Chapter 38 Interventions in pregnancy, labour and birth
Learning outcomes for this chapter are:
1. To describe interventions in birth in relation to the normal physiology of birth
2. To explore the cascade of interventions in pregnancy, labour and birth, including the known benefits and harms of each intervention
3. To outline the aetiology of cerebral palsy
4. To explore the use of antenatal surveillance in pregnancy
5. To discuss the use of electronic fetal monitoring and the cardiotocograph in labour, including indications and contraindications in relation to current evidence and best practice
6. To discuss the reasons for induction of labour in relation to the current evidence and best practice models, and to identify the outcomes associated with induction of labour
7. To outline the use of augmentation of labour
8. To describe the implications of epidurals and combined spinal epidurals for labour and birth
9. To explore indications and outcomes of caesarean section deliveries.
combined spinal and epidural block
epidural analgesia and anaesthesia
fetal blood sampling, induction of labour
patient-controlled epidural analgesia
umbilical artery Doppler velocimetry
In both New Zealand and Australia, only about half of all childbearing women have spontaneous vaginal births. Even though we live in an age of evidence-informed practice, offering women many interventions for which the evidence is either non-existent or very weak has become almost routine. The difficulty for midwives is in separating practices based on sound evidence from those driven by opinion, authority, dogma, market or business principles, or other needs. This chapter will discuss common interventions in pregnancy, labour and birth in the light of findings from recently published research.
INTRODUCTION
As confusing as this may seem, there are several other factors worth considering. Physiologists claim that a woman should not be removed from her safe environment for labour because this will invariably result in inhibition of uterine contractions. We are advised that the safest way to help labouring women is to ‘respect nature and not to interfere with spontaneous events unless there is clear evidence that to do so would be beneficial’ (Naaktgeboren 1989). However, there is an opposing view that labour might be best avoided altogether and babies delivered routinely by abdominal operation (Hannah 2004).
AVOIDING UNNECESSARY INTERVENTION
• There must be a good reason for intervening in a woman’s labour. This means that you must be able to describe and support with good evidence the ‘clinical indications’ that require you to do anything that would interfere with the normal physiological process of labour and birth. Then you must weigh up the evidence to show that the intervention you are about to undertake will not cause more harm than good.
• By supporting a woman fully with appropriate and adequate information, you will find that many unnecessary interventions can be avoided.
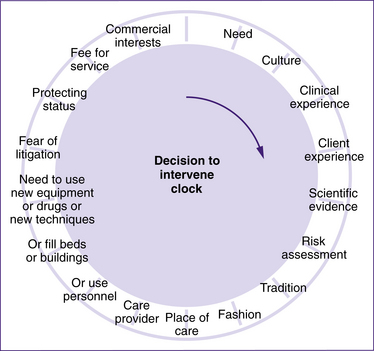
Much of the intervention that is routinely used in hospitals today evolved from the use of technology to ‘save’ mothers or babies when they were in distress during birth. ‘Distress’ itself is a subjective term and now there are parameters—or measurements—that enable us to see whether or not a woman may need medical intervention. Figure 38.1 shows an ‘intervention clock’, which was presented in the journal Birth in 1991. Even though it is around 20 years old, it still resonates for many of us. Twenty years ago, Iain Chalmers described the need to intervene in pregnancy and childbirth in terms of a ‘decision to intervene’ clock: ‘As you go around the clock … from unambiguous “need” at 1 o’clock to “commercial interests” at 11 o’clock, the factors that influence the decision to intervene become less and less defensible’ (Chalmers 1991, p 137). Several published studies demonstrate that there is still a need to question the effect of non-clinical factors on the rates of operative intervention during childbirth (Cary 1990; Roberts et al 2000; Shorten & Shorten 1999).
CEREBRAL PALSY
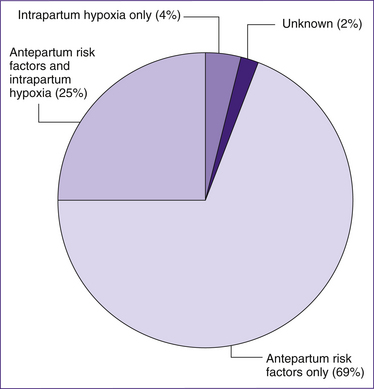
A major influence on the use of intervention was the belief until very recently that intervention in birth would be effective in preventing cerebral palsy (Blair & Stanley 1997). In some cases this may be so, but the birth prevalence of cerebral palsy in the developed world has not declined since the mid-1950s, in contrast to perinatal mortality. In developed countries, the majority of aetiological paths are likely to commence before labour and birth. Approximately 10% of cases are believed to now be causally associated with adverse intrapartum events. This is less than the proportion traditionally assumed to be due to intrapartum damage, and less than the proportion caused post-neonatally (after the baby is born) (Blair & Stanley 1997).
Cerebral palsy (CP) is a term of convenience applied to a group of motor disorders or motor impairment, stemming from a malfunction of the brain (rather than spinal cord or muscles). CP refers to brain malfunction that is non-progressive and manifests early in life. It is not a diagnosis, because it infers nothing about pathology, aetiology or prognosis. It is an umbrella term covering a wide range of cerebral disorders (Badawi et al 1998) used to describe chronic, non-progressive disorders appearing early in life, in which the defining symptoms are abnormal control of movement and posture. Cerebral palsy types are classified by the number of limbs involved (e.g. hemiplegia, quadriplegia or hemiparesis) and the type of movement disorder (e.g. spastic, athetoid/dyskinetic, akinetic, ataxic or mixed) (Hankins et al 2003).
Research suggests that spastic quadriplegia, and less often, dyskinetic CP, are the only types of CP associated with hypoxic intrapartum events but that neither of these types of CP are specific to intrapartum asphyxia. However, hemiplegic CP, spastic diplegia and ataxia are not associated with intrapartum asphyxia in term infants (Fahey & King 2005). CP affects two in 1000 live-born children. There are several antenatal factors, including preterm delivery, low birthweight, infection/inflammation, multiple gestations and other pregnancy complications, that have been associated with CP in both the preterm and term infant, with birth asphyxia playing a minor role. Due to the increasing survival of the very preterm and very-low-birthweight infant secondary to improvements in neonatal and obstetric care, the incidence of CP may be increasing (Longo & Hankins 2009).
• if the prevalence of CP has fallen with increasing use of obstetric and neonatal interventions aimed at reducing birth asphyxia
• if there is any evidence that CP is caused by birth asphyxia
• if there is any evidence that intrapartum fetal monitoring or caesarean section reduces the prevalence of CP.
The study found that:
• CP proportions are not falling in spite of significant increases in obstetric and neonatal interventions aimed at reducing asphyxia
CP proportions in low-birthweight infants are rising in most developed countries, coincident with increases in the neonatal survival of low-birthweight babies
• few cases of CP seem to be caused by birth asphyxia, and those that are may not have been preventable by obstetric care.
The study concluded that parents will continue to sue if obstetricians keep promising perfection from obstetric care in the face of 2.0–2.5 cases of CP per 1000 children born (Stanley & Blair 1991).
In pregnancy, the risk of CP is inversely associated with birthweight ratio (Blair & Stanley 1997; Palmer et al 1995). Researchers agree, however, that it is not low birthweight alone that increases the risk of CP, but rather birthweight in association with intrauterine growth restriction (Blair & Stanley 1997).
Primary antenatal causes of CP are thought to be:
• intrauterine viral infections (Stanley 1986 & English)
• iodine deficiency (Pharoah et al 1971)
• exposure to methyl mercury during pregnancy (Amin-Zaki et al 1979; Murakami 1972)
More recent suggestions support a causal role for chorioamnionitis (Leviton 1993).
Some causes of poor growth may interfere with brain development, or it may be that a previously brain-damaged fetus moves and grows less well (Blair & Stanley 1997). Multiple birth is also strongly associated with CP, and the risk increases with the number of fetuses. The rate of CP in twins of >2500 g birthweight is about four times that of singletons of >2500 g birthweight, suggesting aetiological factors specific to multiple gestation (Blair & Stanley 1997).
Intrapartum factors
Intrapartum factors producing hypoxia and/or trauma have traditionally been assumed to be the principal cause of CP. This has, no doubt, contributed to the increasing use of obstetric intervention and is responsible for malpractice suits being brought against perinatal caregivers (Tito 1995). The most frequently observed fetal heart rate patterns associated with CP are those with multiple late decelerations and decreased beat-to-beat variability. However, these patterns cannot be used to predict CP as they have a false-positive rate of 99% (Nelson et al 1996).
1. evidence of metabolic acidosis in fetal umbilical cord arterial blood obtained at birth (pH less than 7 and base deficit of 12 mmol/L or more)
2. early onset of severe or moderate neonatal encephalopathy in infants born at 34 or more weeks gestation
4. exclusion of other identifiable aetiologies, such as trauma, coagulation disorders, infectious conditions or genetic disorders (Hankin & Speer 2003).
Birth asphyxia is a poorly defined term relating to an exposure–response–outcome sequence initiated by hypoxia (Blair & Stanley 1993). Hypoxia is normal during vaginal delivery. For hypoxia to constitute asphyxia, it must have pathological effects. There is no definitive test for asphyxia (Blair & Stanley 1997). Recent studies suggest that:
• birth asphyxia may not be as important a cause of CP as previously assumed; it may sometimes constitute one step of a multifactorial cause
• neonatal signs associated with birth asphyxia may be early manifestations of CP from a variety of causes, of which birth asphyxia is only one
• most pathways to CP commence before birth
• infants with evidence of damaging birth asphyxia may not have fared better with alternative obstetric care (Blair & Stanley 1997; Stanley & Blair 1991).
The risk of developing CP appears to be elevated in infants:
Box 38.1 Birth asphyxia
• an umbilical blood gas of pH <7.0 or a base excess of ≥12 mmol/L
• an umbilical arterial lactate of >6 mmol/L
Box 38.2 Anti-D and cerebral palsy
A success story in the prevention of cerebral palsy
(Source: Blair & Stanley 1993)
Post-neonatal cerebral palsy
After birth, the causes of CP are known to be infective, anoxic or traumatic, with septicaemia and meningitis accounting for the majority, particularly in developing countries. In developed countries, there is a greater variety of post-neonatal aetiology, with trauma accounting for up to 24% (including motor vehicle accidents and non-accidental injury), and cerebrovascular accident and postoperative causes accounting for up to another 25%. Because these are the most aetiologically obvious, they may also be the most preventable (Blair & Stanley 1997).
INTERVENTIONS IN PREGNANCY
Assessing the wellbeing of the fetus
Interventions to assess the wellbeing of the baby while it is in utero are intended to provide obstetricians and mothers with the best information about the optimum time for birth. Intrauterine growth restriction (IUGR) affects approximately 10% of pregnancies and is associated with significant adverse perinatal outcomes. Severe IUGR results from multiple causes, such as genetic syndromes, aneuploidy or congenital infections, and is thought to be the result of a ‘compromised’ placenta. When a placenta is not functioning optimally, there is a risk that the fetus will suffer from a lack of oxygen (known as ‘placental respiratory failure’ or ‘fetal hypoxaemia’). Obstetricians believe that the inherent risks of delaying delivery of the severely growth-restricted fetus include those of worsening hypoxia, long-term neurodevelopmental complications and even perinatal death. Antenatal tests of fetal wellbeing are performed with the intention of identifying severely growth-restricted fetuses with early signs of compensatory failure and fetuses who are most at risk for adverse outcomes. However, the optimal antenatal test to guide obstetricians about the timing of delivery for the preterm fetus with severe IUGR remains uncertain.
Fetal movements
Fetal movements (FM) are one of the first signs of fetal life and are an indirect measure of central nervous system integrity and function. Because of this, FM are regarded as an expression of fetal wellbeing (Olesen & Svare 2004). Pregnant women usually sense FM from 18 to 20 weeks of gestation in a first pregnancy and at about 16 weeks of gestation in the second or subsequent pregnancy. As pregnancy proceeds, the weekly number of FM increases, peaking between 29 and 38 weeks of gestation (Olesen & Svare 2004). The movements are related to neuromuscular development and a normal metabolic state of the central nervous system of the fetus (Olesen & Svare 2004). A gradual decline in the total number of FM during the last trimester is suggested to be due to improved coordination and reduced amniotic fluid volume coupled with the increased fetal size (Rayburn 1990). On average, the fetus is active between 9% and 18% of the time in late pregnancy (Olesen & Svare 2004), or has movements of about 4 to 100 an hour (Mangesi & Hofmeyr 2004).
On ultrasound it can be observed that babies display chest wall movements that appear to be ‘breathing’ movements. During the last couple of months in a normal pregnancy, these ‘breathing’ movements may become irregular and have a frequency between 10 and 200 breaths/minute (Adelson et al 1999). The complete absence of breathing is observed in some normal fetuses for up to 122 minutes (fetal apnoea), which indicates that monitoring of respiratory movements may require a long observation time (Adelson et al 1999; Rayburn 1990). Women often report fetal hiccup movements that can be very intense, but there is no known pathology associated with this.
Methods of antenatal fetal surveillance
For each admission to hospital for birth in Australia, there are about 15–20 antenatal admissions (Adelson et al 1999). During these admissions, women very often undergo one or other of the following tests to ascertain fetal wellbeing.
Non-stress test (antenatal cardiotocography)
In the 1960s and 1970s, before the introduction of antenatal CTG, biochemical tests of placental or feto-placental function were widely used in high-risk pregnancies to try to predict, and thus avoid, adverse fetal outcome. Because the placenta provides nourishment for the baby in the uterus during pregnancy, it had been thought that testing women’s hormone levels during pregnancy might show how well the placenta was functioning and whether the baby was growing as would be expected. A review of trials in the Cochrane Database found evidence that measuring oestriol levels in high-risk pregnancies did not affect the outcome of the pregnancy (Neilson 2003). Trials of antenatal CTG or non-stress tests were conducted in the early 1980s when the antenatal CTG was being introduced and at a time when biochemical tests were the benchmark of fetal monitoring.
The Cochrane reviewers stated that:
It is not possible to judge whether the CTGs would have been interpreted and acted upon as they would today. There have been no trials in recent years despite the CTG being used extensively in modern practice … For high risk patients: A considerably larger study would be necessary to address the question of the effect of the antenatal CTG on perinatal mortality. Such a study is unlikely in the current environment, where the CTG has become an integral part of modern antenatal care. (Pattison & McCowan 2003)
on the basis of the information presented in this review the antenatal CTG has no significant effect on perinatal outcome or interventions such as early elective delivery. The suggested effect on reduced antenatal intervention is the main reason for the widespread current use of the CTG. All trials were conducted on high or intermediate risk pregnancies. Antenatal cardiotocography appeared to have no significant effect on perinatal mortality or morbidity. There was a trend to an increase in perinatal deaths in the cardiotocography group (odds ratio 2.85, 95% confidence interval 0.99 to 7.12). There was no increase in the incidence of interventions such as elective caesarean section or induction of labour. The one trial which examined an effect on antenatal patient management showed a significant reduction in hospital admissions and a reduction in inpatient stay in the cardiotocography group. (Pattison & McCowan 2003, p 3)
Fetal biophysical profile
Box 38.4 The antenatal CTG
• A reactive (normal) CTG is deemed by two accelerations exceeding 15 bpm, sustained for at least 15 seconds in a 20-minute period (Pattison & McCowan 2003).
Or
• The NST is considered reactive, or normal, if there are two or more FHR accelerations within a 20-minute period, with or without FM discernible by the woman (ACOG 2000).
Reduced variability and the presence of decelerations are abnormal.
Various scoring systems have been devised to classify the CTG. Initial observational studies have showed a strong correlation between the abnormal CTG and poor fetal outcome (Freeman et al 1982; Phelan 1981).
somewhat relative. Conditions in which testing is usually advised include the following:
• poorly controlled hyperthyroidism
• haemoglobinopathies such as thalassaemia
• systemic lupus erythematosus
Pregnancy-related conditions
• pregnancy-induced hypertension
• intrauterine growth restriction
• moderate to severe isoimmunisation
• previous fetal demise (unexplained or recurrent risk)
The biophysical profile (BPP) usually includes ultrasound monitoring of FM, fetal tone and fetal breathing, ultrasound assessment of amniotic fluid volume and assessment of FHR by electronic monitoring. The impact of the BPP on other interventions such as length of hospitalisation, serious short-term and long-term neonatal morbidity and parental satisfaction requires further evaluation. At present, there is insufficient evidence from randomised trials to support the use of BPP as a test of fetal wellbeing in high-risk pregnancies (Lalor et al 2008).
Umbilical artery Doppler velocimetry
Doppler ultrasonography is used to assess the flow velocity waveforms in the fetal umbilical artery. Some clinicians also observe the maternal vessels supplying the placental intervillous space and (especially since the development of colour-flow imaging) other fetal vessels, including aorta and cerebral arteries (Alfirevic & Neilson 1995). The study of the umbilical artery has remained the most widely used approach, however, because less-experienced operators can achieve highly reproducible results with simple, inexpensive continuous-wave equipment.
It became clear from observational data that many of the fetuses with extremely abnormal waveforms had a poor outcome (Bricker & Neilson 2000). An elevated uterine artery Doppler index may indicate increased spiral artery blood flow resistance on the maternal side of the placenta. In the baby the earliest sign of abnormal villous perfusion is a decrease in umbilical venous flow (Miller et al 2008). As the placenta extracts a fixed proportion of the nutrient stream (70% of glucose and 40% of oxygen supplied to the uterus), fetal nutrition is restricted to the surplus that remains after placental demands have been met. Even mild placental dysfunction may restrict nutrient transfer and blood flow to the fetus while placental nutrition is maintained (Miller et al 2008). A meta-analysis published in 1995 (Alfirevic & Neilson 1995) showed that assessment of umbilical artery waveforms by Doppler ultrasonography in high-risk pregnancies reduces the odds of perinatal death by 38% (CI 15%–55%) (Alfirevic & Neilson 1995).
A Cochrane Review of routine Doppler in pregnancy concluded that ‘Abnormal waveforms from Doppler ultrasound may indicate poor fetal prognosis. The use of Doppler ultrasound in high-risk pregnancies appears to improve a number of obstetric care outcomes and appears promising in helping to reduce perinatal deaths’ (Bricker & Neilson 2000). The review concludes, however, that although the study of umbilical artery waveforms helps identify the compromised fetus in ‘high-risk’ pregnancies, based on existing evidence, routine Doppler ultrasound in low-risk or unselected populations does not confer benefit on mother or baby. Future research should be powerful enough to address small changes in perinatal outcome, and should include evaluation of maternal psychological effects, long-term outcomes such as neurodevelopment, and issues of safety.
Doppler ultrasound uses sound waves to detect the movement of blood. It is used in pregnancy to study blood circulation in the baby, uterus and placenta. Using it in high-risk pregnancies where there is concern about the baby’s condition reduces the risk of the baby dying and the need for interventions around birth, such as caesarean section. However, its value as a screening tool in all pregnancies is limited by the rarity of complications, and the greater possibility of unnecessary intervention and adverse effects. A review of trials of routine Doppler ultrasound in pregnancy found that it does not improve the health of either the woman or the baby, and may do some harm (Bricker & Neilson 2000).
INTERVENTIONS IN LABOUR
Electronic fetal monitoring
Electronic fetal monitoring (EFM) is defined as ‘the use of electronic fetal heart-rate monitoring for the evaluation of fetal wellbeing in labour’ (NICE 2008). The word cardiotocography (CTG) translated means ‘a technical means of recording (-graphy) the fetal heartbeat (cardio-) and the uterine contractions (-toco-) during labour’. Thus, cardiotocography (sometimes known as electronic fetal
Table 38.1 Components of the biophysical profile
| Biophysical variable∗ | Normal score (score = 2) | Abnormal score (score = 0) |
|---|---|---|
| Fetal breathing movements | At least one episode of fetal breathing of ≥30 s duration | Absent fetal breathing, or no episode of ≥30 s duration |
| Gross fetal body movement | At least one episode of active extension with return to flexion of fetal limbs or trunk. Includes opening or closing of the hand | Slow extension with return to partial flexion or limb movement without flexion or absent fetal movement |
| Fetal heart rate | ||
| <26 weeks | At least two episodes of ≥10 beat accelerations of ≥10 s duration | Fewer than two episodes of accelerations and durations as specified |
| 26–36 weeks | At least two episodes of ≥10 beat accelerations of ≥15 s duration | |
| >36 weeks | At least two accelerations of ≥20 beat accelerations of ≥20 s duration | |
| Amniotic fluid volume | At least one amniotic fluid pocket of 2 × 2 cm in perpendicular plane | No amniotic fluid pocket of 2 × 2 cm in perpendicular plane |
∗ All parameters are examined in a 30-minute monitoring interval.
(Sources: Manning 1999; Preboth 2000)
The aim of CTG is to identify babies who may be short of oxygen (hypoxic), so that additional assessments of fetal wellbeing may be used or the baby may be delivered by caesarean section or instrumental vaginal birth (Alfirevic et al 2006). The technique allows detection and analysis of the fetal heart rate (via Doppler ultrasound (external transducers) or direct measurement with a fetal scalp electrode) and a semi-quantitative analysis of uterine muscle activity and contractions. Fetal heart rate pattern recognition, including the relationship between the uterine contractions and fetal heart rate decelerations, are fundamental to the use of continuous CTG monitoring. Algorithms have been developed to assess and record what is normal, what requires more careful attention and what is considered abnormal requiring immediate delivery of the baby (RCOG 2001). However, CTG traces are often interpreted differently by different caregivers (inter-observer variation) and even by the same caregiver interpreting the same record at different times (intra-observer variation) (Devane & Lalor 2005).
Continuous cardiotocography during labour is associated with a reduction in neonatal seizures, but no significant differences in cerebral palsy, infant mortality or other standard measures of neonatal wellbeing. However, continuous cardiotocography is associated with an increase in caesarean sections and instrumental vaginal births. The real challenge is how best to convey this uncertainty to women to enable them to make an informed choice without compromising the normality of labour. (Alfirevic et al 2006)
EFM was introduced with the aim of reducing perinatal mortality and cerebral palsy; however, systematic reviews of randomised controlled trials (RCTs) have not demonstrated their effectiveness to date (NICE 2007, 2008), and an increase in maternal intervention rates has been shown (NICE 2007, 2008).
• decisions relating to the use of admission CTG
• decisions relating to the use of EFM (both continuous and intermittent) or intermittent auscultation.
Admission CTG
The use of admission CTG in low-risk pregnancy is not recommended in any birth setting for women without identified risk factors and having a baby at term (37 to 41 weeks) (NICE 2007, p 39). The following statement is reproduced from the Royal Australian and New Zealand College of Obstetricians and Gynaecologists recommendations for the admission CTG (RANZCOG 2006).
The admission cardiotocogram is a short, usually 20 minute, recording of the fetal heart rate immediately after admission to the labour ward. The most commonly heard rationale or routine justification for the admission cardiotocography is that the uterine contractions of labour put stress on the placental circulation and therefore an abnormal tracing might indicate a deficiency and hence identify potential fetal compromise at an early enough stage to allow intervention. Furthermore, a normal admission cardiotocogram offers reassurance. However, the incidence of intrapartum fetal compromise is low in pregnancies that have been uncomplicated before the onset of labour. Thus, labour admission cardiotocography may represent unnecessary intervention. In such low risk cases, confirmation of a normal fetal heart rate by Doppler auscultation should be sufficient. (RANZCOG 2006)
The most important finding from an RCT of admission CTG by Mires et al (2001) was the increased rate of operative delivery in women who had admission CTG. Among women who were low-risk at admission, there was an absolute increase of 5.5% in operative delivery and 1.5% increase in caesarean sections. The increased use of continuous monitoring of FHR in labour in women who had admission CTG in this study is likely to be a contributing factor. This study has confirmed that among women with low-risk features at the onset of labour, the admission CTG is no better than Doppler auscultation of the fetal heart in identifying a potentially compromised fetus. Admission CTG was associated with increased obstetric intervention, including higher rates of operative delivery. Although caution is needed in generalising conclusions to the whole population, the results point to potential problems with admission CTG. These problems are likely to persist while difficulties remain in interpreting CTGs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree