K
Kidney cancer
Kidney cancer arises from the cortex or pelvis (and calyces). Adenocarcinoma (renal cell carcinoma) is the most common type and is twice as frequent in men as in women. It is typically discovered when the person is 50 to 70 years old. The most significant risk factor is cigarette smoking. Other risk factors include family history (first-degree relatives), obesity, hypertension, and exposure to cadmium, asbestos, and gasoline.
Kidney cancer has no characteristic early symptoms; thus many patients go undiagnosed until the disease has significantly progressed. The most common manifestations are hematuria, flank pain, and a palpable mass in the flank or abdomen. Other symptoms include weight loss, fever, hypertension, and anemia. Local extension of kidney cancer into the renal vein and vena cava is common. The most common sites of metastases include lungs, liver, and long bones.
Nursing and collaborative management
Preventive measures, such as quitting smoking, maintaining a healthy weight, controlling BP, and reducing or avoiding exposure to toxins, can help reduce the incidence of kidney cancer. Patients in high-risk groups should be aware of their increased risk for kidney cancer. Teach them about early symptoms (e.g., hematuria, hypertension).
Kidney disease, chronic
Description
Chronic kidney disease (CKD) involves progressive, irreversible loss of kidney function. CKD can be defined as either the presence of kidney damage or a decreased glomerular filtration rate (GFR), less than 60 mL/min/1.73 m2, for more than 3 months. The classification of CKD is presented in Table 55. The last stage of kidney failure (end-stage kidney [renal] disease [ESKD]) occurs when the GFR is less than 15 mL/min. At this point, renal replacement therapy (dialysis or transplantation) is required.
Table 55
Stages of Chronic Kidney Disease
| Description | GFR (mL/min/1.73 m2) | Clinical Action Plan |
| Stage 1 | ||
| Kidney damage with normal or ↑ GFR | ≥90 | Diagnosis and treatmentCVD risk reduction Slow progression |
| Stage 2 | ||
| Kidney damage with mild ↓ GFR | 60-89 | Estimation of progression |
| Stage 3 | ||
| Moderate ↓ GFR | 30-59 | Evaluation and treatment of complications |
| Stage 4 | ||
| Severe ↓ GFR | 15-29 | Preparation for renal replacement therapy (dialysis, kidney transplant) |
| Stage 5 | ||
| Kidney failure | <15 (or dialysis) | Renal replacement therapy (if uremia present and patient desires treatment) |
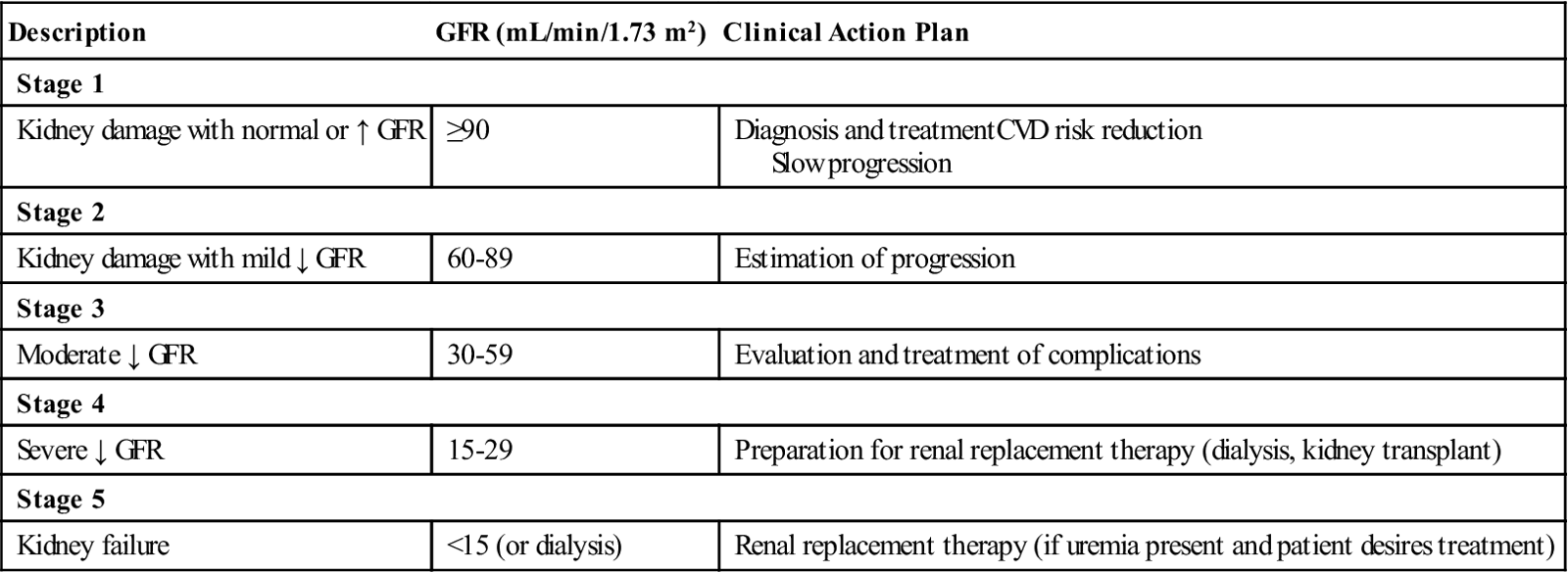
CVD, Cardiovascular disease; GFR, glomerular filtration rate.
Source: National Kidney Foundation. www.kidney.org/kidneydisease/aboutckd.cfm.
Although CKD has many causes, the leading causes of CKD are diabetes mellitus (about 50%) and hypertension (about 25%). One of every nine Americans has CKD. Over half a million Americans are receiving treatment (dialysis, transplant).
Because the kidneys are highly adaptive, kidney disease is often not recognized until there is considerable nephron loss. CKD is often underdiagnosed and undertreated because patients are often asymptomatic. It has been estimated that about 70% of people with CKD are unaware that they have the disease.
Prognosis and course of CKD are highly variable depending on the etiology, patient’s condition and age, and adequacy of health care. Some individuals live normal, active lives with compensated renal failure, whereas others may rapidly progress to ESKD.
Clinical manifestations
As kidney function deteriorates, every body system becomes affected. Manifestations are a result of retained substances including urea, creatinine, phenols, hormones, water, and electrolytes. Uremia is a syndrome in which kidney function declines to the point that symptoms develop in multiple body systems. It often occurs when the GFR is less than 10 mL/min (see Fig. 47-2 in Lewis et al., Medical-Surgical Nursing, ed. 9, p. 1109). Manifestations of uremia vary among patients according to the etiology of kidney disease, comorbid conditions, age, and degree of adherence to the prescribed medical regimen.
Additional systemic signs include pulmonary edema, constipation, peripheral neuropathy, osteomalacia, pruritus, infertility, and personality and behavior changes.
Diagnostic studies
■ Dipstick evaluation of urine is used to detect protein or microalbuminuria.
■ Urinalysis detects RBCs, WBCs, casts, and glucose.
■ BUN and serum creatinine are elevated.
■ GFR, obtained from 24-hour urine creatinine clearance measures, is decreased.
■ Hematocrit (Hct) and hemoglobin (Hgb) levels are decreased.
■ Ultrasound can be used to detect obstructions and the size of kidneys.
Collaborative care
The focus in CKD is to preserve existing kidney function, reduce the risks of cardiovascular disease (CVD), prevent complications, and provide for the patient’s comfort. It is important that patients with CKD receive appropriate follow-up and referral to a nephrologist early in the course of the disease. A focus on stages 1 through 4 (see Table 55) before the need for dialysis (stage 5) includes the control of hypertension, hyperparathyroid disease, anemia, hyperglycemia, and dyslipidemia. The following section focuses primarily on the drug and nutritional aspects of care.
■ Control and treatment of hypertension is discussed in Hypertension, pp. 332 to 333. It is recommended that the target BP be less than 130/80 mm Hg for patients with CKD and 125/75 for patients with significant proteinuria. Treatment of hypertension includes weight loss (if obese), therapeutic lifestyle changes (e.g., exercise, avoidance of alcohol, smoking cessation), diet recommendations, and administration of antihypertensive drugs. Drugs most commonly used include diuretics, β-adrenergic blockers, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin receptor blockers.
■ Exogenous erythropoietin (epoetin alfa [Epogen, Procrit]) is available to treat the anemia of CKD.
Many drugs are partially or totally excreted by the kidneys. Delayed and decreased elimination lead to an accumulation of drugs and the potential for drug toxicity. Drugs of particular concern include digoxin, diabetic agents (metformin, glyburide), antibiotics (e.g., vancomycin, gentamicin), and opioid medication.
Nutritional therapy
The current diet is designed to be as normal as possible to maintain good nutrition (see Table 47-10 for specific recommended restrictions in Lewis et al., Medical-Surgical Nursing, ed. 9, p. 1114). All patients with CKD should be referred to a dietitian for nutritional education and guidance. For CKD stages 1 to 4, many clinicians encourage a diet with normal protein intake. However, teach patients to avoid high-protein diets and supplements as they may overstress the diseased kidneys. For patients with malnutrition or inadequate caloric or protein intake, commercially prepared products that are high in protein but low in sodium and potassium are available (e.g., Nepro, Amin-Aid).
In addition to protein, nutritional therapy also includes the restriction of water, sodium, potassium, and phosphate (see Table 47-10 for specific recommended restrictions in Lewis et al., Medical-Surgical Nursing, ed. 9, p. 1114).
Nursing management
Goals
The patient with chronic kidney disease will demonstrate the knowledge and ability to comply with the therapeutic regimen, participate in decision making for the plan of care and future treatment modality, demonstrate effective coping strategies, and continue with activities of daily living (ADLs) within physiologic limitations.
Nursing diagnoses
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


