as the rate for white females (Figure 20-3). FIGURE 20-3 Estimated numbers of AIDS cases and rates for female adults and adolescents, by race/ethnicity 2007—50 states and the District of Columbia (www.cdc.gov/hiv/topics/surveillance/resources/slides/women/index.htm). 4. Among female adults and adolescents diagnosed with HIV/AIDS in 2007, 83% of the 10,977 HIV/AIDS cases were attributed to high-risk heterosexual contact, 16% to injection drug use, and 1% to other risk factors (Figure 20-4). j. History of blood transfusion before 1985 m. Cough and shortness of breath n. Recurrent or persistent vaginal infections p. Menstrual cycle disturbance (substance abuse and weight loss may cause oligomenorrhea and amenorrhea) q. Tuberculosis (TB); including association with persons with TB r. Intravenous (IV) drug abuse t. Sexual behavior: number of sexual partners, sexual orientation, contraceptive use, and specific sexual practices a. Elevated temperature (38.5° C [101.3° F]) d. Vaginitis caused by Candida, Trichomonas, and bacterial vaginosis that may not respond to therapy e. Presence of opportunistic infection (1) Pneumocystis jiroveci pneumonia (2) Kaposi’s sarcoma; reddish-blue or purple lesions on hard palate; rare in women with AIDS (4) Disseminated mycobacterial infections (10) Human papillomavirus (HPV) condyloma (13) Staphylococcus aureus; most common cause of bacterial skin disease (14) Diarrhea lasting greater than 1 month (15) Herpes zoster (shingles), involving at least two distinct episodes (17) Pelvic inflammatory disease, particularly if complicated by tubo-ovarian abscess c. Lack of social support and social isolation i. Possible lack of food, clothing, and basic childcare or health care a. The initial serologic screening test is ELISA, which is highly sensitive and inexpensive. If the ELISA is positive, repeat. After two positive ELISA assays, a Western blot or immunofluorescent antibody assay is performed for confirmation. (1) CBC with differential and platelet count (to monitor anemia, leukocytopenia, and thrombocytopenia) (2) Type, Rh factor, and antibody screen (5) Purified protein derivative (PPD) or radiograph (incidence of active TB is markedly elevated among HIV-infected patients) (6) Immunoglobulin levels are elevated. (7) Papanicolaou (Pap) smear: increased incidence of invasive cervical cancer (8) Gonorrhea, chlamydia cultures, and TORCH screen (9) Ultrasonography every trimester for IUGR, congenital abnormalities, and placental problems (10) Venereal Disease Research Laboratory (VDRL) testing (11) Urinalysis: may reveal proteinuria resulting from AIDS nephropathy (a) Elevated blood urea nitrogen (BUN) and creatinine levels may indicate presence of AIDS-related renal disease. (b) Abnormal liver enzymes may indicate liver infiltration by opportunistic infection. (c) Elevated total protein may indicate hypergammaglobulinemia.
Maternal Infections
INTRODUCTION
TORCH (TABLE 20-1)
CLINICAL PRACTICE
ACQUIRED IMMUNODEFICIENCY SYNDROME (TABLE 20-2)
CLINICAL PRACTICE
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Maternal Infections
Get Clinical Tree app for offline access