7
Infection prevention and control in the community
• To enable the student to gain an understanding of infection control measures as they apply within the community placement environment
• To enable the student to gain an understanding of the principles of infection prevention
• To enable the student to use their developing knowledge and skills of infection control in the community through focusing on the specific prevention and control of infection in wound care
Introduction
Healthcare-associated infections (HCAIs or HAIs) are infections that are acquired in a hospital or other healthcare setting, such as a hospice or care home, or as a result of a healthcare intervention or procedure (Turner 2008). They pose a significant threat to the safety of patients and the public. Consequently, policies and procedures for the control of infection are a major concern to the NHS and a particular area of responsibility for all practitioners within all aspects of care. It is important to note here that this does not only apply to what may be called adult nursing placements, but those related to children’s nursing, where more children are also being cared for in the home. Patients suffering from mental health can also be at risk of infection from issues such as self harm. Students who are learning in mental health nursing placements (Stacey et al 2012) may also be called upon to administer care with their mentors for patients with mental health problems who have been discharged home following surgery. Collaborative working with the district nurse in such situations is essential to ensure holistic care of the patient.
• identify and take effective measures to prevent and control infection in accordance with local and national policy
• maintain effective standard control of infection precautions and apply and adapt these to needs and limitations in all environments
• provide effective nursing interventions when someone has an infectious disease including the use of standard isolation techniques
• fully comply with hygiene, uniform and dress codes in order to limit, prevent and control infection
• safely apply the principles of asepsis when performing invasive procedures and be competent in aseptic technique in a variety of settings
• act, in a variety of environments including the home care setting, to reduce risk when handling waste, including sharps, contaminated linen and when dealing with spillages of blood and other body fluids.
A variety of key personnel are specifically involved with infection prevention and control. For example, infection control nurses are specialists in infection prevention and control and provide advice on infection prevention and control in hospital and in the community.
Hospital infection control teams provide an infection control service for the hospital, which can also include community hospitals. These teams are often led by a nurse consultant in this field and a lead consultant microbiologist. Infection control link personnel are normally employees working in a surgery or care home who have completed additional training in infection control and act as a link between the workplace and the infection control nurse. Environmental health officers work for local authorities and advise on food safety, pest control and waste disposal. The Public Health departments in many community health organisations play a key role in the prevention and control of infection across the community as a whole, including areas such as child care centres (Health Protection Scotland 2012: http://www.documents.hps.scot.nhs.uk/hai/infection-control/guidelines/infection-prevention-control-childcare.pdf – accessed July 2012.)
Lawrence and May (2003) outline a checklist of questions which can help the nurse with control of infection in the home; this includes the following:
• Has the client been discharged from hospital recently and if so, did they have any infections during their stay?
• Is there a history of known infections/antibiotic treatment?
• What other services are involved with care?
• What procedures need to be carried out in the home?
• Can hands be washed in the home?
• Is there adequate storage space in the home for necessary equipment?
• Are there any other family members ill or immunocompromised?
Normally, discharge from hospital will be planned and the community nurse will have been given sufficient time to make appropriate arrangements to enable continuity of care; in some cases, a home visit may have been organised for example before surgery, enabling the above questions to be addressed.
Standard infection control precautions
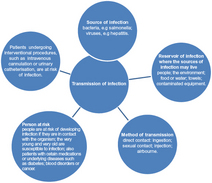
The practice of standard infection control precautions aims to prevent the transmission of infection. Potential sources of infection include blood and body fluids or excretions and any equipment in the care environment that could become contaminated. Figure 7.1 outlines the ways in which infection can spread. It is important that you learn about this process and most importantly, the physiological aspects of infection and its causes and outcomes.
It is essential that all practitioners carry out standard infection control precautions at all times, irrespective of whether infection is present or not and irrespective of the setting in which they are caring for their patients. However, compared with the hospital setting, it can be challenging to practise all standard infection control precautions to the same high standard and in some community contexts, the risks are very different. For example, risks such as cross-infection between people in close proximity as in a hospital ward are significantly reduced in the home but it is also more difficult to control the environment when it is a person’s home. The elements of standard infection control precautions are listed in Table 7.1. It is also important to include the patient’s family and/or immediate carer in any risk assessment of infection and how to prevent it happening. Patient education will often include the family member or carer, especially when the patient is unable to undertake any procedure necessary.
Table 7.1
Elements of standard infection control precautions
Patient positioning
Hand hygiene
Respiratory hygiene
Personal protective equipment
Occupational exposure management including sharps
Management of care equipment
Safe care of linen including uniforms
Control of environment
Management of blood and body spillages
Safe waste disposal
Hand hygiene
Handwashing is an essential component in the prevention and control of infection and regular careful handwashing is vital when you are looking after someone at home. However, within someone’s home, hot and cold running water might not always be readily available. Community nurses therefore carry alcohol hand rubs/alcohol hand gel and tissues to address this problem but it must be remembered that this must be accompanied by an appropriate hand decontamination technique. (See an online example of this technique at the CETL website: http://www.cetl.org.uk/learning/hands/hand-washing/data/downloads/print-sheet.pdf – accessed October 2012.)
In your initial preparation for clinical practice, you will have received specific instructions on how to wash your hands, covering all the surfaces of your hands including the tips of your fingers, your thumbs and the areas between the fingers. It is essential to explain the risks associated with poor hand hygiene to service users and carers and educate them to undertake effective hand hygiene, particularly within the home setting, when an informal carer may be delivering the majority of nursing care. (See an example of information for patients and carers to use in the home at the Stroke4Carers website: http://www.stroke4carers.org/?p=5086 – accessed October 2013)
Personal protective equipment
The main purpose of protective clothing is to prevent the spread of potentially pathogenic micro-organisms to another client, preventing contamination of the nurse’s uniform or clothing (NICE 2003). It is important that you adhere to the local policy and protocols regarding protective clothing such as gloves and aprons.
Sharps management
• Never re-sheathing needles after use
• Disposing of syringes and needles as one complete unit immediately after use
• Never leaving sharps lying a round
• Ensuring secure closure of sharps boxes after three quarters full
• Storing sharps container in a secure place out of the reach of others.
Remember also that inoculation can also occur if abrasions, cuts or scratches are exposed to blood or body fluids. Within their everyday work, nurses risk exposure to dangerous viruses such as hepatitis as a result of needle stuck injury (RCN 2009).
• Encourage bleeding from the inoculation site and wash under running water
• Cover with a waterproof dressing and report to a senior member of staff on duty
• Inform occupational health, GP (or visit accident or emergency) and client’s carer
• Assess risk of hepatitis B and C or HIV
• Obtain relevant blood samples from source and recipient with informed consent
• Seek specialist advice if there a need for post-exposure prophylaxis or follow-up for Hepatitis B and C or HIV?