To facilitate improved outcomes, it is essential that members of the interprofessional team are aggressive with early mobility, interaction, and education for the patient with ischemic stroke. The interprofessional team caring for the patient with ischemic stroke is composed of health professionals representing medicine and surgery, nursing, physical medicine and rehabilitation, physical and occupational therapy, speech and language pathology, case management, social work, nutrition support, and pharmacy. Their understanding of the pathophysiology and etiology of ischemic stroke as well as patient risk factors and comorbidities is imperative to anticipating the course of treatment and plan of care. With the expansion of understanding of stroke pathology and treatment over the past three decades, there has never been more availability of evidence-based guidelines and education for physicians, nurses, and interprofessional team members specific to stroke care that is easily accessible. The challenge facing all stroke practitioners is consistently implementing evidence-based stroke care in an organized fashion for all stroke patients across the nation.
This chapter will review the epidemiology and pathophysiology of stroke, initial and ongoing patient management, and interprofessional care of the stroke patient. Additionally, the organization of stroke care including stroke quality measures and evidenced-based best practices for optimal outcomes and care coordination across the continuum of care are discussed. This chapter will also discuss clinical recommendations for stroke care that come from the most recent guidelines available in early 2014 published by the American Heart Association and recommendations of the Brain Attack Coalition (BAC).
Clinical Pearl: Stroke information is available at your fingertips. There are comprehensive applications (apps) for your smart phone or tablet that include scales for ischemic and hemorrhagic stroke.
 BACKGROUND
BACKGROUND
Stroke is the fourth leading cause of death in the United States. In 2010, 1 of every 19 deaths in the United States was from stroke. Each year, 795,000 people have strokes at a cost of $36.5 billion (Go et al., 2013). Of these, 610,000 are first strokes and 180,000 are recurrent strokes. Ischemic stroke is the most common type of stroke in the United States, comprising 87% of all strokes. Intracerebral hemorrhage (ICH) accounts for 10% of all strokes in the United States, and 3% are caused by subarachnoid hemorrhage (Go et al., 2013). Stroke carries a significant burden and is a disease that disproportionately impacts minority populations. Approximately 25% of patients who are 65 years of age and older will die within 1 year after their first stroke, and over 50% of patients who are 65 years of age and older will be dead within 5 years of their first stroke. Of patients between the ages of 45 and 64 years at the time of their first stroke, 14% of Caucasian men and 18% of Caucasian women will be dead at 1 year. Of African American patients having a first stroke between the ages of 45 and 64 years, 18% of men and 19% of women will be dead at 1 year. The death rate at 5 years is significantly higher for African American patients than white patients, with 40% of African American women versus 29% of Caucasian women and 41% of African American men versus 26% of Caucasian men dead within 5 years of their first stroke (Go et al., 2013). People living in the southeastern United States in the area known as the stroke belt have a 20% higher stroke mortality than the rest of the country. The number of adults between the ages of 20 and 54 years having strokes has increased, whereas a decline in other age groups has been noted. As the baby boomer population ages, it is anticipated that by 2030, an additional 3.4 million people will have had a stroke (Go et al., 2013). For additional information on stroke epidemiology and risk, refer to Chapter 1 on Stroke Epidemiology, Definition, Burden, and Prevention.
 PATHOPHYSIOLOGY
PATHOPHYSIOLOGY
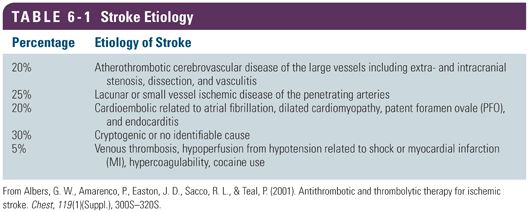
Ischemic stroke occurs through a number of mechanisms that all result in the blockage of an artery and subsequent cell death. Several common ischemic stroke subtypes are recognized, and the etiology of a patient’s stroke will determine how care is customized for the patient (Table 6-1).
Regardless of the etiology, during an acute ischemic stroke, 2 million neurons die every minute (Hickey, 2013). Neuronal death from ischemia is rapid because the brain cannot store glucose and without oxygen does not have any mechanism to create its own energy supply. The degree and duration of limited blood flow impact the brain cells differently. Oligemia is a reduction in the volume of blood flowing to the brain. The progression to ischemia occurs when the reduction in blood flow causes insufficient volume to perfuse the tissue. This results in infarction. This continuum creates a phenomenon known as the ischemic penumbra. The core of the infarct is the area of little to no perfusion that progresses to neuronal death and is considered unsalvageable. The penumbra is the area surrounding the core infarct that although is experiencing a limited supply of oxygen and glucose has several hours of potential viability should blood flow be restored.
A sudden onset of sustained ischemia is more detrimental to brain tissue than one either of short duration or one that progresses slowly. Initially, the brain attempts to compensate using cerebral autoregulatory mechanisms by vasodilating, expanding collateral vessels, and increasing the oxygen and glucose extraction from the blood. If compensatory mechanisms fail, and brain cells are without oxygenated blood flow, tissue becomes ischemic and will progress to cell death or infarct if uncorrected (Shah, 2002). The availability of collateral circulation greatly influences the individual response to ischemia. Collateral circulation refers to a network of small arterial vessels that develop to support the arterial perfusion of brain tissue (Liebeskind, 2003). Much remains unknown about collateral cerebral circulation. However, patients with chronic atherosclerosis and ischemia may have developed an extensive network of small artery growth that supports the blood perfusion to the chronically affected brain tissue. When an acute ischemic stroke occurs, recruitment of collateral circulation begins immediately (Liebeskind, 2003). However, the degree to which each individual develops a collateral network of circulation varies for reasons not well understood.
Ischemic stroke may occur in large or small cerebral arteries, although the mechanism of ischemic stroke is generally different in large versus small arteries. Large artery vessel disease impacts both the intra- and extracranial arteries through a process of atherosclerosis. Fatty streaks full of foam cells as well as circulating lipids turn to plaques in the artery walls. When plaque forms in the lining of the blood vessels, it causes narrowing of the lumen. Through an acute process often mediated by inflammation, the plaques may ulcerate and thrombose, developing an acute occlusion of the artery. Additionally, atherosclerotic plaque may calcify, increasing the risk for rupture. The plaque disrupts the smooth surface of the artery and can become sites for thrombus formation. The narrowing or even complete blockage of the artery lumen limits blood flow, resulting in ischemia in the brain tissue distal to the obstruction. In the smaller arterioles and capillaries, stroke is caused by tiny thrombi formed when there is a release of vasoactive enzymes from the endothelium, leukocytes, and platelets. The endothelial cells swell, reducing the patency of the vessel lumen. Therefore, larger artery strokes generally result from atherosclerotic processes, and small artery strokes generally result from chronic vessel disease resulting from hypertension and diabetes mellitus.
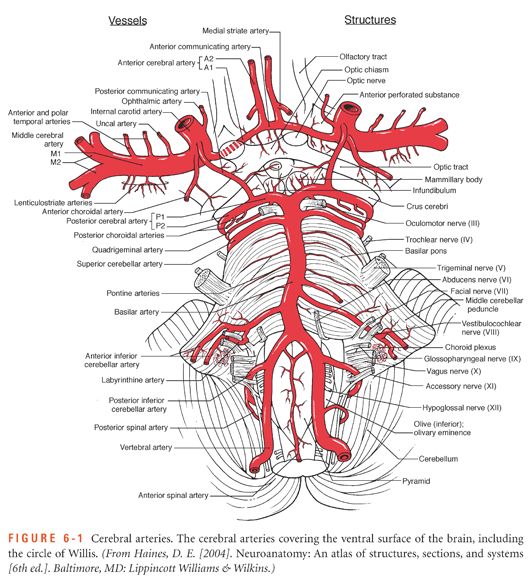
Emboli from plaque or vegetation in the heart or aorta may be the etiology of large vessel obstruction resulting in ischemic stroke. Embolic strokes most often affect the middle cerebral artery (MCA) because of its anatomic proximity to the carotid arteries. Eighty percent of the blood carried to the brain through the large arteries of the neck passes through the MCAs (Fig. 6-1 shows a detailed view of cerebral arteries). Therefore, when obstruction is noted in the large vessels of the brain, particularly the MCA, but also the posterior circulation, a full cardiac workup is indicated to identify the potential source for an embolism (Ustrell & Pellisé, 2010).
Regardless of the mechanism, within minutes of ischemia, the leukocytes that migrate to the area activate oxygen-free radicals, cytokines, and nitric acid. These mediators result in cellular and vessel changes that result in the vessels becoming more permeable, resulting in cerebral edema. This occurs within 1 hour of ischemia and is the beginning of cellular apoptosis (Shah, 2002). When brain tissue becomes ischemic, cell death and subsequent intracellular edema occurs. The edema compromises capillaries, which even further deprive the brain of blood and much needed oxygenation. The larger the stroke size and territory of infarct, the more likely the development of cerebral edema. Cerebral edema generally peaks 72 hours after initial injury. Therefore, the patient may worsen clinically in days 1 to 3 following the initial event.
Additional neurological injury may occur after the initial stroke event, resulting from vasospasm triggered by the presence of emboli in a large vessel as well as hemorrhagic transformation of the ischemic stroke. Infarcted brain tissue is friable and sensitive to pressure changes associated with fluctuations in perfusion. Hemorrhagic transformation of an ischemic stroke results from abnormal bleeding into the brain tissue in the region of ischemia and infarct. If the thrombus or embolus causing the ischemia or infarct migrate or dissolve either spontaneously or as a result of thrombolytics, there can be resulting reperfusion to an area of cerebral tissue no longer able to support circulation (Shah, 2002). Hemorrhagic conversion of ischemic strokes is discussed in greater detail in Chapter 7.
In small vessel strokes, the smaller arteries are involved, and the changes to the blood vessel are typically the outcome of thickening of the vessel lining as a result of lipohyalinosis. These infarcts lead to the lacuna seen on imaging and reported as lacunar infarcts. These infracts are typically found in the basal ganglia, thalamus, white matter of the internal capsule, and the pons (Hickey, 2013). Hypertension is the leading cause of small vessel ischemic strokes. Again, the impact of the stroke will depend on the size and territory of the infarct, which is based on where along the artery the occlusion occurs. In conclusion, the variables that impact the size of the infarct are collateral circulation available in the individual brain and the speed with which reperfusion of the penumbra is established.
Clinical Pearl: Only 50% of people have a complete circle of Willis joining the anterior and posterior circulation of the brain, which explains the variability of human response to strokes in similar territories due to availability of collateral circulation.
 STROKE LOCATION
STROKE LOCATION
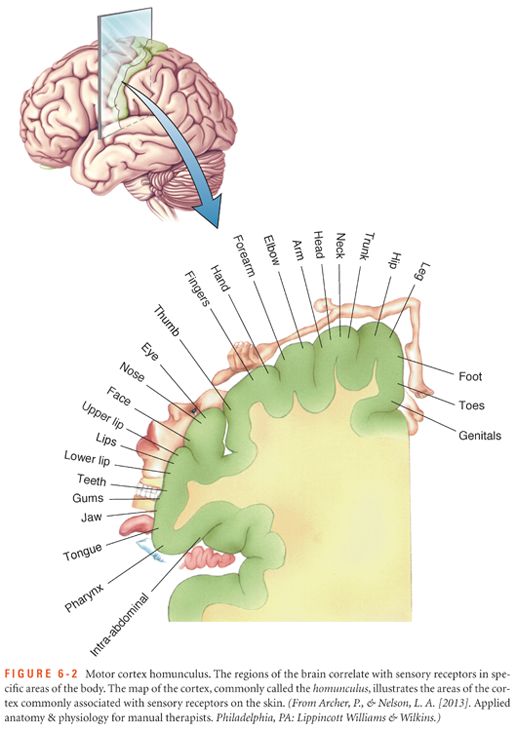
Localization of an ischemic stroke lesion involves recognizing syndromes or patterns of stroke based on location of affected arteries. This can help to predict or interpret the neurological deficits in acute stroke. The patient with stroke will experience symptoms based on which artery is occluded and how much brain tissue is without arterial circulation. Presenting symptoms can be used to predict complications, morbidity, and mortality in the stroke patient. In a left MCA stroke, the patient presents with aphasia, a left gaze preference, and right hemiplegia. In a right MCA stroke, the patient presents with a right gaze preference, left hemiplegia, and neglect. Neglect is the phenomenon that occurs when patients are unable to recognize, pay attention to, or acknowledge the existence of one side of the body. Anterior cerebral artery (ACA) strokes presents on the right side with apathy and left arm and leg weakness and on the left side with aphasia, apathy, and right arm and leg weakness. A patient presenting with a basilar artery stroke may exhibit quadriplegia or hemiplegia, locked-in syndrome, nystagmus, vertigo, diplopia, nausea and vomiting, or ataxia. The same symptoms without paralysis may indicate vertebral artery stroke (Fig. 6-2 shows the motor cortex homunculus).
Clinical Pearl: Approach patients from the unaffected side when they have homonymous hemianopsia (loss of vision in half of each visual field) to avoid startling the patients.
 THE CONTINUUM OF STROKE CARE
THE CONTINUUM OF STROKE CARE
The care of the patient with acute ischemic stroke is often categorized into three distinct phases based on the pathophysiology as discussed earlier and therapeutic goals of care (Summers et al., 2009). The hyperacute stroke period refers to the first several hours after an acute ischemic stroke. During the hyperacute phase of care, the interprofessional team is focused on efforts to treat the ischemic stroke and open the obstructed artery, when possible. The acute stroke phase generally begins 12 to 24 hours after the stroke begins and continues through the first several days after stroke. The goals of care during the acute phase of stroke include identifying the cause of the stroke, preventing and managing complications of the stroke, and initiating secondary prevention strategies to prevent another stroke event. The subacute phase of stroke care starts approximately 3 to 5 days after the stroke and continues for the first several weeks after the stroke. The goals of care during the subacute phase include the continued management of complications, continuation of secondary prevention measures to prevent another stroke event, aggressive rehabilitation to regain function, and reintegration of the stroke survivor back into the community (Summers et al., 2009).
 STROKE PREVENTION: BEGINNING THE CONTINUUM
STROKE PREVENTION: BEGINNING THE CONTINUUM
When a patient presents with acute ischemic stroke, clinicians employ a multitude of diagnostic tests to determine the source of the embolus or cause of the thrombus. Although viewed as comorbidities, these often preventable disease processes are the primary contributors to stroke. Up to 80% of strokes can be prevented (Go et al., 2013). Although age, sex, race, and family history cannot be changed, other risk factor modifications, with the guidance of a health care professional, can reduce stroke risk and increase awareness of signs and symptoms of acute stroke. High-impact risk factor modifications include controlling blood pressure, cholesterol, and blood glucose. Atrial fibrillation management, controlling diabetes, smoking cessation, maintenance of a healthy weight and body mass index, and eating a healthy diet can reduce risk of stroke. Stress, depression, oral contraceptive and hormone replacement therapy use, illegal drug use, and alcohol abuse can also contribute to stroke and are modifiable risk factors. Secondary prevention focuses on the management of modifiable risk factors through pharmaceutical measures, behavior modification, education, and community support and resources. See Chapter 1 for further discussion of preventive strategies.
 TRANSIENT ISCHEMIC ATTACK
TRANSIENT ISCHEMIC ATTACK
Patients may enter the hospital as direct admissions or through the emergency department after having had symptoms of stroke that subsequently resolved or are rapidly improving. A transient ischemic attack (TIA) occurs when blood flow to part of the brain is interrupted for a brief period of time (Easton et al., 2009). Since 2009, a tissue-based definition has been used for TIA pointing to transient deficit in neurological function caused by focal brain, spinal cord, or retinal ischemia without acute infarction. Prior to 2009, TIAs were thought to be defined by an absence of deficits or symptoms within 24 hours of onset. Newer imaging technology has demonstrated that one third of patients with traditionally resolving TIAs have actually had tissue infarction. Therefore, defining TIA based on time to tissue resolution alone results in an inadequate diagnosis (Easton et al., 2009).
A TIA is an indicator of significant risk for subsequent stroke. Ten percent to 15% of patients with TIA will go on to have a stroke within the following 90 days and half of those occur within 48 hours (Easton et al., 2009). Patients experiencing TIA are at high risk and need neurodiagnostic imaging, preferably diffusion magnetic resonance imaging (MRI), within 24 hours of symptom onset. Every effort should be made to determine the cause of ischemia and associated damage. Noninvasive imaging of the cervical vessels should be performed to assess for carotid stenosis and is typically done using magnetic resonance angiography (MRA) or carotid duplex. It is essential to uncover the mechanism that contributed to the event to determine the plan of care, the potential course of the disease process, and appropriate treatment. Blood work should mirror the workup including complete blood count, blood chemistry, prothrombin time (PT), partial thromboplastin time (PTT), and a fasting lipid profile. TIAs of unknown origin after diagnostic workup may need cardiac studies such as Holter monitoring, generally completed in the outpatient setting.
In the patient experiencing TIA, the ABCD2 score can predict the likelihood of a subsequent stroke and may be used to tailor care (Johnston et al., 2007). The score is determined by assigning a value to risk factors such as age 60 years and older, blood pressure, type and duration of neurological symptoms, and presence of diabetes. The score does not include findings from imaging studies. Some stroke programs use the ABCD2 score to determine the need for acute hospitalization versus follow-up in an outpatient setting within a few days of the TIA episode. Regardless of complete resolution of symptoms, if not admitted to the hospital, then patients should have diagnostic imaging scheduled as soon as possible after leaving the emergency department. Recently, a variety of TIA clinics have been designed for expeditious follow-up that allow for completion of MRI with diffusion-weighted imaging (DWI) and other neurodiagnostic studies including transcranial Doppler and carotid ultrasound. Clinic follow-up for TIA also allows an opportunity for risk factor review, planning, and teaching for medical management and consultation as needed for surgical treatment options.
 HYPERACUTE STROKE CARE TREATMENT
HYPERACUTE STROKE CARE TREATMENT
The hyperacute phase of stroke care begins with stroke symptom recognition by the patient or witness and mobilization to the hospital for acute stroke care. Emergency department (ED) care occurs faster if the patient is brought to the hospital by local emergency medical services (EMS) (Jauch et al., 2013). Once the stroke patient has arrived at the ED, care should be provided according to the recommendation in the “Guidelines for the Early Management of Patients with Acute Ischemic Stroke” from the American Heart Association (Jauch et al., 2013). The guidelines reference National Institute of Neurological Disorders and Stroke (NINDS) recommendations from a 1996 symposium outlining specific time frames for the delivery of key elements of care.
Initial Emergency Department Response
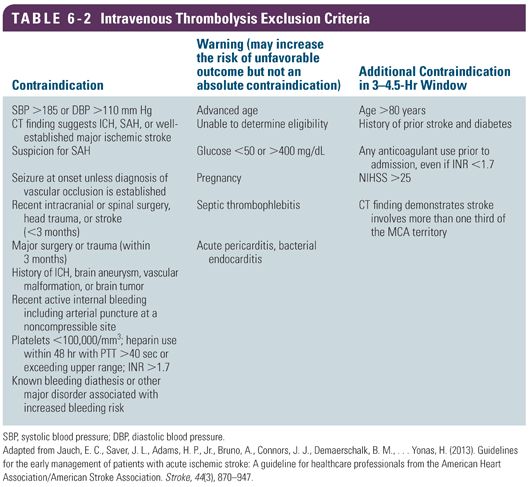
Quick recognition of acute stroke symptoms and mobilization of the interprofessional team is paramount to the rapid treatment of the stroke event. Recommendations are for a patient to see a physician in 10 minutes or less from arrival and stroke team activation within 15 minutes. A computed tomography (CT) scan of the head should occur in 25 minutes or less, with results reported within 45 minutes or less from hospital ED arrival. In eligible patients, intravenous tissue plasminogen activator (tPA) should be administered within 60 minutes or less from arrival (Table 6-2) (Jauch et al., 2013). The same goal parameters for assessment and treatment apply to inpatients exhibiting signs and symptoms of acute stroke. One successful model to achieve time-based interventions includes prehospital notification of an inbound stroke patient from EMS and activation of the interprofessional team from the EMS phone call  . The team converges on the patient location and provides rapid assessment, ordering of diagnostic studies, and acute interventions.
. The team converges on the patient location and provides rapid assessment, ordering of diagnostic studies, and acute interventions.
The urgent goal of ED treatment of a patient with new stroke symptoms is to identify the type of stroke (e.g., ischemic vs. hemorrhagic stroke) and evaluate the patient for urgent intervention, including intravenous fibrinolysis and endovascular procedures to open the occluded vessel. This process includes the rapid completion of neurological assessment, diagnostic imaging, and diagnostic testing including essential laboratory values. Within the aforementioned time frames, a thorough history and physical assessment should be conducted with a standardized neurological exam such as the National Institutes of Health Stroke Scale (NIHSS) (Meyer, Hemmen, Jackson, & Lyden, 2002). The assessment helps to confirm suspicion for stroke and rule out any disease processes that present like stroke. These are often referred to as stroke mimics. Stroke mimics include hypoglycemia, seizures, migraine, tumors, drug intoxication, and psychogenic causes. All potential stroke patients should have a noncontract CT scan of the brain or brain MRI. The noncontrast CT of the brain is sensitive for detection of ICH and subarachnoid hemorrhage (SAH) and will help the clinician determine if hemorrhage is causing stoke symptoms or if ischemic stroke is the expected mechanism. Many stroke centers are including CT angiography and CT perfusion emergently with or immediately following the initial CT imaging.
Initial Diagnostics and Blood Pressure Control
The ED workup should include the assessment of blood glucose, oxygen saturation, and blood work including serum electrolytes, renal function tests, a complete blood count, platelet count, activated partial thromboplastin time (aPTT), and PT with international normalized ratio (INR). An electrocardiogram (ECG) and cardiac markers should also be completed as acute myocardial infarction may occur with ischemic stroke. Blood pressure management in the first hour of stroke treatment will depend on whether the patient receives treatment with intravenous recombinant tissue plasminogen activator (rtPA). Seventy-seven percent of patients experiencing a first stroke have blood pressure reading greater than 140/90 mm Hg (Go et al., 2013). For an ischemic stroke patient not receiving rtPA, current guidelines recommend that blood pressure not be lowered during the first 24 hours of stroke unless it is greater than 220/120 mm Hg. If the blood pressure requires reduction in the first 24 hours, it may be lowered by 15% of the presenting elevated pressure with concurrent monitoring for any sign or symptoms of neurological deterioration (Jauch et al., 2013). In order to administer intravenous rtPA, the blood pressure must be gently lowered to less than 185/110 mm Hg using agents such as labetalol or nicardipine. Once given, the blood pressure must be maintained below 180/105 mm Hg to minimize the risk of intracranial hemorrhage. Frequent monitoring is necessary to maintain the blood pressure within the safe range. Blood pressure should be monitored with neurological checks every 15 minutes for 2 hours, then every 30 minutes for the next 6 hours, and hourly for the remainder of the 24 hours from the administration of intravenous rtPA. This is a class I, level of evidence B recommendation in the most recent iteration of the American Heart Association “Guidelines for the Early Management of Patients with Acute Ischemic Stroke” (Hacke et al., 2008; Jauch et al., 2013). If elevated during the first 24 hours, blood glucose should be managed to a target range of between 140 and 180 mm Hg.
Initial Treatment
Fibrinolytic Therapy
Background
Intravenous (IV) fibrinolysis with tPA is the only approved treatment for ischemic stroke. Stroke treatment with IV tPA was approved by the U.S. Food and Drug Administration (FDA) after the 1996 NINDS Stroke Trial demonstrated that treatment with IV tPA within 3 hours of stroke symptom onset was associated with significantly improved outcome when measured at 90 days (The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group, 1995). Patients who received IV tPA were more likely to have less global disability, improved measures of activities of daily living, and less neurological deficit 90 days after drug administration. Hemorrhage, particularly ICH, is the major complication associated with tPA treatment. ICH occurred in 6% of patients treated with tPA in the NINDS Stroke Trial compared to 0.6% who were not treated in the NINDS trial. There was no significant difference in mortality between the groups at 90 days or 1 year. The medication was approved for use by the FDA in 1996 and has become the standard of care for patients who are eligible for treatment (Jauch et al., 2013).
Since the approval of tPA for treatment of ischemic stroke, several trials and retrospective reviews have influenced fibrinolytic treatment. The European Cooperative Acute Stroke Study (ECASS III) trial demonstrated that tPA could be safely given to patients who present up to 4.5 hours after stroke symptom onset with a few additional exclusion parameters (Hacke et al., 2008). Patients receiving oral warfarin regardless of INR, patients with diabetes and a history of stroke, and patients older than age 80 years may be eligible for IV tPA if they present within 3 hours of stroke but should be excluded in the 3- to 4.5-hour time frame. The American Heart Association/American Stroke Association (AHA/ASA) endorsed the extended treatment window. However, the FDA has yet to approve the drug for usage in the extended window. Most organizations have embraced the extended time window and treat patients who present within 4.5 hours of stroke symptom onset.
Additionally, several retrospective case reviews have resulted in modifications to the original NINDS Stroke Trial inclusion and exclusion criteria for tPA treatment of patients who present within 3 hours of stroke treatment (Table 6-2). For example, the original trial excluded patients who had an NIHSS score higher than 4. However, experience with tPA treatment and stroke disease has revealed that patients with NIHSS less than 4 often experience debilitating strokes and often worsen after the first few hours of stroke. Therefore, most practitioners no longer consider this an absolute contraindication and treat patients with low NIHSS. As the inclusion and exclusion criteria continue to evolve, please refer to the most recent AHA/ASA clinical practice guideline for a detailed review of the literature.
Care during Fibrinolytic Administration
In the ED, the decision to administer IV rtPA must be made quickly because early and rapid treatment of ischemic stroke with IV tPA is associated with improved outcomes. Trials consistently demonstrate that IV tPA is most effective if given within the first 60 minutes of the acute stroke and has less benefit if treatment is delayed (Ahmed et al., 2010).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


