Integrating Cultural Beliefs and Practices When Caring for Childbearing Women and Families
Lynn Clark Callister
Maria, a Mexican American woman having her first baby, attended a childbirth education class where the expectant fathers learned labor support techniques. She declined to lie on the floor surrounded by other men while her husband massaged her abdomen.
Hala, a Muslim Arabic woman experiencing her first labor, was attended by her mother and mother-in-law. As the labor slowly progressed and Hala began to be more uncomfortable, the two mothers alternated between offering her loving support, chastising her for acting like a child, and praying loudly that mother and baby will be safe from harm.
Nguyet, a primiparous Vietnamese immigrant, had been in the United States only a short time when she went into labor. She arrived at the birthing unit in active labor dilated to 5 cm. Nguyet and the father of the baby, Duc, spoke very limited English. Her labor was difficult, but she did not utter a sound. Duc entered the birthing room only when the nurses asked him to translate for Nguyet. After 20 hours of labor, a cesarean birth was performed. On the mother-baby unit, Nguyet cooperated with the instructions from the nurse to cough and deep breathe, but she became agitated when the nurse set up for a bed bath and began bathing her. When she was encouraged to walk, she shook her head and refused. She also refused the chilled apple juice the nurse brought to her. Because of abdominal distention and dehydration, a nasogastric tube was inserted, and intravenous fluids were restarted. No one could understand why she was so uncooperative.
Because of a nonreassuring fetal heart rate, Koua Khang needed an emergent cesarean birth. The nurse told her she would need to remove a nondescript white string bracelet from her wrist before surgery. Koua became hysterical, gesturing and trying to convey the message that the bracelet would protect her during the birth from evil spirits.
Michelle, a certified nurse midwife, cared for a Mexican immigrant mother who finally confided in her that during her postpartum hospitalization she went in the shower and turned on the water but was very careful not to get wet. She was following instructions from her nurse while trying to maintain her own cultural beliefs.
Mei Lin, a Chinese woman in graduate school in the United States, promised her mother she would follow traditional Asian practices after her son was born, including “doing the month” and subscribing to the hot/cold theory. Even though this woman was intellectually aware these practices had little scientific basis, she demonstrated her respect for her mother and her culture by honoring her mother’s request.
Sameena was having a scheduled cesarean birth. Her family had a tradition that the newborn be placed immediately in a blanket that had been in the family for generations, but were concerned that since it was a surgical birth, the tradition would not be followed. The nurses accommodated this cultural tradition, and the blanket was placed inside the hospital receiving blanket when her child was born. The grandmother was pleased and grateful.
Childbirth is a time of transition and social celebration in all cultures. A Wintu child living in Africa, in deference to his mother, refers to her as, “She whom I made into mother.” Culture also influences the experience of perinatal loss because the meaning of death and rituals surrounding death are culturally bound. Healthcare beliefs and health-seeking behaviors surrounding pregnancy, childbirth, and parenting are deeply rooted in cultural context. Culture is a set of behaviors, beliefs, and practices, a value system that is transmitted from one woman in a cultural group
to another (Lauderdale, 2007). It is more than skin color, language, or country of origin. Culture provides a framework within which women think, make decisions, and act. It is the essence of who a woman is. The extent to which a woman adheres to cultural practices, beliefs, and rituals is complex and depends on acculturation and assimilation into the dominant culture within the society, social support, length of time in the United States or Canada, generational ties, and linguistic preference. Even within individual cultural groups, there is tremendous heterogeneity. Although women may share a common birthplace or language, they do not always share the same cultural traditions (Moore, Moos, & Callister, 2010).
to another (Lauderdale, 2007). It is more than skin color, language, or country of origin. Culture provides a framework within which women think, make decisions, and act. It is the essence of who a woman is. The extent to which a woman adheres to cultural practices, beliefs, and rituals is complex and depends on acculturation and assimilation into the dominant culture within the society, social support, length of time in the United States or Canada, generational ties, and linguistic preference. Even within individual cultural groups, there is tremendous heterogeneity. Although women may share a common birthplace or language, they do not always share the same cultural traditions (Moore, Moos, & Callister, 2010).
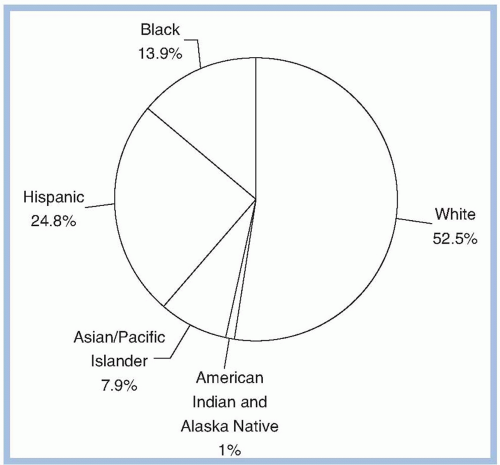
Diversity is a reality in the United States. Nurses provide care to immigrants, refugees, and women from almost everywhere in the world, many of whom are of childbearing age (Grewal, Bhagat, & Balneaves, 2008; McKeary & Newbold, 2010). More than 30% of the U.S. population now consists of individuals from culturally diverse groups other than non-Hispanic whites, whereas only 9% of registered nurses come from racial or ethnic minority backgrounds. It is projected that by the year 2050, minorities will account for more than 50% of the population of the United States. Each year, nearly 1 million immigrants come to the United States, half of whom are immigrant women of childbearing age. Since 1980, more than 200,000 refugees have resettled in the United States (U.S. Bureau of Population, 2008). One in every 12 U.S. residents is foreign born. Twenty-seven percent of women living in the United States are women of color. One of the challenges for healthcare in this century is that members of racial and ethnic minorities make up a disproportionately high percentage of persons living in poverty.
AFRICAN AMERICAN/BLACK
Geophagia (ingestion of soil, chalk, or clay) may be present during pregnancy
Strong extended family support
Matriarchal society
Present time orientation
May engage in folk practices (“granny,” “root doctor,” voodoo priest, spiritualist) depending on background
Tend to seek prenatal care after the first trimester
AMERICAN INDIAN AND NATIVE ALASKAN
Healthcare decision making by families/tribal leaders
Often stoic; don’t make eye contact, limit touch
Strong spiritual foundation
May utilize a medicine man or shaman
Present time orientation
ASIAN AMERICAN AND PACIFIC ISLANDER
Culturally and linguistically heterogeneous
Healthcare decision making by families
“Hot/cold” theory of illness (pregnancy considered a “hot” condition, except among Chinese women, who consider it a “cold” condition)
Asians are often stoic.
Strong extended family support
Asian fathers may choose not to attend the birth.
Chinese postpartum focus on “doing the month”
AAs have future orientation, PIs have present orientation
Asians have high respect for others.
Asians may utilize an acupuncturist/acupressurist, herbalist.
HISPANIC/LATINO
Healthcare decision making by families
Strong extended family support
Prenatal care may not be valued because pregnancy is a healthy state.
Enjoy strong extended family support
Fathers may choose not to attend the birth.
May use folk healers and Western medicine concurrently (curandero, espiritualista, yerbero)
Present time orientation
Believe in the “evil eye”
Postpartum maternal/newborn dyad vulnerable or delicate
WHITE/CAUCASIAN
Often considered a noncultural group
Value autonomy and personal decision making
Eastern European women avoid cutting or coloring hair during pregnancy.
Future time orientation
Focus on achievement
Poverty brings many challenges in healthcare delivery (U.S. Census Bureau [USCB], 2010; U.S. Department of Health and Human Services [USDHHS], 2010; USDHHS Office of Minority Health, 2010). Women and families in poverty can be considered a culture associated with health disparities and increased vulnerability in childbearing women.
Clinical examples in this chapter represent only a fraction of the possible cultural beliefs, practices, and behaviors the perinatal nurse may see in practice (Display 2-1). It is beyond the scope of this chapter to thoroughly discuss in detail each cultural group. Although generalizations are made about cultural groups, a stereotypical approach to the provision of perinatal nursing care is not appropriate. Cultural beliefs and practices are dynamic and evolving, requiring ongoing exploration (Douglas & Pacquaio, 2010). In any given culture, each generation of childbearing families perceives pregnancy, childbirth, and parenting differently. Each individual
woman should be treated as an individual who may or may not espouse specific cultural beliefs, practices, and behaviors.
woman should be treated as an individual who may or may not espouse specific cultural beliefs, practices, and behaviors.
Cultures are not limited to the obvious traditional ethnic or racial groups. Examples of other “cultures” include refugees and immigrants, women living in poverty, women who have experienced ritual circumcision, adolescent childbearing women, women with disabilities, and deeply religious women such as those espousing the beliefs of Jehovah’s Witnesses (Bircher, 2009; Braithwaite, Chichester, & Reid, 2010; Ogunleye, Shelton, Ireland, Glick, & Yeh, 2010; Wisdom et al., 2010). Perinatal nursing units may also be considered a culture, for some women a “foreign country” (Lewallen, 2011).
CULTURAL FRAMEWORKS AND CULTURAL ASSESSMENT TOOLS
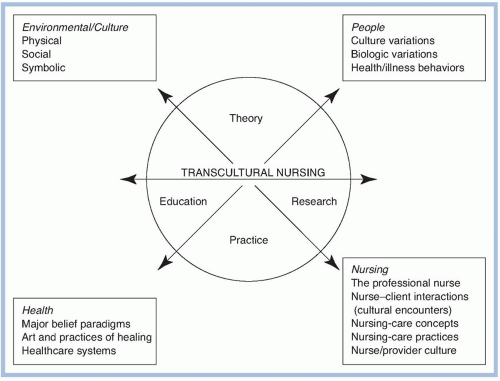
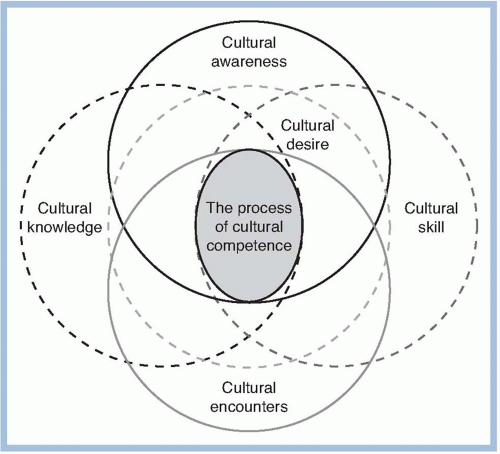
Cultural frameworks and cultural assessment tools have been developed to guide perinatal nursing practice. The Sunrise Model is based on culture care theory (Fig. 2-1) (Leininger & McFarland, 2006). The Transcultural Assessment Model (Giger, 2008) includes variables such as communication, space, social organization, time, environmental control, and biologic variations (Fig. 2-2). Others have identified the dimensions of culture, including values, world-view, disease etiology, time orientation, personal space orientation and touch, family organization, and power structure (Purnell & Paulanka, 2011). The Transcultural Nursing Model is illustrated in Figure 2-3 (Andrews & Boyle, 2007). Mattson (2011) has conceptualized specific ethnocultural considerations in caring for childbearing women (Fig. 2-4). Four assumptions define the influence culture has on pregnancy, childbirth, and parenting (Display 2-2). Models should focus on the person, the processes, the environment, and the outcomes.
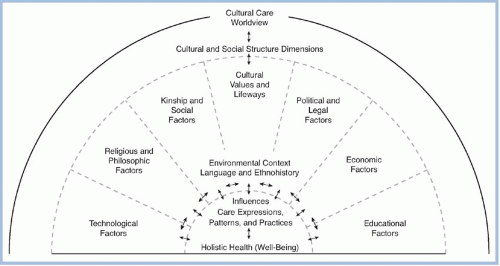 FIGURE 2-1. The Sunrise Model. (From Leininger, M., & McFarland, M. R. [2006]. Cultural Care Diversity and Universality: A Worldwide Nursing Theory [2nd ed.]. Sudbury, MA: Jones & Bartlett.) |
CULTURAL COMPETENCE
The process of cultural competence in the delivery of healthcare includes cultural awareness, skills, encounters, and knowledge (Campinha-Bacote, 1994). Cultural competence is more than a nicety in healthcare. Cultural competence has become imperative because of increasing health disparities and population diversity; the competitive healthcare market; federal regulations on discrimination; complex legislative, regulatory, and accreditation requirements; and our litigious society (deChesnay, Wharton, & Pamp, 2005; Joint Commission for Accreditation of Healthcare Organizations, 2010; Rorie, 2008) (Fig. 2-5).
Acculturation is a complex variable that is challenging to measure, and current measures need to be refined (Beck, Froman, & Bernal, 2005). Acculturation can be at a cultural or group level and a psychological or individual level (Beck, 2006; Gorman, Madlensky, Jackson, Ganiats, & Boles, 2007;
Huang, Appel, & Ai, 2011). The General Acculturation Index scale can be used to assess level of acculturation, and it includes items such as written and spoken language, the country where the childhood was spent, the current circle of friends, and pride in cultural background (Balcazar, Peterson, & Krull, 1997). Other instruments include the Short Acculturation Scale, the Acculturation Rating Scale for Mexican Americans (ARSMA), the ARSMA II, and the Bidimensional Acculturation Scale for Hispanics (Beck, 2006). A framework for acculturation has been identified by Berry (1980). Outcomes include assimilation, the establishment of relationships in the host society made at the expense of the patient’s native culture; integration, in which cultural identity is retained and new relationships are established in the host society; rejection, in which one retains cultural identity and rejects the host society; and deculturation, in which one values neither. Nurses will encounter immigrant women who fall into each of these categories of acculturation.
Huang, Appel, & Ai, 2011). The General Acculturation Index scale can be used to assess level of acculturation, and it includes items such as written and spoken language, the country where the childhood was spent, the current circle of friends, and pride in cultural background (Balcazar, Peterson, & Krull, 1997). Other instruments include the Short Acculturation Scale, the Acculturation Rating Scale for Mexican Americans (ARSMA), the ARSMA II, and the Bidimensional Acculturation Scale for Hispanics (Beck, 2006). A framework for acculturation has been identified by Berry (1980). Outcomes include assimilation, the establishment of relationships in the host society made at the expense of the patient’s native culture; integration, in which cultural identity is retained and new relationships are established in the host society; rejection, in which one retains cultural identity and rejects the host society; and deculturation, in which one values neither. Nurses will encounter immigrant women who fall into each of these categories of acculturation.
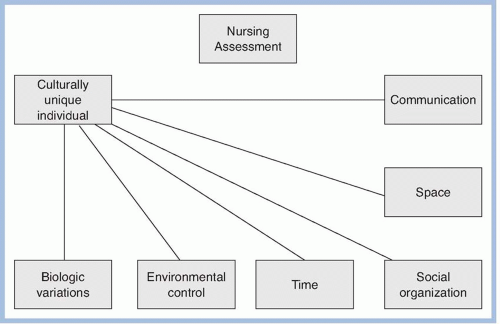 FIGURE 2-2. Transcultural model. (From Giger, J. N. [2007]. Transcultural Nursing: Assessment and Intervention [5th ed.] St. Louis, MO: Mosby-Year Book.) |
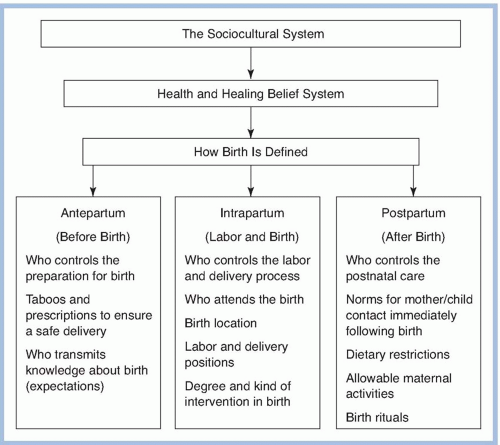 FIGURE 2-4. The sociocultural system, health and healing belief system, and how birth is defined. (From Mattson, S. [2011]. Ethnocultural considerations in the childbearing period. In S. Mattson & J. E. Smith [Eds.]. Core curriculum for maternal-newborn nursing [4th ed.] Philadelphia: Saunders.) |
What constitutes a positive and satisfying birth experience varies from one culture to another (Amoros, Callister, & Sarkisyan, 2010; Callister, Holt, & Kuhre, 2010; Callister, Corbett, Reed, Tomao, & Thornton, 2010; Callister et al., 2007; Callister, Eads, Diehl, & See, 2011; Corbett & Callister, 2012; Johnson, Callister, Beckstrand, & Freeborn, 2007; Wilkinson & Callister, 2010). For example, within the Japanese culture, there is the belief in a process called “education of the unborn.” A happy mother is thought to ensure joy and good fortune because the unborn child learns, communicates, and responds in utero. The individual personality is formed before birth. Such a belief about the fetus is reflected in many cultures, with concern during pregnancy about evil spirits and birthmarks. Other cultural considerations include fertility rites and beliefs about what determines the gender of the unborn child.
Within the framework of the moral and value system, cultural groups have specific attitudes toward childbearing and the meaning of the birth experience.
Within the framework of the ceremonial and ritual system, cultural groups have specific practices associated with childbearing.
Within the framework of the kinship system, cultural groups prescribe gender-related roles for childbearing.
Within the framework of the knowledge and belief system, cultural groups influence normative behavior in childbearing and the pain experience of childbirth.
From Callister, L. C. (1995). Cultural meanings of childbirth. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 24(4), 327-331.
Rich meaning may be created by women espousing traditional religious beliefs and may also influence the promotion of healthy behaviors (Callister & Khalaf, 2010; Lemon, 2006; Murray & Huelsman, 2009; Page, Ellison, & Lee, 2009; Yosef, 2008). An Orthodox Jewish mother gives silent thanks in the ancient words of the Psalms following the birth of her firstborn son. She believes that by birthing a son, she has fulfilled the reason for her creation in obedience to rabbinical law. The creation of life and giving birth represent obedience to religious law and the spiritual dimensions of the human experience.
Giving birth is a significant life event, a reflection of a woman’s personal values about childbearing and child rearing, and the expression and symbolic actualization of the union of the parents. For Muslim women, giving birth fulfills the scriptural injunctions recorded in the Quran. Muslim women may be asked soon after getting married, “Do you save anything inside your abdomen?” Meaning, “Are you pregnant yet?” Pregnancy in a traditional Asian family is referred to as a woman having “happiness in her body.” In Latin America, if you were to ask an expectant mother when her baby is due, the direct translation from Spanish to English is, “When are you going to give light?”
PRACTICES ASSOCIATED WITH CHILDBEARING
There are many diverse cultural rituals, customs, and beliefs associated with childbearing. American Indian mothers believe tying knots or weaving will cause birth complications associated with cord accidents. Navajo expectant mothers do not choose a name or make a cradleboard because doing so may be detrimental to the well-being of the newborn. Arabic Muslim women do not prepare for the baby in advance (e.g., no baby showers, layette accumulation, or naming the unborn child) because such planning has the potential for defying the will of Allah regarding pregnancy outcomes. Similarly, Eastern European women do not make prenatal preparations for the newborn, believing such actions would create bad luck. Filipino women believe that daily bathing and frequent shampoos during pregnancy contribute to having a clean baby. Asian American women may not disclose their pregnancy until the 120th day, when it is believed the soul enters the fetus. In many cultures, girls are socialized early about childbearing. They may witness childbirth or be present when other women repeat their birth stories, especially extended female family members. In the Sudan, a pregnant woman is honored in a special ceremony, as extended female family members rub her belly with millet porridge, a symbol of regeneration, empowering her to give birth. Because of the importance of preserving modesty, Southeast Asian women tie a sheet around their bodies like a sarong during labor and express a preference to squat while giving birth. An Italian maternal grandmother may request permission to give her newborn grandson his first bath. After the bath, she dresses him in fine, white silk clothing that she stitched by hand for this momentous occasion. When women in Bali hear the first cries of a newborn, they lavish the new mother with gifts such as dolls, fruit, flowers, or incense to bless, honor, purify, and protect the new child.
The placenta is called “el compañero” in Spanish, translated to mean, “the companion of the child.” There are a variety of cultural rituals associated with the disposal of the placenta, including having it dried, burned, or buried in a specific way. Although disposing of the placenta must meet with standard infection control precautions, individual family preferences should be honored as much as possible.
A variety of cultural practices influence postpartum and newborn care. Laotian women stay home the first postpartum month near a fire or heater in an effort to “dry up the womb.” The traditional postpartum diet for Korean women includes a soup made from beef broth and seaweed that is believed to cleanse the body of lochia and increase breast milk production. In Navajo tradition, a family banquet is prepared following the baby’s first laugh because this touches the hearts of all those who surround the baby.
Care of the newborn’s umbilical cord includes the use of a binder or belly band, the application of oil, or cord clamping, and then sterile excision. A Southeast Asian woman may fail to bring her newborn to the pediatrician during the first month after birth because this is considered to be a time for confinement and rest.
Postpartum cultural rituals are important for women of different cultures. Culturally diverse women experience postpartum depression, with an increased risk related to the gender of the child because in some societies male children are more highly valued (Callister, Beckstrand, & Corbett, 2010; Lau & Wong, 2008b).
GENDER ROLES
Many cultural groups show strong preference for a son. For example, according to Confucian tradition, only a son can perform the crucial rites of ancestor worship. A woman’s status is closely tied to her ability to produce a son in many cultures.
A Mexican immigrant woman may prefer that her mother or sister be present during her childbirth, rather than the father of her child. In some cultures, fathers may prefer to remain in the waiting room until after the birth. Vietnamese fathers rarely participate in the birth of their children. Only after the newborn is bathed and dressed may the father see him or her. In cultures
in which the husband’s presence during birth is not thought to be appropriate, nurses should not assume this denotes lack of paternal involvement and support.
in which the husband’s presence during birth is not thought to be appropriate, nurses should not assume this denotes lack of paternal involvement and support.
Modesty laws and the law of family purity found in the Torah prohibit the Orthodox Jewish husband from observing his wife when she is immodestly exposed and from touching her when there is vaginal bleeding. Depending on the specific religious sect, observance of the law varies from the onset of labor or bloody show to complete cervical dilation. Jewish husbands present at birth stand at the head of the birthing bed or behind a curtain in the room and do not observe the birth or touch their wives. Although cultural factors may limit a husband’s ability to physically support or coach his wife during labor and birth, Jewish women still feel supported. Husbands praying, reading Psalms, and consulting with the rabbi represent significant and active support to these women (Noble, Engelhardt, Newsome-Wicks, & Woloski-Wruble, 2009; Noble, 2009; Zauderer, 2009).
CHILDBIRTH PAIN AND CULTURE
A major pain experience unique to women is that associated with giving birth. Many cultural differences related to the perception of childbirth pain have been identified (Callister, 2011). Some women feel that pain is a natural part of childbirth and that the pain experience provides opportunity for important and powerful growth. Others see childbirth pain as no different from the pain of an illness or injury; that it is inhumane and unnecessary to suffer.
Words used to describe the pain associated with childbirth vary. Labor pain has been described as horrible to excruciating, episiotomy pain described as discomforting and distressing, and postpartum pain described as mild to very uncomfortable. Korean women described pain with words such as “felt like dying” or the “the sky was turning yellow,” or the sense of “tearing apart.” Mexican American women view pain as a physical experience, composed of personal, social, and spiritual dimensions. Scandinavian women demonstrate a high level of resilience and hardiness when giving birth, as do Australian women. One Australian woman viewed birth as symbolic of the challenges of life: “[Giving birth] makes you more resilient. You know you are able to handle things that you didn’t think you could. I think it gives you strength because you know if you can through that, you can cope with a lot of other things” (Callister, Holt, et al., 2010, p. 113). Women’s perceptions of personal control have been found to positively influence their satisfaction with pain management during childbirth.
Pain behaviors also are culturally bound. Some Hispanic laboring women may moan in a rhythmic way and rub their thighs or abdomen to manage the pain. During labor, Haitian women are reluctant to accept pain medication and instead use massage, movement, and position changes to increase comfort. Filipino women believe that noise and activity around them during labor increases labor pain. African American women are more vocally expressive of pain. American Indian women are often stoic, using meditation, self-control, and traditional herbs to manage pain. Puerto Rican women are often emotive in labor, expressing their pain vocally. There is disparity between the estimation of labor pain by caregivers and the pain the women reported they were experiencing. The Coping with Labor Algorithm is proving helpful in assessing pain in laboring women rather than use of the traditional pain scale (Roberts, Gulliver, Fisher, & Cloyes, 2010).
MAJOR CULTURAL GROUPS
The major cultural groups in the United States include African Americans/blacks (AA/B), American Indian/Alaska Native (AI/AN), Asian American/Pacific Islander (AA/PI), Hispanic/Latino (H/L), and white/Caucasian (W/C). Designation in one of these five categories is not equated with within-group homogeneity. The U.S. population by race and ethnic origin is shown in Figure 2-6 (USCB, 2010). The names used to identify these major U.S. cultural groups are those used by the USCB. The following two modifications were made in the year 2000 census data. The AA/PI category was separated into two categories, Asian American or Native Hawaiian/Pacific Islander; and Latino has been added to the Hispanic category (H/L).
AFRICAN AMERICAN OR BLACK
According to 2010 census data, this group constitutes 12.6% of the population in the United States. This heterogeneous group has origins in black racial groups of Africa and the Caribbean Islands, including the West Indies, Dominican Republic, Haiti, and Jamaica. AA/B persons may speak French, Spanish, African dialects, and various forms of English. By 2050, the AA/B population is expected to nearly double its present size to 61 million. A disproportionate percentage of AA/Bs are disadvantaged because of poverty and low educational levels, and they are more likely to have only public insurance. Comparative lifetime pregnancy rates for U.S. women between the ages of 15 and 44 are 2.7 for W/Cs and 4.6 for AA/B and H/L women. Health disparities exist between W/C and AA/B women (Dominguez, 2011). Infant mortality rates for AA/Bs have consistently been twice those of the overall population (USDHHS, 2010). As a group, AA/Bs are at increased risk for diabetes, lupus, HIV/AIDS, sickle cell anemia, hypertension, and cancer of the esophagus and the stomach (Purnell & Paulanka, 2011; Spector, 2008).
Core Values
AA/B families display resilience and adaptive coping strategies in their struggles with racism and poverty. They have a strong religious commitment, as observed in Southern Baptist, fundamentalist, and black Muslim church communities, which helps to enhance their spiritual health and general well-being (Wehbe-Alamah, McFarland, Macklin, & Riggs, 2011). Fifty-one percent of AA/B families are headed by women, and more than 55% of all AA/B children younger than 3 years are born into single-parent families. AA/B families have extensive networks of extended families, friends, and neighbors who participate in child rearing with a high level of respect for elders. Children are highly valued, and as a result of extended family networks, the “mothering” a child receives comes from many sources. An example of this is the active role assumed by the maternal grandmother when an adolescent pregnancy occurs. Becoming a mother at a young age is acceptable (Nabukera et al., 2009). AA/Bs are demonstrative; comfortable with touch, physical contact, and emotional sharing; and have an orientation toward the present. AA/B women demonstrate great strength and matriarchal leadership, even in the face of devastating challenges, such as being HIV positive and mothering children who were also HIV positive. Providing healthcare to this group may be complicated by folk practices, including the belief that all animate and inanimate objects have good or evil spirits. Healers may include family, a “Granny,” or a spiritualist. Folk practices may also include pica (i.e., ingestion of nonfood items such as starch, clay, ashes, or plaster); use of herbal medicine; and wearing of garlic, amulets, and copper or silver bracelets (Gunn & Davis, 2011; Spector, 2008).
Cultural Beliefs and Practices
Some American blacks may resent being called African Americans because this does not represent their origin (Moore et al., 2010). AA/Bs living in poverty may demonstrate a lack of respect for or fear of public clinics and hospitals. They tend to seek prenatal care later than other women, usually after the first trimester. The incidence of breastfeeding is related to the level of maternal education and social support. AA/B women are more expressive of pain and are usually accompanied during labor and birth by female relatives. Most male newborns are circumcised.
Haitian women are less likely than other groups to seek prenatal care. During pregnancy, they believe they should not swallow their saliva and instead carry a spit cup with them. Fathers are unlikely to be present during birth, believing it is an event only for women. Haitian women are encouraged by their community to breastfeed. However, some inaccurate beliefs, such as thick milk causing skin rashes and thin milk resulting in diarrhea, persist. During the postpartum period, women may believe that a series of three baths aids in their recovery. The first 3 days, women bathe in a special water infused with herbs. For the next 3 days, women bathe in water in which leaves have been soaked and warmed by the sun. After 4 weeks, a cold bath is taken that is believed to tighten muscles and bones loosened during the birth process. Women also believe that wearing a piece of linen or a belt tightly around the waist prevents the entry of gas into their body. Eating white foods such as milk, white lima beans, and lobster is avoided during the postpartum period because they are believed to increase vaginal discharge and hemorrhaging. Traditionally, Haitian women do not have their newborns circumcised because they believe circumcision decreases sexual satisfaction, but as acculturation occurs, this procedure is becoming more common. West Indian countries of origin are Trinidad, Jamaica, and Barbados. Traditionally, the father of the baby is not present during labor and birth.
Ghanian and other African childbearing women may believe in witchcraft and often access Western healthcare, ethnomedicine, and faith-based interventions simultaneously to ensure positive outcomes from pregnancy and childbirth (Farnes, Callister, & Beckstrand, 2011).
Ethiopian woman are considered to be in a delicate state after birth. To be protected from disease and harm, they remain secluded for at least 40 days. A special diet that includes milk and warm foods such as gruel made of oats and honey is thought to increase breast milk production.
Somali refugee women are resistive to and fearful of cesarean births and most technological perinatal interventions and are very afraid of dying in childbirth. As one woman said, “They got a C-section…They gonna die” (Brown, 2010, p. 220).
AMERICAN INDIAN AND ALASKAN NATIVE
Descendants of the original peoples of North America (i.e., American Indian, Eskimo, and Aleut) constitute 0.9% of the population. There are 500 federally recognized AI nations accessing healthcare from Indian Health Services and/or traditional healers.
AI/ANs have a higher unemployment and poverty rate than the general population. They average 9.6 years of formal education, the lowest rate of any major group in the United States. Urban AI/ANs have a much higher rate of low-birth-weight infants compared with urban W/Cs and rural AI/ANs and a higher rate of infant mortality than urban W/Cs. Urban AI/ANs have a high incidence of risk factors associated with poor birth outcomes, including delayed prenatal care, single marital status, adolescent motherhood, and use of tobacco and alcohol. These risk factors resemble the prevalence among AA/ABs except for the higher incidence of alcohol use among AI/ANs. Rural AI/ANs have lower rates of low-birth-weight infants and higher rates of timely prenatal care than their urban counterparts. As a group, AI/ANs have an increased risk for alcoholism, heart disease, cirrhosis of the liver, and diabetes mellitus (Purmell & Paulanka, 2011; Spector, 2008).
Core Values
In general, AI/ANs have a strong spiritual foundation in their lives with a holistic focus on the circular wheel of life. It is important to live in complete harmony with nature. Values include oral traditions passed from generation to generation. Elders play a dominant role in decision making and many AI/AN tribes are matrilineal, so involving maternal grandmothers in teaching young mothers is an important and culturally sensitive intervention. AI/ANs are present oriented, which may make it difficult to obtain an accurate health history because the past may be perceived as unrelated to current conditions. They believe in harmony. They may avoid eye contact and limit touch. Use of a formal interpreter increases the credibility of the healthcare provider because listening is highly valued.
Cultural Beliefs and Practices
During pregnancy, women avoid touching their hair. If an infant is born prematurely or expected to die, a family member may request to perform a ceremony that includes ritual washing of the hair. If hair is removed to initiate a scalp intravenous line on a newborn, some families want the hair returned to them. The mother and newborn remain indoors resting for 20 days or until the umbilical cord falls off. The umbilical cord may be saved, because some AI/ANs believe that it has spiritual significance. Patterns of infant care include group caregiving, living spiritually, merging the infant into Indian culture, using permissive discipline, and observing the child developing.
ASIAN AMERICAN AND PACIFIC ISLANDER
AA/PIs are people with origins in the Far East, Southeast Asia, the Indian subcontinent, or the Pacific Islands. AA/PIs constitute 3.6% of the population in the United States and are projected to make up 8.7% by 2050. There is great diversity in the 28 AA/PI groups designated in the census. Asians comprise 95% of this population and are divided into 17 groups, speaking 32 different primary languages plus multiple dialects. Major groups of AAs include Chinese, Japanese, Koreans, Filipinos, Vietnamese, Cambodians, and Laotians. The major groups, Chinese and Japanese, are the most long-standing groups of Asian immigrants.
PIs comprise 5% of AA/PIs, with specific groups including Hawaiian, Samoan, Guamanian, Tongan, Tahitian, North Marianas, and Fijian. There are more than 50 subgroups speaking at least 32 different languages. Approximately two thirds of Asians living in the United States are foreign-born. This group is culturally and linguistically heterogeneous. In the United States, AA/PIs are highly concentrated in the western states and in metropolitan areas.
There is a paucity of data regarding the health status of AA/PIs. Because they are a small minority, AA/PIs are often overlooked in healthcare services planning and research. In relation to healthcare, AA/PIs comprise the most misunderstood, underrepresented, underreported, and understudied ethnic population. They are often mistakenly referred to as the healthy minority (Kim & Keefe, 2010). Their educational attainment has a bimodal distribution, with 39% having college degrees and 5% assessed as functionally illiterate. They utilize primary and preventive care less often than non-Hispanic whites (Zhao, Esposito, & Wang, 2010). If they have limited English proficiency, barriers to healthcare include making an appointment, locating a health facility, communicating with healthcare providers, and acquiring health literacy (Kim & Keefe, 2010). Posttraumatic stress syndrome is of concern in AA/PI refugee women, especially Hmong women, who may have suffered atrocities while living in their country of origin. Infant mortality rates are highest in Native Hawaiians (11.4/1,000 live births). As a group, AA/PIs are at increased risk of hypertension, liver cancer, stomach cancer, and lactose intolerance (Purnell & Paulanka, 2011; Spector, 2008).
Core Values
Values embody the philosophical traditions of Buddhism, Hinduism, and Christianity. They believe events are predestined and strive for a degree of spirituality in their lives. Core values include cohesive families, filial piety and respect for the elderly, respect for authority, interdependence and reciprocity (group orientation), interpersonal harmony, and avoidance of disagreement and conflict. Pride, fatalism, education/achievement orientation, respect for tradition, and a strong work ethic are also core values. Asians seldom express strong reactions to emotionally arousing events and are taught to suppress feelings to maintain harmonious relationships with others. They avoid public displays of affection, except among family and close friends, and have clearly defined gender roles.
Traditional therapies are often employed concurrently with Western medicine, including acupuncture, herbs, nutrition, and meditation (Callister, Eads et al., 2011; Chuang et al., 2007; Chuang et al., 2009). Asian women may believe Western medicines are too strong and may halve the prescribed dosages. Chinese women avoid oral contraceptives because of a perception that hormones may be harmful. Screening exams such as cervical screening may be avoided because of modesty and discomfort with such intimate procedures.
Cultural Beliefs and Practices
Traditional Asian healthcare beliefs and practices are Chinese in origin, with the exception of Filipino beliefs and practices being based primarily on the Malaysian culture. The yin/yang polarity is a major life force and focuses on the importance of balance for the maintenance of health. Yin represents cold, darkness, and wetness; yang represents heat, brightness, and dryness. For those who subscribe to the hot/cold theory (including Asians and Hispanics), health requires harmony between heat and cold. Balance should be maintained for women to be in harmony with the environment. During pregnancy, women eat “cold” foods such as poultry, fish, fruits, and vegetables. Eating “hot” foods at this time, such as red peppers, spicy soups, red meat, garlic, ginger, onion, coffee, and sweets, is believed to cause abortion or premature labor (Le, Ngai, Lok, Yip, & Chung, 2009). A designation of “hot” or “cold” does not necessarily refer to physical temperature but the specific effects the food is believed to have on the body.
Because pregnancy is a “hot” condition, some expectant mothers may be reluctant to take prenatal vitamins, which are considered a “hot” medication. Encouraging the woman to take her prenatal vitamins with fruit juice may resolve the problem. Some pregnant Asian women believe that iron hardens bones and makes birth more difficult, and these women resist taking vitamin preparations containing iron. Many Southeast Asian women believe that exposure of the genital area is inappropriate because this is considered a sacred part of the body. They may be reluctant to have Pap smears, wait to seek prenatal care, and communicate poorly about physical changes of pregnancy. Sexual intercourse is avoided during the third trimester because it is thought to thicken amniotic fluid, causing respiratory distress in the newborn.
Vaginal exams and an open hospital gown may be deeply humiliating and unnerving to Southeast Asian women, who value humility and modesty. Giving birth is believed to deplete a woman’s body of the “hot” element (blood) and inner energy. This places her in a “cold” state for about 40 days after birth, which is assumed to be the period for the womb to heal. Rice, eggs, beef, tea, and chicken soup with garlic and black pepper are foods high in “hotness” and are eaten by postpartum women. During postpartum, pericare and hygiene are considered important, but women are discouraged from showering for several days to 2 to 4 weeks. They believe that exposure to water cools the body and interrupts balance, which may cause premature aging. Differences between cultural traditions and the Western healthcare delivery system may cause cultural tension (Le et al., 2009). One woman said, “American hospital workers don’t really understand Chinese traditional customs and what may be important to a Chinese mother” (Callister, Eads et al., 2011). Another Chinese woman noted,
[The nurses] don’t really know or understand. They just aren’t aware. Right after birth, I told them I wanted to keep myself warm and I wanted more blankets but they said I didn’t need blankets. As Chinese we are more afraid of the cold but the [nurses] didn’t seem to think so. (Callister, Eads et al., 2011)
Most AA/PI women breastfeed for several years. Women in the Hmong community (originally from Laos) may choose to formula feed, inaccurately believing American women do not breastfeed because they do not see this practice in public like they did in their homelands (Riordan, 2005).
Korean mothers may believe that newborns need sleep and little stimulation. They are discouraged from touching the baby. Thus, they may not understand the amazing capabilities of the newborn to see, hear, and interact. Child rearing often occurs within the extended family. A newborn’s head is considered sacred, the essence of his/her being. Touching the newborn’s head is distressing to parents and should be avoided. Traditionally, newborns have not been circumcised, but as acculturation occurs, some AA/PIs have adopted this practice.
Cambodian women may avoid certain activities during pregnancy, such as standing in doorways, because they believe this will cause the baby to become stuck
in the birth canal. Sexual intercourse is not permitted during the third trimester. It is thought that avoidance of sexual intercourse during pregnancy will produce a more attractive baby. Vernix caseosa is believed to be sperm. Cambodian woman will not be seen cuddling their newborns; instead, the newborn is held down and away from their body. Herbal medications are prepared during the third trimester to be eaten three to four times per day during the postpartum period to restore body heat. Along with eating special foods that are thought to restore lost heat, mothers wear heavy clothing during the postpartum period. Breastfeeding is delayed for several days because colostrum is thought to be harmful for the newborn.
in the birth canal. Sexual intercourse is not permitted during the third trimester. It is thought that avoidance of sexual intercourse during pregnancy will produce a more attractive baby. Vernix caseosa is believed to be sperm. Cambodian woman will not be seen cuddling their newborns; instead, the newborn is held down and away from their body. Herbal medications are prepared during the third trimester to be eaten three to four times per day during the postpartum period to restore body heat. Along with eating special foods that are thought to restore lost heat, mothers wear heavy clothing during the postpartum period. Breastfeeding is delayed for several days because colostrum is thought to be harmful for the newborn.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access