Chapter 2 Infectious Disease and Health Breakdown
When you have completed this chapter you will be able to
THE CONCEPT OF INFECTION
Human beings, like other animals, play host to a wide variety of microorganisms. These microorganisms are referred to as commensals or the ‘normal flora’ of the body and may be beneficial to the human host1 (see Table 2.1). Microorganisms assist in metabolising food, production of vitamins (e.g., vitamin K), have a protective function against infection and stimulate the immune response2. Microorganisms are found in parts of the body that are exposed to, or communicate with the environment, including, for example, the skin, nose and mouth, intestinal and female genital tracts. These organisms are derived from sources such as the maternal genital tract at birth, close contacts, the environment and food3. The internal organs and tissues of the body, such as the brain, spinal cord and vascular system, are normally sterile, that is, there is an absence of commensal organisms1.
TABLE 2.1 EXAMPLES OF NORMAL FLORA IN HUMANS
| Area of the Body | Commensal Organisms |
|---|---|
| Mouth and teeth | |
| Throat | Bacteria: |
| Skin | Bacteria: |
| Bowel | Bacteria: |
| Vagina (adult) |
The term colonisation is used to describe the presence of commensal microorganisms where there is no disruption to the normal body function2. Colonisation may be transient or permanent. In contrast, microorganisms that are capable of invading the body and causing disease are termed pathogens3. Infection is a disease process caused by a pathogen and occurs when the interaction between the pathogen and the host results in pathological processes and associated tissue damage in the host3. The tissue damage associated with infection can result from microbial factors and activities, for example, it can result from a proliferation of the microorganisms and the production of toxins, or from the effects of the host’s immune response to the organism.
Some microorganisms are always associated with disease in humans and are termed strict pathogens. Examples include Salmonella and Shigella (as causes of gastroenteritis) and the rabies virus2. However, many infections are caused by opportunistic pathogens, organisms that usually do not cause disease, yet if introduced into sites where they are not typically found, or when host susceptibility is altered, may result in disease3. The bacterium, Escherichia coli is an example of a microorganism that normally colonises the gastrointestinal tract, but can cause urinary tract infections especially when an indwelling urinary catheter is present. Pathogenicity is the organism’s ability to cause disease in a susceptible host, while virulence refers to the organism’s enhanced capacity to cause more severe infection, a quantitative measure of pathogenicity4.
OBLIGATORY STEPS IN INFECTION
For infectious organisms to perpetuate in nature there needs to be a sequence of interactions between the organism and the potential host. First, the microorganism must gain entry into the body. Humans have many natural barriers such as skin, antibacterial secretions (e.g., lysozyme), and the presence of mucous or ciliated epithelium to prevent organisms accessing the body5. However, any breach in these defences, such as a cut to the skin or an invasive device, may allow organisms to enter. Other bodily functions or activities may facilitate access to the body, for example, inhalation or ingestion6.
Depending on the type of infection, there will be a local effect or a generalised response in the body through the blood or lymphatic system. Once established within the host, the organisms replicate to establish sufficient numbers for continued spread and invasion. Many pathogenic microorganisms have developed strategies that facilitate evasion of immune and other defence mechanisms in the host, so that replication can be completed. Human immunodeficiency virus (HIV) exhibits such an evasion system by killing or interfering with the T-cells of the immune system, which are normally required to eliminate the virus3,5.
Crucially, in order to perpetuate the infective process, the pathogen must be shed from its current host in a manner – and in sufficient numbers – that enables spread of the pathogen to new hosts. Various mechanisms may assist the pathogen in this process. Viruses that infect the upper respiratory tract, such as the common cold, may induce increased nasal secretions; and they may stimulate coughing and sneezing, with the droplets containing virus particles that can then spread to new potential hosts. For gastrointestinal infections, the combination of diarrhoea and inadequate hygiene practices has been highly successful in spreading diseases such as cholera and typhoid5.
SIGNS AND SYMPTOMS OF INFECTION
The signs and symptoms associated with infection vary, depending on the causative organism and the site of the infection. One of the most common manifestations of infection is fever and it is believed to be beneficial in combatting the infection process7. Pathogens associated with human disease replicate most effectively at temperatures at or below 37°C. The higher temperatures seen in fever may inhibit pathogen replication, and promote phagocytosis, antibody and interferon production, thus aiding the immune response7.
Many organisms also cause some degree of inflammation with the presence of local heat, swelling, redness and pain at the site of infection. The inflammatory response is a combination of vasodilation, an outpouring of exudate from dilated capillaries, an accumulation of white cells (neutrophils and macrophages) into an area, and the release of immune active chemicals, which regulate the immune response3.
Rashes are a distinct form of inflammation and their site of origin, form of spread and characteristic type of skin lesion can aid in diagnosing specific infections. Some rashes are evidence of the harmful effects of the interaction between the pathogen and the host’s immune system3.
Other signs and symptoms will be dependent on the infecting organisms and disease caused. Some viruses are cytopathic and cause direct cellular damage, for example, poliovirus, HIV and rhinoviruses (common cold viruses)5. Plasmodium, the protozoan cause of malaria, causes direct damage to erythrocytes as part of its disease cycle. Toxin-mediated effects are a feature of bacterial infection and are varied and numerous. Clostridium tetani releases a neurotoxin causing the spastic paralysis seen in tetanus. Staphylococcus aureus may produce a range of toxins, including the toxin responsible for the often-serious toxic shock syndrome. A further example is found in the enterotoxins causing enteritis2.
THE TRANSMISSION OF INFECTION AND THE PRINCIPLES OF INFECTION CONTROL
The Chain of Infection is represented by a simple model, based on the steps required for the transmission of infection (see Figure 2.1). Each link in the chain must be present and in sequence for an infection to occur. The six components of the Chain of Infection4 are
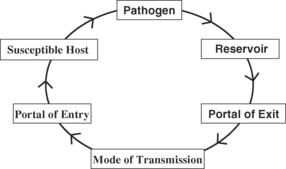
FIGURE 2.1 Chain of Infection.
Source: Adapted from Lawrence, J & May, D. 2003; Infection Control in the Community, Churchill Livingstone, Edinburgh, Fig. 2.4, p. 17.
The main groups of pathogens causing infection in humans are viruses, bacteria, fungi, protozoa, helminths (worms) and arthropods1. A great diversity for potential reservoirs of these organisms exists, including humans, animals, the environment, and contaminated water and food. For example, the hepatitis A virus may be found in water or food contaminated with sewage (resulting in contaminated shellfish), and Listeria can be associated with uncooked meat products, for example, salami and some pâtés (liver spreads). Inanimate sources are environmental, such as dust and contaminated equipment. Humans form a major animate reservoir along with other animals such as cattle, chickens, rodents and some insects4. When an organism causing infection arises from these external sources, it is termed exogenous. Alternatively, if the organism arises from the patient’s own normal microbial flora, it is then considered to be endogenous in origin6.
Portals of exit are the mechanisms by which the microorganisms mobilise from the reservoir at a given time. In considering the human being as a reservoir, potential portals of exit include excretions and secretions, such as faeces, sputum, saliva and the droplets contained within a cough or a sneeze5.
The potential modes of transmission facilitating the spread of micro-organisms are summarised in Table 2.2. Transmission depends upon several factors including the number of organisms shed and their ability to survive in the environment. There is marked variation in the number of organisms required to infect a new host. Only 10–100 Shigella dysenteriae organisms will cause disease in a host. However, 1 × 106Salmonella organisms are necessary to result in Salmonella food poisoning5. Transmission may be aided by the organism’s ability to facilitate spread, such as respiratory illnesses that promotes coughing/sneezing in their host, or those diseases that produce diarrhoea5.
TABLE 2.2 EXAMPLES OF THE MODES OF TRANSMISSION FOR MICROORGANISMS
| Mode of Transmission | Explanation | Examples |
| Direct contact | Mostly via human hands, which are easily contaminated by contact with reservoirs of microorganisms, such as other humans, the environment, secretions and excretions. | Bacteria such as methicillin-resistant Staphylococcus aureus, vancomycin-resistant enterococci, contagious skin conditions, i.e., scabies, impetigo. |
| Droplet | Via contact of the mucous membranes of the nose/mouth or conjunctiva with large particle droplets (>5 nm), which contain the microorganisms created by persons with or carrying the disease. | Neisseria meningitidis, whooping cough, rubella. |
| Airborne | Involves the transmission of small droplets (<5 nm), which contain the microorganism. These droplets can stay suspended in the air for long periods of time. | Tuberculosis, chickenpox. |
| Ingestion | Ingesting contaminated food, water or ice. Also person-to-person spread by the faecal–oral route. | Cholera, hepatitis A and causes of gastroenteritis, e.g., Salmonella. |
| Parenteral | Injection or inoculation, including needle-stick injury and sharing drug injecting equipment. | Blood-borne viruses, such as hepatitis B, hepatitis C and HIV. |
| Via vectors | Vectors, including mosquitoes, lice and ticks, transmit a microorganism via biting. | The commonest cause of malaria, the protozoa Plasmodium falciparum is transmitted via bites from infected female anopheline mosquitoes. |
| Vertical | Can be prenatal via the placenta, perinatal via the birth canal, postnatal via breastmilk. | Rubella can cross the placenta, Group B streptococcus birth canal, hepatitis B via breastmilk. |
Portals of entry are the routes that pathogens use to gain entry into the body6. Some portals are natural and always present, such as inhalation, ingestion or mucous membranes. Others, especially within health care settings, are temporary portals of entry. Surgical incisions, wound drains, urinary catheters, intravenous lines and endotracheal tubes can significantly increase a person’s risk of infection4.
Many factors influence the susceptibility of a potential host for acquiring infection and this is accentuated within health care settings. These include4
If all the components of the Chain of Infection are present, then infection can result.
FUNDAMENTAL PRACTICES FOR INFECTION CONTROL
Infection prevention and control centres on practices and procedures aimed at breaking the Chain of Infection. Some of these practices can be pre-emptive, such as the use of vaccination to prevent infectious diseases. Others, such as hand hygiene, can be practised on a regular basis to minimise the spread of infection4. Hands can easily become contaminated with microorganisms via contact with people, secretions, excretions, equipment and the environment8. Hand hygiene has been repeatedly supported by studies in the literature, and yet there is a continuing lack of compliance among health care workers with this effective infection-control measure9. Traditionally, hand hygiene is achieved by hand washing with soap or antiseptic solution and water. However, increasingly in heath care settings, the use of alcohol-based hand rubs/gels are advocated as a means of reducing the number of microorganisms carried on the hands8.
Other infection-control practices, which break the chain of infection include standard and transmission-based precautions, decontamination of equipment, safe sharps management systems, and the use of environmental and food hygiene practices4. The evolution of HIV and AIDS in the 1980s led to the development of universal precautions and body substance isolation, which are now combined as Standard Precautions and form the first tier in many infection control systems10. Standard precautions alert health care workers to patient situations that require special barrier techniques and aim to minimise the risk of infection transmission. The barrier techniques utilise personal protective equipment, such as gloves, gowns, nose, mouth and eye protection, when caring for all patients where actual or potential contact with blood or other body fluids may occur. In addition to standard precautions, infection control systems may also use transmission-based precautions when indicated for certain diseases. There are three types of additional precautions for specific infectious diseases spread by the following routes: airborne, droplet, and contact11,12.
Maintenance of clean environments and the decontamination of equipment using cleaning, disinfection and sterilisation are important components of any infection control management plan. In modern health care, there is an increasing role for ‘Single Use’ disposable items, which negate the need for reprocessing and minimise the risk of transmission. The use of guidelines and practices that promote safe management of indwelling medical devices, including urinary catheters and intravenous equipment, also contributes to the prevention of infection13,14.
VIRUSES
Viruses infect every form of life from animals and plants to bacteria and other microorganisms. Viruses are small, ranging in size from the poliovirus at 30 nm to large viruses such as vaccinia virus at 400 nm5. Structurally, viruses consist of a genome of either DNA or RNA (never both), which is packaged in a protein coat called a capsid2. The viral protein coat consists of repeating units known as capsomeres, and often has distinctive symmetry, such as icosahedral or helical structures5. Classification of viruses is based on three determinants: 1) the type of nucleic acid; 2) the structure and symmetry of the capsids of the protein coat; and 3) the presence or absence of an envelope3. This outer envelope is derived from the host cell membrane. Enveloped viruses are more susceptible to environmental factors, such as drying and gastric acidity, whereas envelope-free viruses are better able to survive in the environment5.
Viruses are unable to replicate independently and they rely on the biochemical machinery of their host’s cells to replicate – they are termed obligate intracellular parasites2. The capsid facilitates attachment and entry of the virus to the target host cells. The virus causes the host cells mechanisms to both replicate the viral nucleic acid and to synthesise new proteins for its capsid5. Following assembly of these viral components within the host cell, the new virus particle may be released in several ways. Some viruses cause cell lysis, a process where the host cell is destroyed, releasing the new virus2. In other infections, such as hepatitis B, the host’s cells are not destroyed, but release virus particles at a slow rate over time5.
The actual name given to viruses may originate from a characteristic of the virus, such as size, or after the locations where they were first isolated. For example, in the picornavirus, ‘pico’ means small; the poxviruses derive their name from causing conditions referred to as ‘poxes’ (e.g., smallpox); and the Coxsackie virus was named after Coxsackie, an area of New York2.
The outcomes of viral infection can vary substantially, ranging from unapparent infection, sub-clinical infection, and disease syndrome leading to death15.
VIRAL INFECTION: WHAT DOES IT MEAN?
Viruses can cause disease when they enter the body by breaching natural defences via several routes, including direct contact, injection, inhalation, and ingestion. The route of transmission will depend on the source of the virus. For example, the cold virus (rhinovirus) is transmitted via inhaled droplets, and by secretions coming into direct contact with the mucous membranes2.
The target tissue (tissue tropism) of the virus will determine the disease presentation and associated signs and symptoms. The manifestations of viral infection will vary from host to host and depend on both host and viral factors. Host factors (such as age, prior immunity, effectiveness of the immune response, and any treatment available) will influence the overall outcome. Features of the virus may enhance the virus’s ability to invade the host, evade local defences, spread within the host and replicate2.
WHAT IS THE PATHOPHYSIOLOGY?
Chickenpox or varicella is a common, highly infectious disease typically of childhood, caused by primary infection with varicella-zoster virus (VZV)3. VZV, a member of the herpesvirus family, causes two distinct diseases: varicella (chickenpox), and zoster (shingles). The latter results from reactivation of latent varicella. Varicella is a human disease with worldwide occurrence. Generally, varicella is regarded as a mild self-limiting disease in healthy children. However, complications can occur in children and especially in adults, neonates and immunosuppressed individuals of any age16.
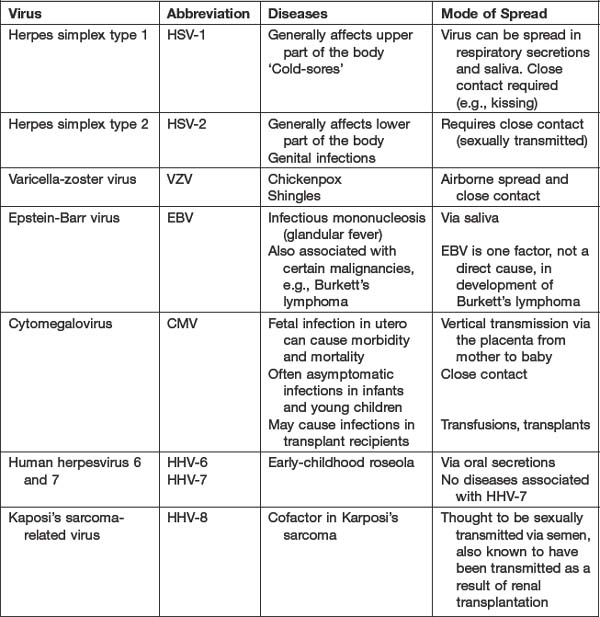
The herpesviruses are large, double-stranded DNA, enveloped viruses (see Table 2.3)17–19. Infections with herpesviruses are common and, while often associated with relatively mild disease, can cause significant morbidity and mortality, especially in immunosuppressed people. Latency is a feature of herpesviruses, with lifelong carriage of the virus following infection. As noted above, VZV (as a member of the herpesvirus family) establishes a latent infection in the neurons and subsequent reactivation results in a secondary infection, known commonly as shingles17.
VZV is transmitted from active cases to susceptible host by droplet or airborne spread of secretions from the respiratory tract of varicella cases, and from direct contact with contaminated secretions or the vesicular fluid from skin lesions of varicella or zoster cases. VZV enters via the respiratory tract or conjunctiva20. Primary infection with VZV initially begins in the mucosa of the respiratory tract and signs of disease are not present2,4. The virus spreads via the blood stream (primary viraemia) and the lymphatic system to the cells of the reticuloendothelial system, where replication of the virus occurs. After 11 to 13 days, a second viraemia spreads the virus primarily to the skin and respiratory tract, but extension to the mouth, conjunctiva and genitourinary tract is also possible2,4. VZV is highly infectious and humans are the only reservoir3.
Following primary infection with VZV and recovery, the virus demonstrates the latency associated with the herpesvirus family and lies dormant in the dorsal root ganglia. Subsequent reactivation of the virus results in the localised cutaneous eruption – herpes zoster or shingles21. The rash in herpes zoster is chickenpox. As in nature, it follows a dermatome with small closely placed lesions on an erythematous base2. The risk of shingles occurring is associated with changes to specific cell-mediated immune responses, such as may occur with ageing, and in immunosuppression. The rash of shingles is frequently painful in nature and postherpetic neuralgia, (defined as pain, which persists for more than thirty days from onset of rash) is a notable complication, more prevalent with increasing age21.
WHAT ARE THE CLINICAL MANIFESTATIONS?
The incubation period of VZV ranges from 10 to 21 days, most commonly 14 to 16 days2,15,20. There may be a prodromal illness, more frequently seen in adults, with fever, headache, and muscle aches. The rash is characteristic, appearing first on the trunk then the face and scalp. Presence of the rash on the scalp helps distinguish chickenpox from other illnesses2. Lesions start as flat macules, which rapidly become raised into small round papules that develop into fluid-filled, blister-like vesicles. Finally, these vesicles become pustular, then break down and crust over2,15,17.
A feature of the rash is ‘cropping’ with new lesions appearing in crops over several days, so that lesions of differing stages of development are present at any time. Chickenpox is contagious up to 48 hours before the rash appears and extends until all lesions are crusted and no new lesions occur (usually 5 days)22. Generally, chickenpox is a self-limiting illness, but complications can occur. The disease is often more severe in adults and this is believed to be attributable to heightened cell-mediated immune response, which produces greater cell damage2.
The most common complications are secondary bacterial infection of the vesicles with Staphylococcus aureus or Streptococcus pyogenes, which may warrant treatment with appropriate antibiotics. Secondary infection increases the risk of scarring from the lesions, as does trauma, such as scratching2. Severe disease can be seen in adults, neonates and immunosuppressed individuals, and pulmonary involvement may lead to respiratory failure, requiring mechanical ventilation. In addition, renal impairment, intravascular coagulation and altered liver function can occur and, in such cases, full supportive therapy and intravenous antiviral agents are indicated3.
Other rare complications include involvement of the neurological system in chickenpox infection (encephalitis), presenting as a cerebellar disturbance with ataxia (affecting coordination and speech) and the visual disturbance, nystagmus. These effects may persist for days or weeks, but are normally self-limiting with a good outcome3. A thrombocytopenia with a haemolytic rash and haematuria can occur, and this is usually transient, responding to corticosteroids therapy and platelet transfusion if required3.
In pregnancy, when the mother is non-immune, chickenpox can lead to severe morbidity in the mother, the fetus and in newborn babies. The complications of varicella pneumonia can occur in 10% of pregnant women with chickenpox, and its severity is greatest in the third trimester23. Chickenpox during pregnancy can result in fetal varicella, which occasionally causes ‘congenital varicella syndrome’. The effects include skin scarring, congenital malformations and other anomalies23. In Australia, the incidence of congenital varicella syndrome is one in 107,000 pregnancies24. Chickenpox occurring in pregnancy during the period five days before delivery to two days after delivery may result in severe varicella infection in 17% to 30% of newborns infants23.
WHAT SHOULD YOU BE LOOKING AT IN THE LABORATORY TESTS?
The diagnosis of chickenpox is usually based upon clinical presentation and laboratory diagnosis is not usually required20. If it is necessary to establish a diagnosis, then fluid or scrapings from the lesions can be examined using a fluorescent monoclonal antibody test. This test is sensitive, specific and will confirm the presence of VZV viral particles from the lesions24.
Laboratory tests are used to establish the presence of immunity to VZV. As the clinical disease is highly distinctive, a reliable history of chickenpox is a good indicator of past exposure and immunity20. A range of serological tests is available to detect immunoglobulins (antibodies), both IgG and IgM, to varicella-zoster virus. Recent or current infection is indicated by a positive IgM test. A positive test for varicella antibodies (IgG) indicates past exposure and immunity to VZV16.
WHAT IS THE TREATMENT?
Uncomplicated varicella infection in an immunocompetent child is a self-limiting disease. The aims of management will be symptomatic relief and prevention of complications. Symptom control may include the use of antipyretics, if pyrexial, and anti-pruritics to soothe itching25. Attention should be paid to skin care with bathing and regular changes of clothing and bed linens26. Fingernails need to be kept clean and short and itching discouraged to minimise the risk of secondary bacterial infection26.
While not recommended for routine use in uncomplicated cases of chickenpox, oral or intravenous antiviral therapy may be indicated for immunocompromised patients, and patients with complications including pneumonitis, and adolescents/adults26. Viruses, as obligate intracellular parasites, utilise the host cells machinery in order to replicate, complicating antiviral drug designs to limit toxicity to the host cell2. Several antiviral drugs, including acyclovir and famciclovir, are active against varicella virus17,25.
Prevention of varicella infection is possible with use of a live attenuated vaccine, which is approved for use in children over 12 months of age. It is recommended for use in non-immune adolescents and adults, especially those in high-risk occupations, such as health care workers and teachers20. The vaccine cannot be given during pregnancy. Vaccines generally contain a component of the microorganism, dead organism or modified live organisms, which stimulate the immune system to produce immunity without resulting in the disease process6.
In cases of high-risk, non-immune individuals having significant exposure to varicella, including non-immune pregnant women, zoster immunoglobulin (ZIG) may be used to give passive artificial immunity. Passive artificial immunity refers to the administration of antibodies (gamma globulin) derived, in the case of ZIG, from human plasma from blood donors. In contrast, passive natural immunity refers to the transfer of antibodies from mother to baby, across the placenta before birth, which gives protection to the baby for the first few months of life6. ZIG must be given to neonates whose mothers develop varicella (chickenpox) from seven days or less before delivery and up to 28 days after delivery, because its use can prevent or lessen the effects of varicella in the newborn period. ZIG must be given as soon as possible, but must be within 72 hours of exposure for optimal effect23. Use of ZIG is highly effective but supplies are limited.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree