Chapter 25 INFECTION PREVENTION AND CONTROL
Nurses, together with all health care workers, share the responsibility of preventing the spread of infection between themselves and clients and between one client and another. Clients in health care settings are at risk of acquiring infections because of lowered resistance and increased exposure to microorganisms. Sources of infecting microorganisms can be people or environmental objects, such as medical or nursing equipment that has become contaminated.
MICROORGANISMS AND INFECTION
TYPES OF MICROORGANISMS
Bacteria
Bacteria are single-celled microscopic organisms without a nucleus that have the capacity to reproduce rapidly. Bacteria may be classified by reactions to laboratory techniques and by their appearance. Gram-staining, growing bacteria by culture and sensitivity testing are some of the laboratory techniques that identify bacteria and determine which antibiotic will be effective against them. Gram-staining involves placing live bacteria onto a microscope slide then applying methyl violet followed by iodine solution. The cells are stained blue at this stage. They are then treated briefly with acetone. Bacteria that retain the original blue stain are Gram-positive. Gram-negative cells are de-colourised by the acetone and appear red (Wilson 2000). Gram-negative bacteria are the more dangerous because they produce an endotoxin that can cause haemorrhagic shock and severe gastrointestinal disturbance, such as acute diarrhoea. They also lower the client’s resistance to other pathogens, making them susceptible to other different infections.
To culture (grow a sample of) bacteria, a sample from the client is transferred to growth medium, such as nutrient agar, that promotes multiplication and growth. When bacteria are present in sufficient quantity, sensitivity tests are carried out to determine the appropriate antibiotic to prescribe (deWit 2005).
Some species of bacteria have the ability to develop highly resistant round or oval structures, called spores, when they are exposed to adverse conditions such as lack of nutrients and/or water. Spores are resistant to disinfectants and to high or low temperatures, so they are difficult to destroy. They are resistant to sunlight and even freezing conditions so may remain viable in adverse environments for many years. They germinate when the environmental conditions become favourable, and this allows the bacterial cell within to begin multiplying (Wilson 2000).
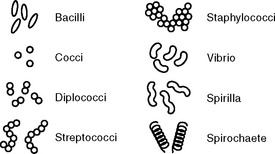
Bacteria appear in a variety of sizes, shapes and arrangements. There are three main shapes — rod shaped (bacilli), round (cocci) and spiral shaped (spirilla, vibrios and spirochaetes). Figure 25.1 provides examples of bacterial shapes.
Diseases caused by cocci include meningitis, gonorrhoea, pneumonia and skin infections such as boils and impetigo; diseases caused by bacilli include tetanus, diphtheria, tuberculosis (TB) and Legionnaires’ disease; the disease most commonly caused by spirochaete infection is syphilis. Different kinds of bacteria tend to affect different organs and systems of the body, producing a range of infectious diseases, each with its own group of symptoms. Bacteria make up the largest group of pathogens and are usually treated with antibiotics. The advent of antibiotics in the 1940s provided a powerful weapon to treat bacterial infections; however, because bacteria continually mutate as they divide, some had natural resistance to the effects of antibiotics and have developed into resistant strains. These pathogens include methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus (VRE) and penicillin-resistant Pneumococcus. These multi-drug-resistant organisms are dangerous threats, and emphasise the need for nurses and all health care workers to practise effective infection prevention and control measures (Wilson 2005).
Rickettsiae and Chlamydiae are microorganisms classified as specialised bacteria but they are smaller than most other bacteria and can only reproduce within the living cells of a host. Organisms that can only multiply within living cells are called parasites. Rickettsiae are often carried by arthropod vectors such as fleas, ticks and lice. A vector is the term used for a carrier that transfers an infective agent from one host to another. Body lice, for example, are arthropod vectors that carry the Rickettsiae responsible for epidemic typhus. Arthropods are creatures with jointed legs and include insects and ticks. Arthropods that live on the body’s surface (skin and mucous membranes) are called ectoparasites. Ectoparasites are responsible for conditions such as scabies and head or pubic lice (see Chapters 27 and 37 concerning nursing care for these conditions).
Mycoplasmas are a type of ultramicroscopic bacteria that lack a cell wall. They are responsible for some respiratory and genital-tract infections in humans. Mycoplasma pneumoniae causes a virulent type of pneumonia that spreads via respiratory secretions and is transmitted slowly but easily between humans (Wilson 2005; Wilson 2000).
Viruses
Viruses are specialised microorganisms with a number of distinctive characteristics:
The major viral diseases of concern within the health care setting are infectious mononucleosis (glandular fever [Epstein–Barr virus infection]), cytomegalovirus infection, herpes simplex virus infection, viral hepatitis (hepatitis A, B and C viruses), influenza, measles, human immunodeficiency virus (HIV) infection, respiratory syncytial virus infection, rotaviral enteritis, chickenpox (varicella virus), shingles (herpes zoster virus), rubella (German measles), viral haemorrhagic fevers and, most recently, severe acute respiratory syndrome (SARS, caused by a novel coronavirus) (Lashley & Durham 2007; Wilson 2005; Wilson 2000).
Fungi
Fungi are tiny organisms such as moulds and yeasts that belong to the world of plants but contain no chlorophyll. Fungi are present in the soil, air and water and they multiply by producing various kinds of spores. Most species of fungi are non-pathogenic, but a few cause disease. There are three types of fungal (mycotic) infections: superficial, which affect the skin, mucous membranes, hair and nails; intermediate, which affect subcutaneous tissues; and systemic, which infect deep tissues and organs. Tinea (ringworm) is one genus of the fungal group of organisms called dermatophytes. Tinea species cause superficial infections of the keratin found in skin, scalp and nails. Sometimes antibiotic medications alter the body’s normal flora, providing an environment that allows fungal infections such as vaginal candidiasis (vaginal thrush) and tinea pedis (athlete’s foot) to develop (Wilson 2000).
Protozoa
Some protozoans are transmitted by insects (vectors) to man. Pathogenic protozoa include the plasmodium species, which is carried by mosquitoes and causes malaria. Malaria still causes over three million deaths each year in the more tropical regions of the world (Herlihy & Maebius 2000). Certain strains of protozoa are a major cause of opportunistic infections, meaning that they take the opportunity to establish themselves in a host whose resistance is lowered. For example, Pneumocystis carinii is commonly the cause of pneumonia in people with acquired immune deficiency syndrome (AIDS), whose immune systems are weakened by the presence of the AIDS virus (HIV) (Lashley & Durham 2007).
Helminths
Roundworms include ascarides, hookworms, trichinae, pinworms and a minute worm that causes filariasis (elephantitis). Pinworm is one of the most common parasitic worms. It affects children more often than adults. This nematode is less than a centimetre long and inhabits the upper part of the large intestine, but lays its eggs on the outer perianal area of the host. The deposition of the eggs causes irritation, the child scratches, hands are contaminated and eggs are transferred from hand to mouth and sometimes to friends. This circular pattern of reinfestation makes pinworm particularly hard to control (King, Belman & Kramer 2001).
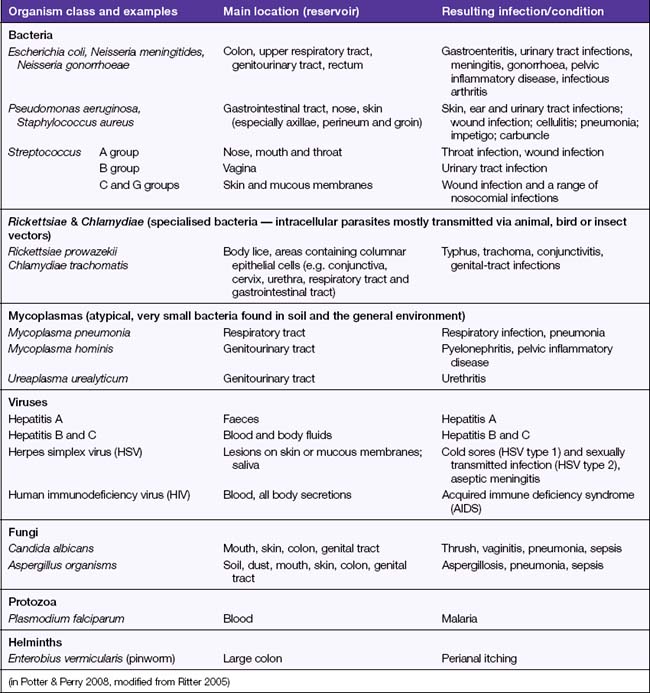
The diagnosis of worm infestation is made by microscopic examination of the client’s faeces, which reveals the presence of adult worms or their larvae. Infestation by parasitic worms is treated with medications called anthelmintics (Bryant, Knights & Salerno 2006). Education of clients regarding prevention of spread and reinfestation is essential. Table 25.1 provides a list of common infection-causing organisms.
CHAIN OF INFECTION
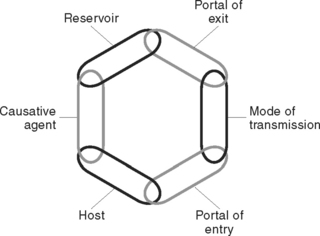
Figure 25.2 illustrates the chain of infection. Infection prevention and control is directed towards breaking the links in the chain of infection.
RESERVOIRS (SOURCES) OF INFECTION
The reservoirs of pathogenic microorganisms are human, animal or inanimate sources. A reservoir is a place where a pathogen can survive but may or may not multiply. The presence of microorganisms does not always cause a person to be ill. In humans, microorganisms can thrive in reservoirs such as open wounds, nasal passages, skin crevices and in the blood.
Human sources
Most organisms that infect humans are acquired from human sources. A variety of organisms, normal flora, reside on the surface of the skin and within body cavities, fluids and discharges. Some areas of the body contain larger populations of normal flora than others, for example, the skin, respiratory tract, colon, mouth and vagina. Areas of the body that are usually considered sterile (without normal flora) include the spinal fluid and blood, the urinary system and the peritoneal cavity. The entrance of a foreign object or organism into a sterile site leads to a high risk of infection. Auto-infection occurs when normal flora cause infection by being transferred from their normal place of residence to a different site in the same host. Crossinfection may occur when organisms from one person are transferred to another person, for example, when organisms on a nurse’s hands are transferred to a client’s wound.
A person with an infection can liberate large numbers of pathogens into the environment. In some diseases the risk of infecting others may last only a short time; in others, pathogens continue to be released by the infected person over a long period; for example, the tuberculosis Mycobacterium may be present in the host for many years (Wilson 2000; Wilson 2005).
PORTALS OF EXIT FROM THE RESERVOIR
Urinary tract
When there is an infection of the genitourinary tract, microorganisms can exit via the urine.
MODES OF TRANSMISSION
Contact transmission
This is the most significant route of transmission in health care settings (Wilson 2000). Microorganisms can be transferred directly from one individual to another by physical contact between an infected person and a new host. Contact transmission can occur by touching the skin or body fluids of a client with an infection, or through the use of contaminated nursing or medical equipment. The hands can be the means of transfer if, after contact with an infectious client, they are not washed adequately before tending another client. Effective hand washing is the single most important way to limit cross-contamination and the spread of infection. Cross-contamination is said to have occurred when pathogens have been transmitted from one person or object to another. Contact transmission can also occur as a result of sexual activity or from a mother to an unborn baby via the placenta (transplacentally).
Transmission by ingestion
PORTALS OF ENTRY
Microorganisms can enter the body through the same routes they use for exiting:
RESISTANCE TO INFECTION
NON-SPECIFIC DEFENCE AGAINST INFECTION
External mechanical and chemical barriers
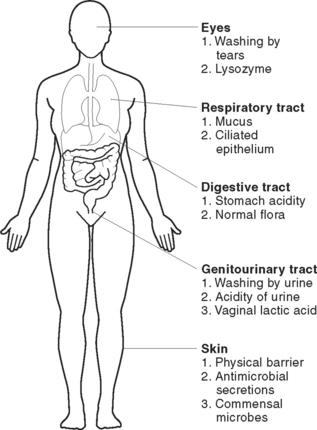
These are the natural physical barriers that prevent microorganisms from entering the body or expel them before they proliferate. Physical barriers include the skin, mucous membranes, normal body flora and some body secretions (Figure 25.3).
The respiratory tract is protected by mucous membrane. The membrane of the upper airway is lined with hair-like structures called cilia, that waft inhaled microorganisms away from the lungs and into the oropharynx to be expectorated or swallowed. Nasal secretions, like saliva, also contain lysozyme.
Protective proteins
There are two groups of protective proteins — complement proteins and interferons. Complement comprises a set of about 20 proteins that help phagocytic cells identify pathogens. They do this by a series of reactions that eventuate in a protein substance, called C3b, coating the surface of the pathogens. Phagocytic cell receptors are able to recognise this substance, bind to it then ingest the pathogen. They are also involved in destroying foreign bacteria by a process called cytolysis. The complement achieves this by first changing the shape of the bacteria to a doughnut shape, then making a hole through the cell membrane. This permits ions and water to enter and swell the cell until it ruptures (Crisp & Taylor 2005).
Interferons are a group of proteins secreted by cells infected with a virus. They are capable of binding onto other surrounding cells and protecting them from viral replication. They are also able to enhance the destructive abilities of NK cells against malignant tumour cells. All cells can produce alpha and beta interferons, which interfere with the replication of viruses. T lymphocytes and NK cells can produce gamma-interferon, which coordinates and enhances the activities of other parts of the immune system (Wilson 2000).
SPECIFIC DEFENCES AGAINST INFECTION: IMMUNITY
Having immunity is the situation of being resistant to, or being unaffected by, a particular infectious disease. It means that a specific antibody has been produced to defend the body against a specific pathogen or the toxin it produces. An antigen is the term used for any foreign material, including bacteria, viruses or toxins, that stimulates an immune response in the body (Wilson 2000). Antibodies are proteins synthesised by the host that inactivate antigens. Tissues from another person, such as incorrectly matched blood or a donor organ, can also be antigens, causing an antigen–antibody response in a recipient host. The antigen–antibody response is a very specific defence because it always involves one specific antibody striving to combat one specific type of antigen. When antibodies directly react against, interact with or bind to antigens, an antigen–antibody reaction is said to have occurred. Mostly the antigen–antibody response is an important mechanism that promotes human survival. On some occasions it can cause problems; for example, an overreaction to an antigen can cause hypersensitivity and an allergic reaction such as is seen in hay fever, in people particularly allergic to bee stings, and sometimes in people who are allergic to particular medications.
The lymphatic system
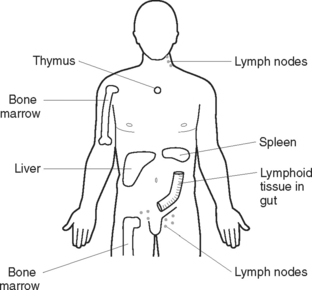
The body’s immune responses are under the control of the lymphatic system. It is a highly efficient system that responds very specifically to the threat of infection. It is made up of lymph, lymphatic vessels, lymph nodes, red bone marrow, the thymus gland, spleen and tonsils. The immune system develops when lymphoid stem cells are manufactured in the red bone marrow and travel to the thymus gland, spleen and other lymphoid tissues and organs in the body. These organs and tissues are coordinated to produce, mature and activate cells effective in providing the body with its immune response (Bryant et al 2006). Lymphocytes are the most significant cells in the body’s immune responses.
Lymphocytes
There are two categories of lymphocytes involved in the specific immune response — T lymphocytes (T cells) and B lymphocytes (B cells). They reside in areas of lymphoid tissue around the body (Figure 25.4) and circulate in the blood. It is the job of T cells and B cells to attack antigens. Fetal stem cells in the bone marrow initiate production of T cells and B cells. T cells travel and mature in the thymus gland. B cells do not travel to the thymus gland and mature and differentiate in fetal blood or bone marrow. After maturing, both types reside in various lymphoid tissue around the body and also circulate in the blood. T cells comprise 70–80% of circulating lymphocytes, B cells comprise the other 20–30%.
Recognising ‘self’ cells
To function effectively at defending the body from invading organisms, these defence responses must be able to distinguish between the body’s own cells and foreign agents. During the period between life as a fetus and several years after birth, the thymus gland is busy setting up the antibody response system. During this process T cells are maturing. To enable the process of identifying cells that belong to the ‘self’ and should not be attacked, markers are placed on the outer surfaces of the body’s own cells. The marker is a group of molecules called the major histocompatibility complex (MHC). Each person has their own unique MHC. This accounts for why the body recognises and attacks tissue or organs donated from others. Any T cells that recognise and respond to ‘self’ cells are discarded.
Cell-mediated immunity
Two types of T cells are involved in cell-mediated immunity: T-helper (CD4) cells, and cytotoxic T cells. Cell-mediated immunity is particularly effective against fungi, protozoan parasites, malignant cells and foreign tissue that is alien to the body, for example, transplanted organs (Herlihy & Maebius 2000). The following steps are involved in cellular immunity:
Antibody-mediated (humoral) immunity
It is mostly B lymphocytes that are involved in the antibody-mediated response. Each B cell is programmed to produce a unique antibody. Each B cell displays its own specific antibody on its outer surface. This acts as a receptor for passing antigens. Antibodies only bind with antigens that specifically fit their unique receptor — the antigen must have a shape that precisely fits the antibody, rather like the way two pieces of a jigsaw puzzle fit together. B cells produce vast quantities of specific antibodies to lock with, then generate a reaction against, specific antigens. Antibodies are gamma globulins, one subtype of a class of proteins called immunoglobulins. Immunoglobulins are classified into five identifiable groups: IgG, IgM, IgA, IgE and IgD. Table 25.2 describes some specific properties of each class of immunoglobulin. Between them they perform these general tasks:
TABLE 25.2 FUNCTIONS OF THE FIVE CLASSES OF IMMUNOGLOBULINS
The following steps are involved in antibody-mediated immunity:
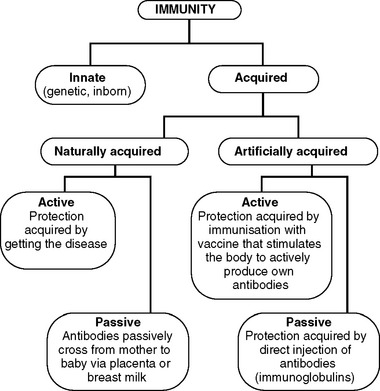
Naturally acquired immunity
Active natural immunity occurs after being exposed to an infectious organism and developing specific antibodies and many memory cells to ward off future encounters with the same pathogen. Active immunity is acquired as a result of the stimulation of an individual’s immune system, with active involvement of the body in the production of its own immunoglobulins. For example, if measles, mumps or chicken pox is experienced as a child, active natural immunity to these illnesses is established.
Artificially acquired immunity
Specific vaccines provide protection against some infectious diseases for months or years. It is recommended that vaccination against many diseases be provided at a very young age; for example, Sabin vaccine, which is ingested orally, provides protection against poliomyelitis, and the first dose should be given when a child is only 2 months old. (For further information about vaccination, refer to the Immunise Australia website www.immunise.health.gov.au.)
Worldwide immunisation programs have eradicated or substantially reduced the incidence of smallpox, diphtheria, tetanus, whooping cough and poliomyelitis. Nurses can promote the health of the community by providing education about immunisation programs. It is strongly recommended that nurses access all available immunisation protection from diseases they may themselves be exposed to, in particular TB and hepatitis A and B. Figure 25.5 indicates the different types of immunity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree