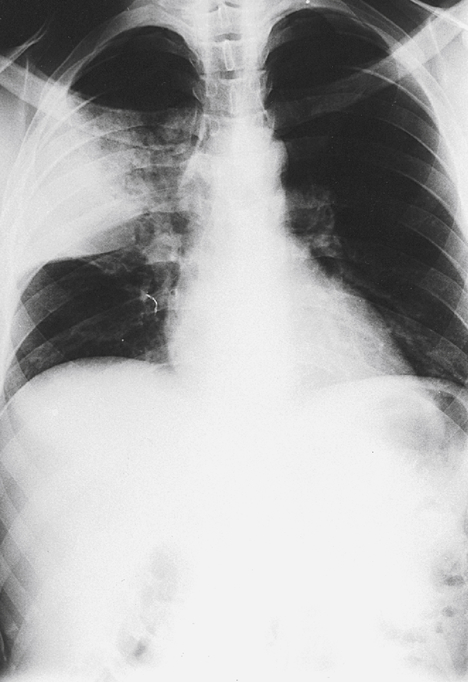
Chapter 20 ∗H. influenzae is no longer as common a cause of meningitis in children because of widespread vaccination. In a child with no history of immunization, H. influenzae is the most likely cause of meningitis. †Examples: Oxacillin, nafcillin. ‡Think of staphylococci if the patient is monogamous or not sexually active. Think of gonorrhea for younger adults who are sexually active. ∗Always use culture sensitivities to guide therapy once available. †With genital infections, always treat for presumed Chlamydia coinfection with azithromycin or doxycycline. Streptococcus pneumoniae. Look for rapid onset of shaking chills after 1 to 2 days of upper respiratory infection symptoms (sore throat, runny nose, dry cough), followed by fever, pleurisy, and productive cough (yellowish-green or rust-colored from blood), especially in older adults. Chest radiograph shows lobar consolidation (Fig. 20-1), and the white blood cell count is high with a large percentage of neutrophils. Treat with a macrolide (e.g., azithromycin, clarithromycin), doxycycline, third-generation cephalosporin with a macrolide or doxycycline, or a fluoroquinolone that provides atypical coverage (e.g., levofloxacin, moxifloxacin).
Infectious Diseases
1 Cover the middle and right-hand columns and specify which bugs are associated with each type of infection and what type of empirical antibiotic should be used while waiting for culture results.
CONDITION
MAIN ORGANISM(S)
EMPIRICAL ANTIBIOTICS
Urinary tract infection
Escherichia coli
Trimethoprim-sulfamethoxazole, nitrofurantoin, amoxicillin, quinolones
Bronchitis
Virus, Haemophilus influenzae, Moraxella spp.
Usually no benefit from antibiotics. May consider macrolides or doxycycline
Pneumonia (classic)
Streptococcus pneumoniae, H. influenzae
Third-generation cephalosporin, azithromycin
Pneumonia (atypical)
Mycoplasma, Chlamydia spp.
Macrolide antibiotic, doxycycline
Osteomyelitis
Staphylococcus aureus, Salmonella spp.
Oxacillin, cefazolin, vancomycin
Cellulitis
Streptococci, staphylococci
Cephalexin or dicloxacillin. Trimethoprim-sulfamethoxazole, doxycycline, or clindamycin are often used as first-line agents because of the emergence of methicillin-resistant S. aureus (MRSA)
Meningitis (neonate)
Streptococci B, E. coli, Listeria spp.
Ampicillin + aminoglycoside (usually gentamicin); an expanded spectrum third-generation cephalosporin (cefotaxime) should be added if a gram-negative organism is suspected
Meningitis (child/adult)
S. pneumoniae, Neisseria meningitidis∗
Cefotaxime or ceftriaxone + vancomycin
Endocarditis (native valve)
Staphylococci, streptococci,
Antistaphylococcal penicillin† (or vancomycin if allergic to penicillin) + aminoglycoside
Endocarditis (prosthetic valve)
Sepsis
Numerous different organisms
Gram-negative organisms, streptococci, staphylococci
Vancomycin + gentamicin + cefepime or a carbapenem
Third-generation penicillin/cephalosporin + aminoglycoside, or imipenem
Septic arthritis‡
S. aureus
Gram negative bacilli
Gonococci
Vancomycin
Ceftazidime or ceftriaxone
Ceftriaxone, ciprofloxacin, or spectinomycin
2 Cover the middle and right-hand columns and specify the empirical antibiotic of choice for each organism.
ORGANISM∗
ANTIBIOTIC
OTHER CHOICES
Streptococcus A or B
Penicillin, cefazolin
Erythromycin
S. pneumoniae
Third-generation cephalosporin + vancomycin
Fluoroquinolone
Enterococcus
Penicillin or ampicillin + aminoglycoside
Vancomycin + aminoglycoside
Staphylococcus aureus
Antistaphylococcus penicillin (e.g., methicillin)
Vancomycin, trimethoprim-sulfamethoxazole, doxycycline, clindamycin, or linezolid for MRSA
Gonococcus†
Ceftriaxone
Cefixime or high-dose azithromycin followed by test of cure in 1 week
Meningococcus
Cefotaxime or ceftriaxone
Chloramphenicol or penicillin G if proven to be penicillin susceptible
Haemophilus
Second- or third-generation cephalosporin
Amoxicillin
Pseudomonas
Antipseudomonal penicillin (ticarcillin, piperacillin) +/- beta lactamase inhibitor (clavulanate, tazobactam)
Ceftazidime, cefepime, aztreonam, imipenem, ciprofloxacin
Bacteroides
Metronidazole
Clindamycin
Mycoplasma
Erythromycin, azithromycin
Doxycycline
Treponema pallidum
Penicillin
Doxycycline
Chlamydia
Doxycycline, azithromycin
Erythromycin, ofloxacin
Lyme disease (Borrelia spp.)
Cefuroxime, doxycycline, amoxicillin
Erythromycin
3 Cover the right-hand column and specify what each Gram stain most likely represents.
GRAM STAIN RESULT
MEANING
Blue/purple color
Gram-positive organism
Red color
Gram-negative organism
Gram-positive cocci in chains
Streptococci
Gram-positive cocci in clusters
Staphylococci
Gram-positive cocci in pairs (diplococci)
Streptococcus pneumoniae
Gram-negative coccobacilli (small rods)
Haemophilus sp.
Gram-negative diplococci
Neisseria sp. (sexually transmitted disease, septic arthritis, meningitis) or Moraxella sp. (lungs, sinusitis)
Plump gram-negative rod with thick capsule (mucoid appearance)
Klebsiella sp.
Gram-positive rods that form spores
Clostridium sp., Bacillus sp.
Pseudohyphae
Candida sp.
Acid-fast organisms
Mycobacterium (usually M. tuberculosis), Nocardia sp.
Gram-positive with sulfur granules
Actinomyces sp. (pelvic inflammatory disease [PID] in intrauterine device users; rare cause of neck mass/cervical adenitis)
Silver-staining
Pneumocystis jiroveci and cat-scratch disease
Positive India ink preparation (thick capsule)
Cryptococcus neoformans
Spirochete
Treponema sp., Leptospira sp. (both seen only on dark-field microscopy), Borrelia sp. (seen on regular light microscope)
5 What is the most common cause of pneumonia? How does it classically present?
14 Cover the middle and right-hand columns and specify the organism after looking at the scenario associated with it.
SCENARIO
ORGANISM(S)
COMMENTS
Stuck with thorn or gardening
Sporothrix schenckii
Treat with itraconazole
Aplastic crisis in sickle cell disease
Parvovirus
B19
Sepsis after splenectomy
Streptococcus pneumoniae,
Haemophilus influenzae,
Neisseria meningitis
(encapsulated bacteria)
Pneumonia in the Southwest (California, Arizona)
Coccidioides immitis
Treat with itraconazole or fluconazole; amphotericin B for severe disease
Pneumonia after cave exploring or exposure to bird droppings in Ohio and Mississippi River valleys
Histoplasma capsulatum
Pneumonia after exposure to a parrot or exotic bird
Chlamydophila psittaci
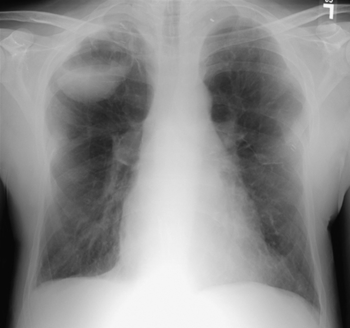
Fungus ball/hemoptysis after tuberculosis or cavitary lung disease
Aspergillus sp.
Treat with voriconazole (Fig. 20-2)
Pneumonia in a patient with silicosis
Tuberculosis
Diarrhea after hiking/drinking from a stream
Giardia lamblia
Stool cysts; treat with metronidazole
Pregnant woman with cats
Toxoplasma gondii
Treat infected pregnant women with spiramycin
B12 deficiency and abdominal symptoms
Diphyllobothrium latum
(intestinal tapeworm)
Seizures with ring-enhancing brain lesion on computed tomography (CT)
Taenia solium (cysticercosis) or toxoplasmosis
Treat neurocysticercosis with albendazole or praziquantel, usually with steroids; consider anticonvulsants
Squamous cell bladder cancer in Middle East or Africa
Schistosoma haematobium
Worm infection in children
Enterobius sp.
Perianal itching, positive tape test; treat with mebendazole or albendazole
Fever, muscle pain, eosinophilia, and periorbital edema after eating raw meat
Trichinella spiralis (trichinosis)
Gastroenteritis in young children
Rotavirus, Norwalk virus
Food poisoning after eating reheated rice
Bacillus cereus
Infection is usually self-limited
Food poisoning after eating raw seafood
Vibrio parahaemolyticus
Diarrhea after travel to Mexico
Escherichia coli (Montezuma revenge)
Treat with ciprofloxacin
Diarrhea after antibiotics
Clostridium difficile
Use oral metronidazole or oral vancomycin
Baby paralyzed after eating honey
Clostridium botulinum
Toxin blocks acetylcholine release
Genital lesions in children in the absence of sexual abuse or activity
Molluscum contagiosum
Cellulitis after cat/dog bites
Pasteurella multocida
Treat animal bite wounds with prophylactic amoxicillin-clavulanate
Slaughterhouse worker with fever
Brucellosis
Pneumonia after being in hotel or near air conditioner or water tower
Legionella pneumophila
Treat with azithromycin or levofloxacin
Burn wound infection with blue/green color
Pseudomonas sp.
S. aureus is also a common burn infection, but it lacks blue-green color ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access