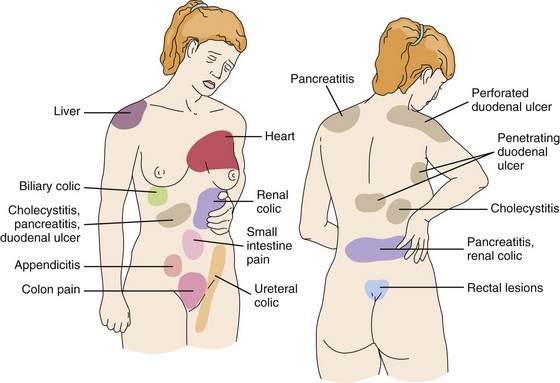
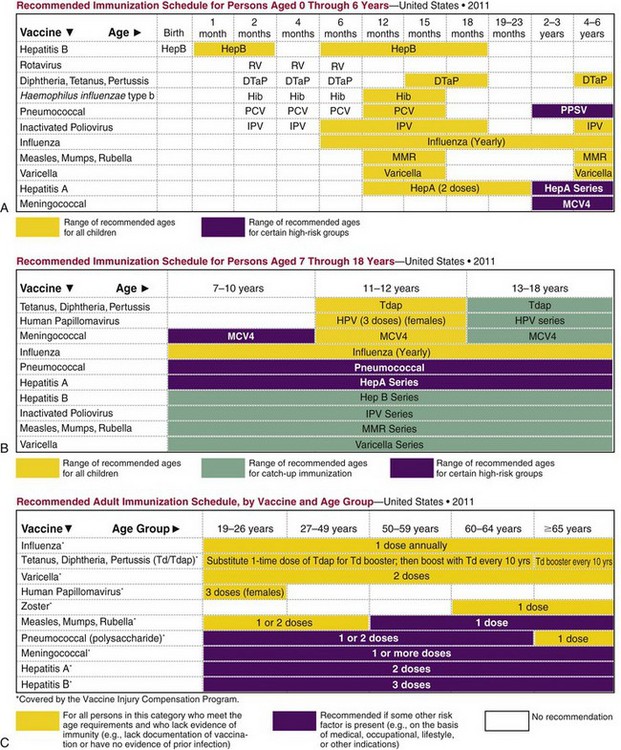
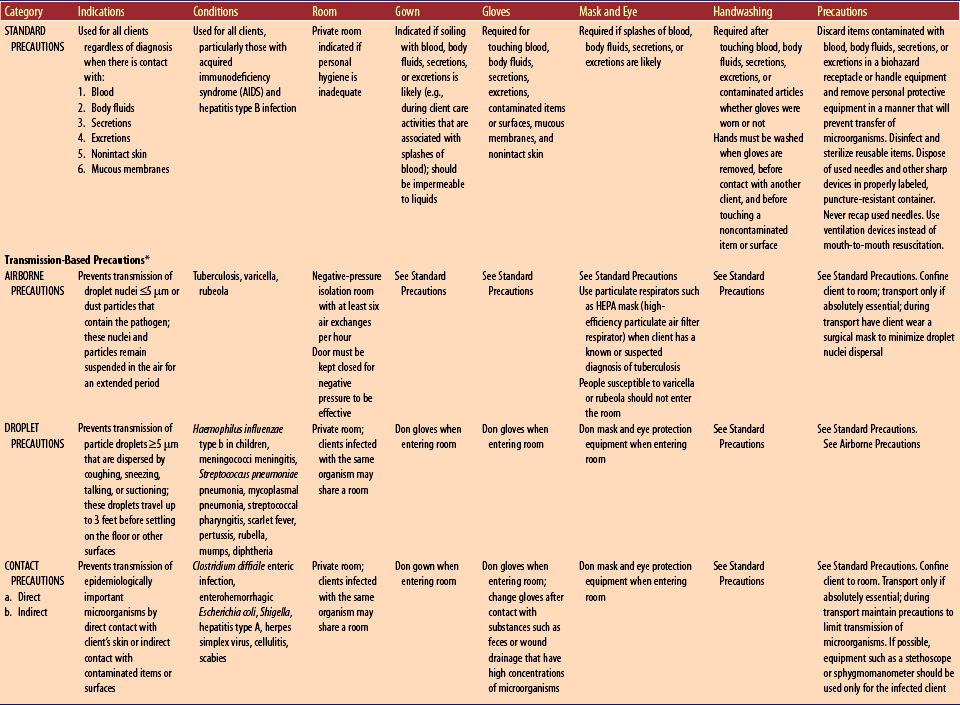
Chapter 3 A Definition: universally unpleasant emotional and sensory experience that occurs in response to actual or potential tissue trauma or inflammation 1. Referred to as fifth vital sign 2. Subjective; pain is whatever client says it is 3. Perception of client’s pain is influenced by multiple factors (e.g., previous pain experience and emotional, physical, and psychological status) 1. Acute pain: mild to severe pain lasting less than 6 months; usually associated with specific injury; involves sympathetic nervous system response; leads to increased pulse rate and volume, rate, and depth of respirations, blood pressure (BP), and glucose level; urine production and peristalsis decrease 2. Chronic pain: mild to severe pain lasting longer than 6 months; associated with parasympathetic nervous system; client may not exhibit signs and symptoms associated with acute pain; may lead to depression and decreased functional status 1. Pain threshold: minimum amount of stimulus required to cause sensation of pain 2. Pain tolerance: maximum pain a client is willing or able to endure 3. Referred pain: pain experienced in an area different from site of tissue trauma (Figure 3-1: Common sites of referred pain) 4. Intractable pain: pain not relieved by conventional treatment 5. Neuropathic pain: pain caused by neurologic disturbance; may not be associated with tissue damage 6. Phantom pain: pain experienced in missing body part 7. Radiating pain: pain experienced at source and extending to other areas A Sensory neurons, nociceptors in peripheral nervous system, are stimulated by biochemical mediators (e.g., bradykinin, serotonin, histamine, potassium, and substance P) when there is mechanical, thermal, or chemical damage to tissue; viscera do not have special neurons for pain transmission; receptors respond to stretching, ischemia, and inflammation B Pain impulses are transmitted to spinal column C Impulse enters at dorsal horn and ascends spinothalamic tract to thalamus D Impulse travels to basal areas of brain and to somatic sensory cortex E Endogenous opioids, such as endorphins, are released and bind to receptors to modify pain transmission F Gate-control theory suggests that stimulation of large-diameter fibers can block transmission of painful impulses through dorsal horn A Acupuncture: insertion of disposable needles into meridians (energy pathways) to change energy flow; may use heat or electric stimulation B Acupressure: finger pressure applied over meridians; less invasive but less effective than acupuncture C Aroma therapy: plant oils applied topically or misted (e.g., ginger for arthritis or headaches, lavender to reduce anxiety associated with pain) have shown benefit D Distraction: focuses client’s attention away from pain E Heat and cold: diminishes pain experience by stimulation of large sensory fibers (gate-control theory) F Imagery: calming, peaceful thoughts reduce pain perception G Massage: stimulates large-diameter fibers, blocking pain transmission H Reflexology: pressure applied to areas on feet, hands, or ears that correspond to specific body organ; may have calming effect through release of endorphins I Sequential muscle relaxation: promotes relaxation and decreases anxiety, thereby reducing pain perception J Transcutaneous or percutaneous electric stimulation: stimulation of peripheral sensory nerve fibers blocks transmission of pain impulse K Therapeutic touch: use of hands near body to improve energy imbalances L Hypnosis: altered state of consciousness in which concentration is focused; believed that pain stimuli in brain are prevented from penetrating the conscious mind; also, may cause release of natural morphine-like substances (e.g., endorphins and enkephalins) 1. Bind to opiate receptors in central nervous system (CNS) 2. Result in diminished transmission and perception of pain impulse B Examples: morphine (MS Contin), codeine, meperidine (Demerol), hydromorphone (Dilaudid), fentanyl (Duragesic, Sublimaze), tapentadol (Nucynta), hydrocodone (Hycodan); administered via oral, buccal, nasal spray, intramuscular (IM), subcutaneous, IV, transdermal, epidural, or rectal routes, depending on drug 1. Monitor for side effects, especially for respiratory depression (e.g., decreased respiratory rate and depth, decreased oxygen saturation) 2. Institute measures to support respiratory function (e.g., encourage frequent turning, coughing, and deep breathing) 3. Ensure availability of opioid antagonist (e.g., naloxone, naltrexone [Vivitrol]) in case of overdose) 4. Ensure medications are renewed at required intervals 5. Keep accurate count of opioids 6. Use measures to promote elimination (e.g., provide fluids, roughage; encourage upright position) 7. Monitor and maintain therapeutic levels of medication; may take 24 hours to achieve when using transdermal route 8. Administer before pain becomes severe because analgesics are less effective when pain is severe 9. Teach how to use patient-controlled analgesia (PCA) pump for management of severe pain; program infusion pump for continuous basal dose, client-controlled bolus dose, and lockout time interval that allow client to control administration without overdose; may be IV, subcutaneous, or epidural 10. Maintain safety after administration of opioid analgesia 11. Instruct to keep medication in secure environment; dispose of excess doses by returning to pharmacy 1. Act on peripheral nerve endings and decrease inflammatory mediators by inhibiting prostaglandin synthesis 2. Have analgesic, antiinflammatory, and antipyretic effects B Examples: aspirin (Ecotrin), ibuprofen (Motrin, Advil), naproxen (Naprosyn, Aleve) (see Related Pharmacology, NSAIDs in Chapter 11) 1. Gastrointestinal (GI) ulceration and bleeding are most common; tarry stools (melena) 2. Kidney and liver impairment 5. Bone marrow depression and impaired coagulation 6. Visual disturbances, headache 7. Tinnitus (especially with aspirin) 10. Hypertension and fluid retention, especially with older adults 1. Analgesic effect may be caused by inhibition of CNS prostaglandin synthesis 2. No effect on peripheral prostaglandin synthesis; therefore no antiinflammatory action B Example: acetaminophen (Tylenol) C Major side effects are few if therapy is short term 1. Teach not to crush extended-relief products 4. Teach to avoid alcohol and other over-the-counter (OTC) products that contain acetaminophen (avoid exceeding maximum dose of 4 g daily) 5. Explain that acetaminophen can be taken concurrently with anticoagulants 6. Ensure availability of antidote for acetaminophen if there is a risk for toxicity (e.g., acetylcysteine [Acetadote]) 1. Client’s description of pain: location; intensity as measured by numeric rating scale of 0 to 10, Wong-Baker FACES Pain Rating Scale, FLACC Scale (Face, Legs, Activity, Cry, Consolability); character; onset; duration; and aggravating and alleviating factors 2. Associated signs and symptoms: increased vital signs (may be decreased with visceral pain), nausea, vomiting, diarrhea, diaphoresis 3. Nonverbal cues: distraught facial expression, rigid or self-splinting body posture 4. Contributing factors: age (older adults may expect pain or may fear addiction, so they may not complain), culture, past experience, anxiety, fear, uncertainty (lack of information), fatigue 5. Effect of pain on ability to perform activities of daily living (ADLs) 1. Individualize pain management based on client’s needs and not on own personal experiences, biases, or cultural beliefs regarding pain 2. Monitor and document client’s pain, associated symptoms, and response to pain management interventions 3. Use nonpharmacologic techniques 4. Administer prescribed analgesics and local anesthetics (see Pain, Related Pharmacology and Perioperative Care, Related Pharmacology, Local Anesthetics) 5. Institute measures to counteract side effects of medications (e.g., increase fiber and fluids to prevent constipation associated with opioids) 6. Provide preoperative and postoperative care for clients requiring surgical intervention for pain management a. Rhizotomy: posterior spinal nerve root is resected between ganglion and spinal cord, resulting in permanent loss of sensation; anterior root may be cut to alleviate pain usually associated with lung cancer b. Cordotomy: alleviates intractable pain in trunk or lower extremities; transmission of pain and temperature sensation is interrupted by creation of lesion in ascending tract; performed percutaneously using an electrode or surgically via laminectomy c. Sympathectomy: controls ischemic and phantom limb pain d. Dorsal column stimulator and peripheral nerve implant: direct attachment of electrode to sensory nerve; electrode is attached to a transmitter that is carried by client so electric stimulation can be administered as needed A Nonspecific immune response: directed against invading microbes 1. Body surface barriers: intact skin and mucosa, cilia, and mucus secretions 2. Antimicrobial secretions: oil of skin, tears, gastric juice, and vaginal secretions 3. Internal antimicrobial agents a. Interferon: substance produced within cells in response to viral attack b. Properdin (Factor P): protein agent in blood that destroys certain gram-negative bacteria and viruses 4. Phagocytes (monocytes, macrophages): cells that ingest and destroy microbes; part of reticuloendothelial system B Specific immune response: directed against a specific pathogen (foreign protein) or its toxin; may be cell-mediated or humoral a. Occurs within cells of immune system b. Involves T lymphocytes (e.g., T helper, T suppressor, T cytotoxic, lymphokines); each type plays a distinct role in immune response c. Cluster designations: mature T cells carry markers on surface that permit them to be classified structurally (e.g., CD4 cells associated with acquired immunodeficiency syndrome [AIDS]) d. Functions of cell-mediated immunity 2. Humoral immunity: concerned with immune responses outside of cell; involves B lymphocytes that differentiate into plasma cells and secrete antibodies a. Antigen: any substance, including allergen, that stimulates production of antibodies in body; typically, antigens are foreign proteins, most potent being microbial cells and their products b. Antibody: immune substance produced by plasma cells; antibodies are gamma globulin molecules; commonly referred to as immunoglobulin (Ig) c. Complement-fixation: group of blood serum proteins needed in certain antigen-antibody reactions; both complement and antibody must be present for reaction to occur (1) Immunoglobulin M (IgM) antibodies: first antibodies to be detected after exposure to antigen; protection from gram-negative bacteria (2) Immunoglobulin G (IgG) antibodies: make up more than 75% of total immunoglobulins; highest increase in response to subsequent exposure to antigen; only immunoglobulin that passes placental barrier (3) Immunoglobulin A (IgA) antibodies: present in blood, mucus, and human milk secretions; play important role against viral and respiratory pathogens (4) Immunoglobulin E (IgE) antibodies: responsible for hypersensitivity and allergic responses; cause mast cells to release histamine; protection from parasites (5) Immunoglobulin D (IgD) antibodies: help differentiate B lymphocytes 1. Active immunity: antibodies formed in body a. Natural active immunity: antibodies formed during course of disease; may provide lifelong immunity (e.g., measles, chickenpox, yellow fever, smallpox) b. Artificial active immunity: vaccine or toxoid stimulate formation of homologous antibodies; revaccination (booster shot) often needed to sustain antibody titer (anamnestic effect) (Figure 3-2: Recommended immunization schedules—United States 2011) Figure 3-2 Recommended immunization schedules—United States 2011. A, Schedule for persons aged 0 through 6 years. B, Schedule for persons aged 7 through 18 years. C, Schedule for adults. (From Centers for Disease Control and Prevention: Immunization Schedules—United States 2011. Accessed online at http://cdc.gov/vaccines/recs/schedules/.) (1) Killed vaccines: antigenic preparations containing killed microbes (e.g., pertussis vaccine, typhoid vaccine) (2) Live vaccines: antigenic preparations containing weakened (attenuated) microbes; typically such vaccines are more antigenic than killed preparations (e.g., oral [Sabin] poliomyelitis vaccine, measles vaccine) (3) Toxoids: antigenic preparations composed of inactivated bacterial toxins (e.g., tetanus toxoids, diphtheria toxoids) 2. Passive immunity: antibodies acquired from outside source produce short-term immunity a. Natural passive immunity: passage of preformed antibodies from mother through placenta to fetus or though colostrum to neonate; during first few weeks of life newborn is immune to certain diseases to which mother has active immunity b. Artificial passive immunity: injection of antisera derived from immunized animals or humans; provide immediate protection and also are of value in treatment (e.g., diphtheria antitoxin, tetanus antitoxin) A Infection: invasion of body by pathogenic microorganisms (pathogens) and reaction of tissues to their presence and to toxins generated by them a. Local infection: limited to one locality (e.g., abscess), causing pain, swelling, and erythema; may have systemic repercussions such as fever, malaise, and lymphadenopathy b. Systemic infection: infectious agent is spread throughout body (e.g., typhoid fever) 2. Length of infectious process a. Acute infection: one that develops rapidly, usually resulting in high fever and severe sickness; resolves in a short time b. Chronic infection: one that develops slowly, with mild but longer-lasting clinical manifestation; sometimes an acute infection can become chronic 3. Etiology of infectious process a. Primary infection: develops after initial exposure to pathogen, unrelated to other health problems b. Secondary infection: develops when pathogens take advantage of weakened defenses resulting from a primary infection (e.g., staphylococcal pneumonia as sequela of measles) c. Opportunistic infection: develops when host defenses are diminished because of disease process or therapeutic modalities (e.g., vaginal yeast infection following antibiotic therapy) 2. Reservoir: source of almost all pathogens is human or animal a. Persons exhibiting manifestations of disease b. Carriers: persons who harbor pathogens in absence of discernible clinical disease 3. Portals of exit: route by which microorganisms leave body; blood and body fluids, skin, mucous membranes, and respiratory, genitourinary, and GI tracts a. Contact transmission (e.g., Staphylococcus aureus) (1) Direct: contact between body surfaces (2) Indirect: contact between susceptible host and contaminated intermediate object (e.g., sink faucets) b. Droplet transmission: droplets from infected individual are propelled short distance by coughing, sneezing, talking, or suctioning respiratory secretions (e.g., common cold) c. Airborne transmission: small droplet nuclei (5 µm or smaller) or dust particles that contain pathogen remain suspended in air for extended period (e.g., Mycobacterium tuberculosis) d. Common vehicle transmission: microorganisms are transmitted by contaminated food, water, or equipment (e.g., typhoid fever) e. Vector-borne transmission: microorganisms transmitted by vectors such as mosquitoes, flies, ticks, and rats (e.g., Rocky Mountain spotted fever, Lyme disease) 5. Portals of entry: same as portals of exit except skin; intact skin prevents infection 1. Unicellular microbes without chlorophyll 2. Capsule: material secreted by cell, protects it from phagocytosis and increases its virulence (e.g., Diplococcus pneumoniae) 3. Spores: inactive resistant structures into which bacterial protoplasm can transform under adverse conditions; under favorable conditions spore germinates into active cell (e.g., Clostridium tetani, Clostridium defficile) 4. Examples of disease-producing bacteria a. Eubacteriales: divided into five families based on shape, gram stain, and endospore formation (a) Diplococci: occurring predominantly in pairs (e.g., Diplococcus pneumoniae) (b) Streptococci: occurring predominantly in chains (e.g., Streptococcus pyogenes) (c) Staphylococci: occurring predominantly in grapelike bunches (e.g., S. aureus) (2) Gram-negative cocci include Neisseria gonorrhoeae and Neisseria meningitidis (3) Gram-negative rods include enterobacteria such as Escherichia, Salmonella, and Shigella species (4) Gram-positive rods that do not produce endospores include Corynebacterium diphtheriae (5) Gram-positive rods that produce endospores include Bacillus anthracis, Clostridium botulinum, and Clostridium tetani b. Actinomycetales (actinomycetes): moldlike microbes with elongated cells, frequently filamentous (e.g., Mycobacterium tuberculosis, Mycobacterium leprae) c. Spirochaetales (spirochetes): flexuous, spiral organisms (e.g., Treponema pallidum) d. Mycoplasmatales (mycoplasmas): delicate, nonmotile microbes displaying a variety of sizes and shapes 1. Obligate intracellular parasite; replicates only within cell of another organism; composed of either ribonucleic acid (RNA) or deoxyribonucleic acid (DNA), not both 2. Examples of disease-producing viruses 1. Saprophytic organisms that live on organic material 2. Molds: fuzzy growths of interlacing filaments called hyphae; reproduce by spores 3. Yeasts: organisms that usually are single-celled; usually reproduce by budding 4. Examples of disease-producing fungi 1. Medical asepsis (Table 3-1: Precautions to Prevent the Spread of Microorganisms) Table 3-1 Precautions to Prevent the Spread of Microorganisms *Used in addition to standard precautions for clients with documented or suspected infection with highly transmittable or epidemiologically important pathogens. a. Standard precautions (e.g., hand hygiene, personal protective equipment [PPE]) b. Transmission-based precautions (e.g., airborne, droplet, contact) 3. Disinfection: removal or destruction of pathogens 4. Sterilization: removal or destruction of all microbes 5. Antiseptic: inhibits microbial growth 7. Radiation: all types of radiation injurious to microbes A Bactericidal effect: destroys bacteria at low concentrations B Bacteriostatic effect: slows reproduction of bacteria C Superinfection (secondary infection): emergence of microorganism growth when natural protective flora are destroyed by an anti-infective drug D Bacterial resistance: natural or acquired characteristic of an organism that prevents destruction by a drug to which it was previously susceptible 1. Destroy bacteria or inhibit bacterial reproduction to control infection 2. Available in oral, parenteral, and topical forms, including ophthalmic and ear drop preparations B Antibiotic sensitivity tests: identify antibiotics that are effective against a particular organism C Mechanism of action: interfere with or inhibit cell-wall synthesis of RNA or DNA of pathogen 1. Penicillins (broad spectrum): amoxicillin may be combined with a second drug to prevent bacterial resistance such as amoxicillin and clavulanate (Augmentin), ampicillin and sulbactam (Unasyn), piperacillin and tazobactam (Zosyn) 2. Cephalosporins (broad spectrum): cefazolin (Ancef), cephalexin (Keflex) 3. Erythromycins: clindamycin HCl (Cleocin HCl), azithromycin (Zithromax), erythromycin (Ery-Tab, Eryc) 4. Tetracyclines (broad spectrum): doxycycline (Vibramycin), tetracycline (Sumycin) 5. Aminoglycosides (broad spectrum): gentamicin, neomycin, streptomycin 6. Quinolones (broad spectrum): ciprofloxacin (Cipro) and levofloxacin (Levaquin) 7. Polymyxin group: polymyxin B 1. Depressed appetite (altered taste sensitivity) 2. Nausea, vomiting (normal flora imbalance) 3. Diarrhea (normal flora imbalance) 4. Suppressed absorption of variety of nutrients including fat; protein; lactose; vitamins A, D, K, and B12; and the minerals calcium, iron, and potassium (normal flora imbalance) 5. Increased excretion of water-soluble vitamins and minerals (normal flora imbalance) 6. Superinfection (normal flora imbalance) 7. Allergic reactions, anaphylaxis (hypersensitivity) 8. Nephrotoxicity (direct kidney toxic effect) 9. Can render oral contraceptives ineffective a. Hepatotoxicity (direct liver toxic effect) b. Phototoxicity (degradation to toxic products by ultraviolet rays) c. Hyperuricemia (impaired kidney function) d. Enamel hypoplasia, dental caries, and bone defects in children younger than 8 years of age (drug binds to calcium in tissue) a. Ototoxicity (direct toxic effect to auditory [eighth cranial] nerve) b. Leukopenia (decreased white blood cell [WBC] synthesis) c. Thrombocytopenia (decreased platelet synthesis) d. Headache, confusion (neurotoxicity) e. Peripheral neuropathy (neurotoxicity) f. Nephrotoxicity (direct kidney toxic effect) 1. Assess for history of drug allergy a. How to take drug (e.g., frequency, relation to meals) b. Prevention of emergence of resistant strains of microorganisms (e.g., methicillin-resistant Staphylococcus aureus [MRSA]) by completing prescribed course of therapy c. Symptoms of allergic response d. Need to report side effects, including signs of superinfection (e.g., vaginal itching, diarrhea, change in cough or sputum, white plaques in mouth); suggest ingestion of yogurt or food supplements containing probiotics such as Lactobacillus acidophilus when dairy products cannot be tolerated; suggest nutritional consultation when drug therapy may have negative impact on client’s nutritional status e. Monitor for and promptly report pain, changes in urinary or hearing function 3. Shake liquid suspensions to mix thoroughly 4. Administer most preparations 1 hour before meals or 2 hours after meals for best absorption 5. Administer at equal intervals around the clock to maintain blood levels 6. Assess vital signs during course of therapy 7. Provide well-balanced diet and adequate fluids 8. Encourage use of alternate form of birth control (vs. birth control pills) during therapy a. Explain why they are contraindicated during last half of pregnancy or by children younger than 8 years of age b. Assess for potentiation if concurrently receiving oral anticoagulants c. Teach to avoid direct sunlight d. Advise to avoid dairy products, antacids, or iron preparations because they reduce effectiveness 10. Aminoglycosides: assess for potentiation if client is receiving neuromuscular blocking agents, general anesthetic, or parenteral magnesium; monitor renal and neurologic function 11. Vancomycin: assess peak and trough blood levels because these drugs have a narrow therapeutic range; incompatible with heparin 1. Prevent entrance of virus into host cells; provide prophylaxis after exposure to a person with a viral infection; 2. Available in oral, intravenous, and topical, including ophthalmic, preparations B Examples: acyclovir (Zovirax), amantadine (Symmetrel), zanamivir (Relenza), oseltamivir (Tamiflu) 1. CNS stimulation (direct CNS effect) 2. Orthostatic hypotension (depressed cardiovascular system) 4. Constipation (decreased peristalsis) 5. Nephrotoxicity (direct kidney toxic effect) 1. Assess vital signs during course of therapy 2. Support natural defense mechanisms (e.g., encourage intake of foods rich in immune-stimulating nutrients, such as vitamins A, C, and E, and the minerals selenium and zinc) 3. Encourage intake of high-fiber foods to reduce potential for constipation 4. Monitor disease signs and symptoms and laboratory data 1. Substitute a false metabolite for para-aminobenzoic acid (PABA), required in bacterial synthesis of folic acid; treat urinary tract infections 2. Available in oral, parenteral (IM, IV), and topical, including ophthalmic, preparations B Examples: sulfiSOXAZOLE and combination products such as sulfamethoxazole and trimethoprim (Bactrim, Septra) 1. Nausea, vomiting; decreased absorption of folacin (irritation of gastric mucosa) 2. Skin rash (hypersensitivity) 3. Malaise (decreased red blood cells [RBCs]) 4. Blood dyscrasias (decreased RBCs, WBCs, platelet synthesis) 5. Crystalluria (drug precipitation in acidic urine) 6. Stomatitis (irritation of oral mucosa) 8. Photosensitivity (hypersensitivity) 1. Assess for history of drug allergy 2. Promote increased fluid intake 3. Caution to avoid dehydration and direct exposure to sunlight 4. Assess vital signs during course of therapy 6. Administer at routine intervals around clock to maintain blood levels; obtain blood specimens for peak and trough levels 7. Monitor blood work during therapy because of potential for megaloblastic anemia caused by folacin deficiency 8. Assess for potentiation of oral anticoagulant and oral hypoglycemic effects 9. Monitor for dysuria and urinary output 1. Destroy fungal cells (fungicidal) or inhibit reproduction of fungal cells (fungistatic); treat systemic and localized fungal infections 2. Available in oral, IV, topical, vaginal, and intrathecal preparations 1. Amphotericin B (Fungizone), nystatin (Mycostatin, Nilstat): disrupts fungal cell membrane permeability 2. Fluconazole (Diflucan): disrupts fungal cell membrane function 3. Griseofulvin (Gris-PEG): disrupts fungal nucleic acid synthesis 1. Assess vital signs during course of therapy 2. Review proper method of application a. Use infusion control device for IV administration b. Protect solution from light during IV infusion c. Monitor blood work during therapy because of potential hypokalemia and increased urinary excretion of magnesium d. Premedicate with antipyretics, corticosteroids, antihistamines, and antiemetics before IV administration 1. Interfere with parasite metabolism and reproduction; treat parasitic diseases; helminthic (e.g., pinworm, tapeworm); protozoal (e.g., amebiasis, malaria) 2. Available in oral, parenteral (IM, subcutaneous [Sub-Q], IV), vaginal, and rectal preparations 2. Amebicides: chloroquine phosphate (Aralen), metronidazole (Flagyl) 3. Antimalarials: chloroquine phosphate (Aralen), hydroxychloroquine (Plaquenil), quinine (Qualaquin) a. Nausea, vomiting, diarrhea (GI irritation) b. Blood dyscrasias (decreased RBCs, WBCs, platelet synthesis) c. Skin rash (hypersensitivity) 1. Administer with meals to decrease GI irritability 2. Assess vital signs during course of therapy 3. Monitor blood work during therapy 4. Instruct regarding hygiene practices to prevent spread of infestation 5. Ensure safety (e.g., supervise ambulation) if CNS effects are manifested 6. Antimalarials: encourage frequent visual examinations 7. Antiprotozoals: assess for bronchial constriction that may interfere with desired effect of aerosol pentamidine; assess for side effects of sudden severe hypotension 8. Instruct to report unusual bruising or bleeding
Integral Aspects of Nursing Care
Pain
Overview
Review of Physiology
Nonpharmacologic Pain Management Strategies
![]() Related Pharmacology
Related Pharmacology
Opioid Analgesics
Nonsteroidal Antiinflammatory Drugs (NSAIDs)
Other Nonopioid Analgesics
General Nursing Care of Clients in Pain
Assessment/Analysis
Planning/Implementation
Infection
Review of Physiology (Immunity)
Review of Microbiology
Pathology of Infection
Types of Pathogens
![]() Related Pharmacology
Related Pharmacology
Definition of Terms
Antibiotics
Antivirals
Sulfonamides
Antifungals
Antiparasitics