Lung Cancer
Non–Small Cell Lung Cancer
ETIOLOGY AND RISK FACTORS
• Tobacco is the primary risk factor. Long-term exposure to cigarette or cigar smoking is the major risk factor in development of lung cancer. Risk increases with number of years of smoking, number of cigarettes smoked, young age when smoking started, increased degree of inhalation, high tar and nicotine content, and use of unfiltered cigarettes. Risk does decrease after cessation. Second-hand smoke exposure contributes to a lesser extent.
• Environmental and occupational exposures to arsenic, benzene, radon, asbestos (especially in smokers), copper, silica, lead, diesel exhaust, chromium, and air pollution
• Radiation exposure from occupational, medical, and environmental sources
• Current and former smokers who take pharmacological doses of beta-carotene
• Scars from tuberculosis or inflammatory processes
• Although evidence is increasing that genetic factors can contribute to risk, no genetic abnormality has been found that causes lung cancer.
DIAGNOSTIC WORKUP
• History and physical examination to determine signs and symptoms of lung cancer and metastatic disease. Smoking and carcinogenic exposure history is important.
• Chest x-ray is probably the most helpful initial examination, but peripheral nodules must be 1 cm or larger to be visualized on radiographs. Other changes include lymphadenopathy, atelectasis, and pleural effusions.
• Computed tomographic (CT) scan of chest, abdomen, and pelvis to identify location of primary tumor and sites of metastatic disease (lymph nodes, liver, adrenal glands, bones)
• Biopsy under CT scan guidance, or bronchoscopy
• Mediastinoscopy to determine whether tumor has spread to mediastinal nodes if surgical resection is to be considered.
• Brain magnetic resonance imaging and bone scan looking for metastatic disease.
• Positron emission tomographic scans have become increasingly popular to find metastatic disease.
• Laboratory testing: alkaline phosphatase (bone/liver disease), calcium (hypercalcemia), complete blood cell count, kidney function, and liver function tests
• Pulmonary function tests to determine whether patient can tolerate removal of part of the lung
HISTOLOGY
There are three common histologies:
• Adenocarcinoma is the most common type (about 40%), and the incidence is increasing. Adenocarcinoma is associated with irritation and scarred areas. About one half of cases are not resectable at diagnosis. Includes subtypes of acinar, papillary, and bronchoalveolar
• Squamous carcinoma compromise about 30% of all lung cancers and are generally associated with smoking. These tend to be slow growing and therefore stay localized for a longer period. It usually presents as masses in large bronchi with local extension that may result in atelectasis and pneumonitis. When detected early, squamous carcinoma may be resectable and can be associated with longer survival.
• Large cell carcinoma represents about 10% to 15% of lung cancers. It is more undifferentiated and difficult to treat. It usually arises as peripheral nodules and metastasizes early, often to the gastrointestinal tract. It can be further classified into clear cell and giant cell, but they are treated the same.
CLINICAL STAGING
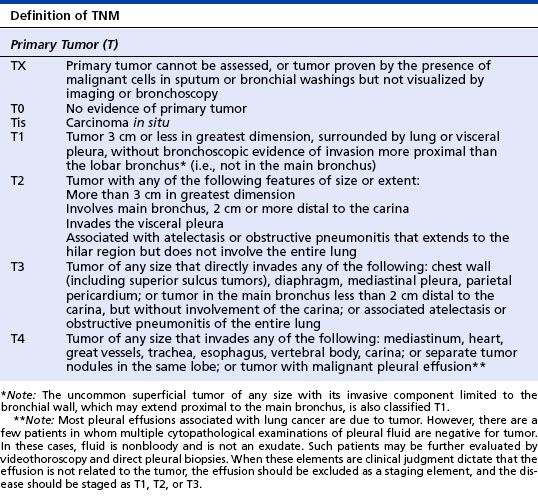
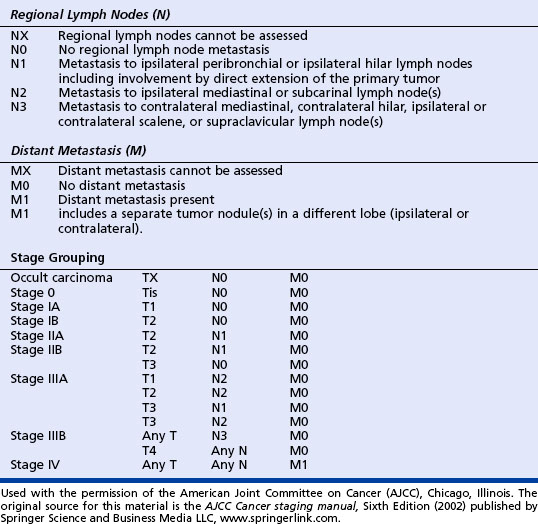
The purpose of staging is to determine how far the cancer has spread, so that appropriate treatment can be offered and a prognosis can be estimated. Patients can be divided into cases that are resectable and those that are not because only in the early stages can surgery be considered. NSCLC uses the TNM (tumor size, lymph nodes, and metastasis) system adopted by the American Joint Commission on Cancer. Histology or type of cancer is not a factor in staging. The stage of cancer determines the most appropriate treatment. See the table on page 118 for staging of lung cancer.
TREATMENT
When the cancer is localized and small (stages I, II, and some IIIA), surgery is usually the treatment of choice if the patient is a good surgical risk and can have a good quality of life after removal of that part of the lung (adequate pulmonary function tests). Surgical procedures include a wedge resection that removes small peripheral nodules (most conservative), segmentectomy that removes part of a lobe of the lung, lobectomy that removes a lobe of the lung (most common), or pneumonectomy that removes either the right or left lung. Only about 25% of patients with NSCLC are operable at diagnosis. Recent studies have shown that adjuvant chemotherapy after surgery in localized NSCLC can improve survival.
Most patients with NSLC will receive chemotherapy because many are initially seen with unresectable disease and 80% of those with resectable disease will have relapses. Treatment with chemotherapy alone for metastatic disease produces only moderate response rates (up to 30% with the newer drugs) and a median survival time of 25 to 30 weeks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree