L
Lactase deficiency
Description
Lactase deficiency is a condition in which the lactase enzyme that breaks down lactose into two simple sugars (glucose and galactose) is deficient or absent.
Primary lactase insufficiency is most commonly caused by genetic factors. Certain ethnic or racial groups, especially those with Asian or African ancestry, develop low lactase levels in childhood. Less common causes include low lactase levels resulting from premature birth and congenital lactase deficiency, a rare genetic disorder. Lactose malabsorption can also occur when conditions leading to bacterial overgrowth promote lactose fermentation in the small bowel, and when intestinal mucosal damage interferes with absorption (e.g., inflammatory bowel disease, celiac disease).
Clinical manifestations
Symptoms of lactose intolerance include bloating, flatulence, crampy abdominal pain, and diarrhea. They may occur within one-half hour to several hours after drinking a glass of milk or ingesting a milk product. Undigested lactose creates an osmotic action, pulling fluid into the small intestines, resulting in diarrhea.
Diagnostic studies
Many lactose-intolerant people are aware of their milk intolerance and avoid milk and milk products. Lactose intolerance is diagnosed by a lactose tolerance test, lactose hydrogen breath test, or genetic testing.
Nursing and collaborative management
Treatment consists of eliminating lactose from the diet by avoiding milk and milk products and/or replacing lactase with commercially available preparations. Teach the patient the importance of adherence to the diet.
Leiomyomas
Leiomyomas (uterine fibroids) are benign smooth muscle tumors within the uterus. They are the most common benign tumors of the female genital tract. By 50 years of age, 60% of all women will have had at least one uterine leiomyoma.
The cause of leiomyomas is unknown. They appear to depend on ovarian hormones because they grow slowly during the woman’s reproductive years and undergo atrophy after menopause.
A majority of women with leiomyomas do not have symptoms. Of the women who develop symptoms, the most common include abnormal uterine bleeding, pain, and symptoms associated with pelvic pressure. Pain is associated with an infection or twisting of the pedicle from which the tumor is growing.
Pressure on surrounding organs may result in rectal, bladder, and lower abdominal discomfort. Large tumors may cause a general enlargement of the lower abdomen. These tumors are sometimes associated with miscarriage and infertility.
Diagnosis is based on the characteristic pelvic findings of an enlarged uterus distorted by nodular masses.
Treatment depends on the symptoms, age of the patient, her desire to bear children, and the location and size of the tumor or tumors. If the symptoms are minimal, the provider may elect to monitor the patient closely for a time.
Leukemia
Description
Leukemia is a general term used to describe a group of malignant disorders affecting the blood and blood-forming tissues of the bone marrow, lymph system, and spleen. It results in an accumulation of dysfunctional cells because of a loss of regulation in cell division. Although leukemia is often thought of as a disease of children, the number of adults affected is 10 times that of children.
Regardless of the specific type, leukemia has no single cause. Most types of leukemia result from a combination of factors including genetic and environmental influences.
Classification
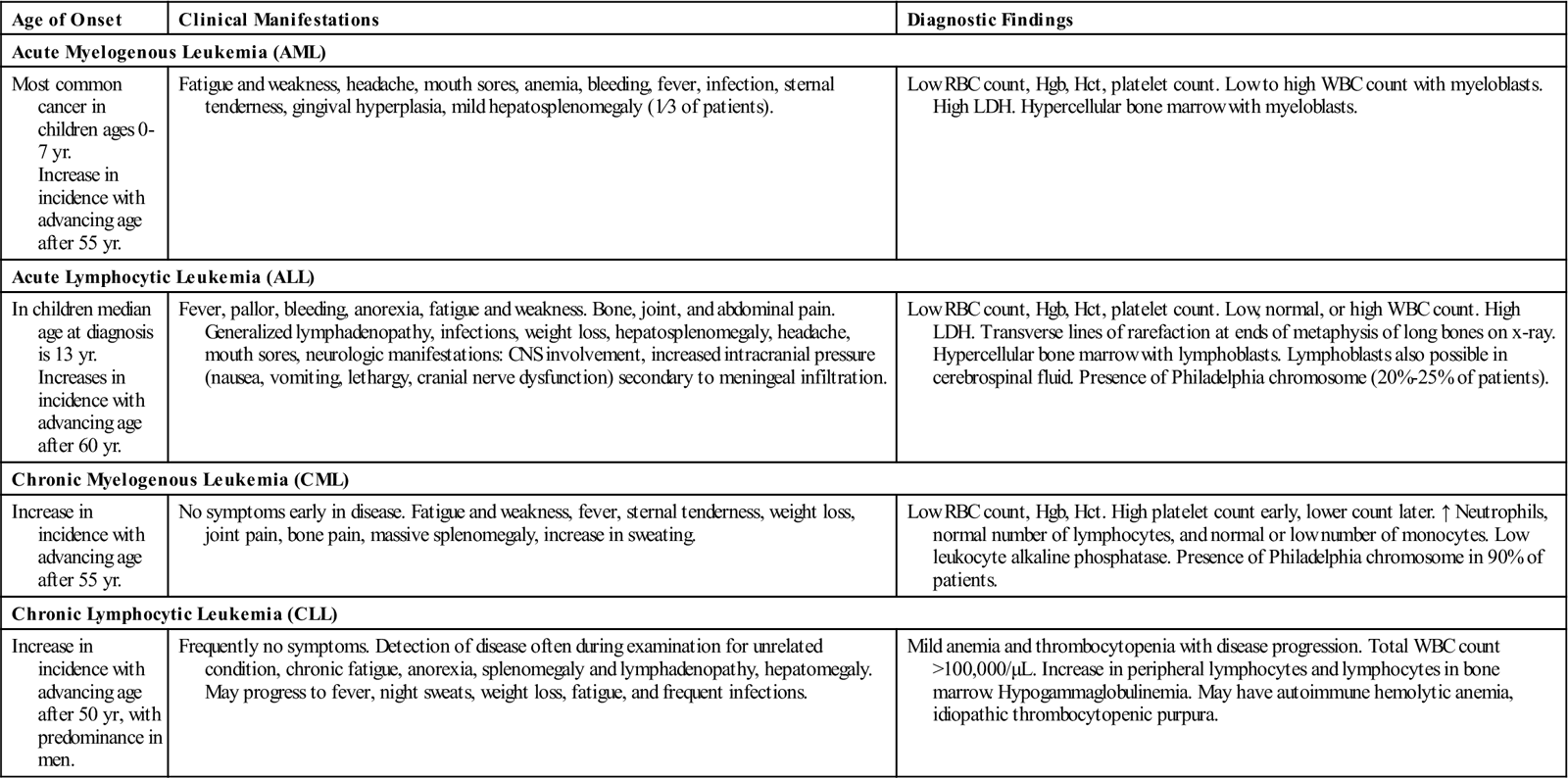
Leukemia can be classified based on acute versus chronic disease and on the type of WBC involved. By combining the acute and chronic categories with the cell type involved, four major types of leukemia can be identified. Table 58 summarizes the relative incidence and features of the four types of leukemia.
Table 58
| Age of Onset | Clinical Manifestations | Diagnostic Findings |
| Acute Myelogenous Leukemia (AML) | ||
| Most common cancer in children ages 0-7 yr. Increase in incidence with advancing age after 55 yr. | Fatigue and weakness, headache, mouth sores, anemia, bleeding, fever, infection, sternal tenderness, gingival hyperplasia, mild hepatosplenomegaly (1⁄3 of patients). | Low RBC count, Hgb, Hct, platelet count. Low to high WBC count with myeloblasts. High LDH. Hypercellular bone marrow with myeloblasts. |
| Acute Lymphocytic Leukemia (ALL) | ||
| In children median age at diagnosis is 13 yr. Increases in incidence with advancing age after 60 yr. | Fever, pallor, bleeding, anorexia, fatigue and weakness. Bone, joint, and abdominal pain. Generalized lymphadenopathy, infections, weight loss, hepatosplenomegaly, headache, mouth sores, neurologic manifestations: CNS involvement, increased intracranial pressure (nausea, vomiting, lethargy, cranial nerve dysfunction) secondary to meningeal infiltration. | Low RBC count, Hgb, Hct, platelet count. Low, normal, or high WBC count. High LDH. Transverse lines of rarefaction at ends of metaphysis of long bones on x-ray. Hypercellular bone marrow with lymphoblasts. Lymphoblasts also possible in cerebrospinal fluid. Presence of Philadelphia chromosome (20%-25% of patients). |
| Chronic Myelogenous Leukemia (CML) | ||
| Increase in incidence with advancing age after 55 yr. | No symptoms early in disease. Fatigue and weakness, fever, sternal tenderness, weight loss, joint pain, bone pain, massive splenomegaly, increase in sweating. | Low RBC count, Hgb, Hct. High platelet count early, lower count later. ↑ Neutrophils, normal number of lymphocytes, and normal or low number of monocytes. Low leukocyte alkaline phosphatase. Presence of Philadelphia chromosome in 90% of patients. |
| Chronic Lymphocytic Leukemia (CLL) | ||
| Increase in incidence with advancing age after 50 yr, with predominance in men. | Frequently no symptoms. Detection of disease often during examination for unrelated condition, chronic fatigue, anorexia, splenomegaly and lymphadenopathy, hepatomegaly. May progress to fever, night sweats, weight loss, fatigue, and frequent infections. | Mild anemia and thrombocytopenia with disease progression. Total WBC count >100,000/μL. Increase in peripheral lymphocytes and lymphocytes in bone marrow. Hypogammaglobulinemia. May have autoimmune hemolytic anemia, idiopathic thrombocytopenic purpura. |
Acute myelogenous leukemia (AML) represents only one fourth of all leukemias, but it makes up approximately 80% of the acute leukemias in adults. Its onset is often abrupt and dramatic. A patient may have serious infections and abnormal bleeding from the onset of the disease. AML is characterized by uncontrolled proliferation of myeloblasts, the precursors of granulocytes. There is hyperplasia of the bone marrow. Clinical manifestations are usually related to replacement of normal hematopoietic cells in the marrow by leukemic myeloblasts and, to a lesser extent, to infiltration of other organs and tissue.
Acute lymphocytic leukemia (ALL) is the most common type of leukemia in children and accounts for about 20% of acute leukemia cases in adults. In ALL, immature lymphocytes proliferate in the bone marrow; most are of B cell origin. Fever is present in the majority of patients at time of diagnosis. Signs and symptoms may appear abruptly with bleeding or fever, or they may be insidious with progressive weakness, fatigue, and bleeding tendencies.
Chronic myelogenous leukemia (CML) is caused by excessive development of mature neoplastic granulocytes in the bone marrow. CML usually has a chronic stable phase that lasts for several years, followed by the development of an acute aggressive phase (blastic phase).
Chronic lymphocytic leukemia (CLL) is the most common leukemia in adults and is characterized by the production and accumulation of functionally inactive but long-lived, small, mature-appearing lymphocytes. The B lymphocyte is usually involved. Lymph node enlargement (lymphadenopathy) is present throughout the body. Because CLL is usually a disease of older adults, treatment decisions must be made by considering disease progression and treatment of side effects. Many individuals in the early stages of CLL require no treatment. Others may be followed closely and receive treatment only when the disease progresses; approximately 30% will require immediate intervention at time of diagnosis.
Clinical manifestations
Although the manifestations of leukemia are varied, they relate to problems caused by bone marrow failure and the formation of leukemic infiltrates (see Table 58). The patient is predisposed to anemia, thrombocytopenia, and decreased number and function of WBCs.
Diagnostic studies
Collaborative care
Collaborative care first focuses on the initial goal of attaining remission.
■ Because cytotoxic chemotherapy is the mainstay of treatment for some patients, you must understand the principles of cancer chemotherapy, including cellular kinetics, the use of multiple drugs rather than single agents, and the cell cycle (see Chemotherapy, p. 694).
Chemotherapeutic agents used to treat leukemia vary. Combination chemotherapy is the mainstay of treatment for leukemia. The three purposes for using multiple drugs are to (1) decrease drug resistance, (2) minimize drug toxicity to the patient by using multiple drugs with varying toxicities, and (3) interrupt cell growth at multiple points in the cell cycle.
Hematopoietic stem cell transplantation (HSCT) is another type of therapy used for patients with different forms of leukemia. The goal of HSCT is to totally eliminate leukemia cells from the body using combinations of chemotherapy with or without total body radiation. This treatment also eradicates the patient’s hematopoietic stem cells, which are then replaced with those of a human leukocyte antigen (HLA)-matched sibling, with those of a volunteer donor (allogeneic) or an identical twin (syngeneic), or with the patient’s own (autologous) stem cells that were removed (harvested) before the intensive therapy. (See content on HSCT in Lewis et al., Medical-Surgical Nursing, ed. 9, pp. 667 to 668.)
The primary complications of patients with allogeneic HSCT are graft-versus-host disease (GVHD), relapse of leukemia (especially ALL), and infection (especially interstitial pneumonia). Because HSCT has serious associated risks, the patient must weigh the significant risks of treatment-related death or treatment failure (relapse) with the hope of cure.
Nursing management
Goals
The patient with leukemia will understand and cooperate with the treatment plan, experience minimal side effects and complications associated with both the disease and its treatment, and feel hopeful and supported during periods of treatment, relapse, or remission.
See nursing care plans for anemia (NCP 31-1, pp. 635 to 636, Lewis et al., Medical-Surgical Nursing, ed. 9), thrombocytopenia (eNCP 31-1, available on the website), and neutropenia (eNCP 31-2, available on the website).
Nursing diagnoses
Nursing diagnoses related to leukemia include those appropriate for anemia (see Anemia, pp. 635 to 636), thrombocytopenia (see Thrombocytopenic Purpura, pp. 653 to 654), and neutropenia (see content on neutropenia in Lewis et al., Medical-Surgical Nursing, ed. 9, pp. 660 to 663).
Nursing interventions
The nursing role during acute phases of leukemia is extremely challenging because the patient has many physical and psychosocial needs. As with other forms of cancer, the diagnosis of leukemia can evoke great fear and be equated with death.
Help the patient realize that although the future may be uncertain, one can have a meaningful quality of life while in remission or with disease control.
Families also need help in adjusting to the stress of the abrupt onset of serious illness and the losses imposed by the sick role. The diagnosis of leukemia often brings with it the need to make difficult decisions at a time of profound stress for the patient and family.
You are an important advocate in helping the patient and family understand the complexities of treatment decisions and manage the side effects and toxicities. A patient may require isolation or may need to temporarily geographically relocate to an appropriate treatment center. This situation can lead a patient to feel deserted and isolated at a time when support is most needed.
From a physical care perspective, you are challenged to make assessments and plan care to help the patient deal with the severe side effects of chemotherapy. The life-threatening results of bone marrow suppression (anemia, thrombocytopenia, neutropenia) require aggressive nursing interventions.
Review all drugs being administered. Assess laboratory data reflecting the effects of the drugs. Patient survival and comfort during aggressive chemotherapy are significantly affected by the quality of nursing care.
 Patient and caregiver teaching
Patient and caregiver teaching
Teach the patient and caregiver to understand the importance of continued diligence in disease management and the need for follow-up care.
Assistance may be needed to reestablish various relationships that are a part of the patient’s life.
Involving the patient in survivor networks, support groups, or services may help the patient to adapt to living with a life-threatening illness. Exploring community resources (e.g., American Cancer Society, Leukemia Society) may reduce the financial burden and feelings of dependence. Also provide the resources for spiritual support.
Liver cancer
Description
Primary liver cancer (hepatocellular carcinoma [HCC] or malignant hepatoma) is the fifth most common cancer in the world and the second most common cause of cancer death worldwide. It is the most common cause of death in patients with cirrhosis.
The incidence of HCC is rising in the United States because of the large number of patients infected with chronic hepatitis C. Cirrhosis caused by hepatitis C is the most common cause of HCC in the United States, followed by alcoholic cirrhosis. Other primary liver tumors are cholangiomas or bile duct cancers.
Metastatic carcinoma of the liver is more common than primary carcinoma. The liver is a common site of metastatic cancer growth because of its high rate of blood flow and extensive capillary network. Primary liver tumors commonly metastasize to the lung.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


