SUBJECT KNOWLEDGE
• Routes of spread of infection
• Physical and physiological aspects of infection control
• Risk management
• Influences of behaviour, attitude and culture
• Epidemiology of infection
• Health promotion
CARE DELIVERY KNOWLEDGE
• A problem solving approach to infection control
• Standard precautions
• Principles of:
– Hand hygiene
– Disposal of healthcare waste, sharps and linen
– Wearing personal protective equipment
– Maintaining a clean environment
– Aseptic technique
– Personal care
PROFESSIONAL AND ETHICAL KNOWLEDGE
• Professional, ethical and political issues
• Roles of specialist teams in hospital and community
PERSONAL AND REFLECTIVE KNOWLEDGE
• Four case studies related to the four branches of nursing
INTRODUCTION
The prevention of spread of disease caused by infection is fundamental to all nursing care, and is an essential part of all health care in hospital and community settings. With the rise of healthcare associated infections, all healthcare professionals have a key role to ensure that infection control procedures and practices are implemented, both to prevent patients from acquiring an infection and to protect healthcare staff from infection (Wilson 2006).
Infectious diseases have been a threat to health and well-being since human life began, with outbreaks of infection over the centuries often generating great fear in people. Just over 100 years ago the science of microbiology was born when the relationship between disease and microorganisms was discovered by Louis Pasteur. In Britain, major infectious diseases kill only a small number of people compared to the past, but across the world the diseases of HIV/AIDS, tuberculosis and malaria account for millions of deaths each year (World Health Organization 2004).
Today, despite modern healthcare having saved countless lives, infectious diseases remain a massive global threat. Alongside the emergence of new diseases such as AIDS, variant Creutzfeldt–Jakob disease and severe acute respiratory syndrome (SARS), there has been the re-emergence of old diseases such as tuberculosis (Wilson 2006).
In the UK there are two particular infection control challenges in hospital care which cause deaths, impede recovery and make frequent headline news: the increasing number of healthcare associated infections (HCAI) and antibiotic resistant bacteria. Most notably these infections are caused by meticillin(methicillin)-resistant Staphylococcus aureus (MRSA), often described as a ‘superbug’, and Clostridium difficile. Infection prevention and control in the community is a key service within public health. As with hospitals, MRSA and C. difficile are being increasingly noted within the community as patients are discharged from hospital with these infections (Lawrence and May 2003).
Infection prevention and control must be a priority for all healthcare staff and should underpin quality clinical practice across all areas of health care. With the current challenge to both hospital and community staff of increasing antimicrobial resistance, healthcare staff can no longer rely on treating organisms with antibiotics; instead healthcare staff need to concentrate again on the basics – proven infection control procedures.
Nurses of all branches have a role to play with their specific patient or client groups. Whether nursing in an institution (hospital or nursing home) or in the community (individual homes, health centres or shared housing), nurses must recognize the sources and modes of spread of infectious microorganisms and understand how to apply evidence-based practice to prevent and control infection.
OVERVIEW
This chapter aims to provide you with an understanding of what infection prevention and control means for individual people (sick or well) and their carers (health professional or informal family and friends), whether this care is in a home or community setting or in a hospital or institution.
Subject knowledge
This section introduces the biological aspects of infection, including the four main groups of microorganisms (bacteria, viruses, fungi, protozoa), routes, modes of spread and sources of physiological and physical control.
The complex psychosocial issues related to the prevention and control of infection are considered, with particular reference to the influence of personal and group behaviour, attitude and culture. Epidemiology and its importance in the identification and control of infection, with particular reference to health promotion, is included.
Care delivery knowledge
A range of nursing practices is explored using a problem solving approach of assessment, planning, implementation and evaluation. Both standard precautions (Royal College of Nursing 2005) and specific practices to prevent and control infection are considered.
Professional and ethical knowledge
Professional accountability is highlighted with specific sections on ethical and political issues. The roles of the infection control team in the hospital and the environmental health team in the community are considered.
Personal and reflective knowledge
Throughout the chapter there are decision-making exercises and suggestions for reflection and portfolio evidence. Case studies related to each branch of nursing are included here to encourage reflection upon practices you have observed and material you have learned from this chapter.
SUBJECT KNOWLEDGE
BIOLOGICAL
CLASSIFICATION OF INFECTIVE AGENTS
An infection is caused by the invasion of a person’s immunological defences by microorganisms that actively cause harm to body tissues (Wilson 2006). Bacteria, viruses, fungi and protozoa are the four main groups of organisms capable of causing disease (Box 5.1). Protozoa are not commonly encountered in the healthcare environment today (Wilson 2006).
Box 5.1
| Organism | Infections and diseases |
|---|---|
| Bacteria | |
| Gram positive | |
| Staphylococcus aureus | Wound infections, pneumonia, osteomyelitis, food poisoning |
| Staphylococcus epidermidis | Wound infection, associated with invasive plastic and metal devices, e.g. IV cannulas |
| Streptococci (group A) | Streptococcal throat, impetigo, rheumatic fever, scarlet fever |
| Streptococci (group B) | Urinary tract infection, wound infection, meningitis |
| Streptococcus pneumoniae | Pneumonia, bronchitis, meningitis, otitis media |
| Enterococci | Urinary tract infection, wound infection |
| Mycobacterium tuberculosis | Tuberculosis |
| Clostridium tetani | Tetanus |
| Clostridium difficile | Diarrhoea, hospital acquired gastrointestinal infections |
| Listeria | Premature delivery, septicaemia and meningitis in neonates |
| Gram negative | |
| Neisseria gonorrhoea | Gonorrhoea, pelvic inflammatory disease, conjunctivitis, infective arthritis |
| Neisseria meningococcus | Meningococcal septicaemia |
| Pseudomonas | Wound infections, chest infections |
| Legionella | Chest infection, legionnaires’ disease |
| Escherichia coli | Wound infections, urinary tract infection, pelvic inflammatory disease |
| Salmonella | Food poisoning |
| Acinetobacter | Urinary tract infection, wound infections, respiratory infections |
| Campylobacter | Diarrhoea, gastroenteritis |
| Helicobacter pylori | Gastritis, gastric ulcers |
| Chlamydia | Trachoma, non-specific urethritis in males |
| Viruses | |
| Hepatitis A | Infectious hepatitis |
| Hepatitis B | Serum hepatitis |
| Hepatitis C | If chronic – liver disease and cirrhosis |
| Herpes (type 1) | Cold sores, sexually transmitted disease |
| Herpes (type 2) | Genital lesions |
| Human immunodeficiency | Acquired immunodeficiency syndrome (AIDS) |
| Enterovirus | Poliomyelitis |
| Epstein–Barr | Glandular fever |
| Virus-like prions | Creutzfeldt–Jakob disease (CJD) |
| Fungi | |
| Candida albicans | Vaginal thrush, urinary tract infection |
| Tinea | Athlete’s foot, ringworm |
| Protozoa | |
| Trichomonas vaginalis | Sexually transmitted disease in women |
| Plasmodium falciparum | Malaria |
| Entamoeba | Amoebic dysentery |
Bacteria are the most common cause of HCAI with viruses considered to be the most common condition in the community, e.g. influenza, common cold. However, not all microorganisms cause infection or disease. Many live quite harmlessly in soil, water, air; and in alcohol and cheesemaking (yeasts). Some bacteria are vital in the production of antibiotics.
Microorganisms capable of causing disease are called pathogens, but the presence of a pathogen does not necessarily mean that an infection will ensue. The surface of the body is densely populated by a wide variety of microorganisms and every day the intestinal system excretes millions of microorganisms. Pathogens that live on their host in a specific body site without causing harm are called commensals and are often described as the normal flora of the body. They only become pathogenic and cause an infection when transferred to an abnormal body site. For example, MRSA is commonly found to be colonized in the nasal mucosa and can live there harmlessly, but organisms from the nose can be easily transferred to other body sites, such as wounds, therefore in some instances it is recommended that patients are decolonized prior to surgery to prevent surgical wounds becoming infected with MRSA (Wilson 2006).
SOURCES OF INFECTION
Bacteria
Bacteria are unicellular organisms that evolved millions of years ago. They are visible under the high magnification of an ordinary light microscope using an appropriate stain. Surrounding the bacterial cell is a membrane made up of proteins and phospholipids and surrounding the membrane is a hard cell wall, which gives the organism its shape.
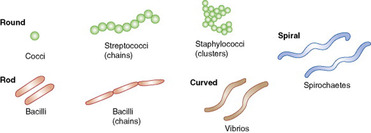
Bacteria are most commonly classified by their shape (Fig. 5.1) and their response to a laboratory reaction when treated with a dye called Gram’s stain. The response is determined by a chemical present in the bacteria’s cell wall. Bacteria are termed gram positive if they stain blue/purple and gram negative if they fail to take up the stain and remain the red colour of the counterstain.
 |
| Figure 5.1 |
Wilson (2006) states there are four main groups of bacteria: gram positive cocci and bacilli and gram negative cocci and bacilli, with other important groups including acid-fast bacilli, spirochaetes and atypical bacteria (see Box 5.1).
MRSA is an example of a gram positive coccus, and as with all bacteria has the potential to cause a whole range of infections including those of the lungs, wounds and urinary tract. More detail regarding specific bacteria, including the increasing problem of antibiotic resistance and methods used to prevent the spread of infection, are included in the Care Delivery section of this chapter.
Some bacteria have the ability to form spores to allow them to survive for longer when environmental conditions are not suitable for their cells to multiply. An example of this is Clostridium difficile, responsible for antibiotic-associated infections of the gastrointestinal tract.
Viruses
Viruses are not cells but minute particles consisting of genetic material and protein. Each virus is a piece of nucleic acid that is protected by a protein coat or lipid membrane. Viruses are not usually defined as a living organism, and instead of growing and dividing like cells, they infect cells. For example, the human immunodeficiency virus (HIV) infects human T cells of the immune system; while viruses that cause the common cold attach themselves to the epithelial cell membrane and invade the cell, releasing new virus particles and destroying the host cell. Viruses are extremely small and can only be seen with a high-powered electron microscope. Unlike bacteria, most viruses are very fragile and cannot survive outside a living cell for very long. Viruses are fairly resistant to disinfectants, such as chlorhexidine, which are unable to penetrate the protein coat or lipid membrane.
There are many viruses (see Box 5.1), of which a number, primarily those transmitted by blood and body fluid, are of particular importance for nurses and other healthcare workers. They are referred to in some detail within the Care Delivery section of this chapter.
Prions
Prions – virus-like agents – are abnormal proteins that contain no nucleic acid. They are unique among microbes and appear to cause disease by replacing normal proteins on the surface of host cells and then gradually compromising their function. The main prion disease in humans in the UK is Creutzfeldt–Jakob disease (CJD), although scrapie, a prion disease in sheep, has been known for centuries. CJD is associated with the destruction of brain tissue. In 1996 a new form of CJD was found called variant CJD (vCJD) which generally affects young people under the age of 30. These cause a range of unusual neurological symptoms and it is likely that such cases are linked to exposure to bovine spongiform encephalitis (BSE) (Wilson 2006). Prion proteins are highly resistant to conventional methods of decontamination, including heat and many chemical disinfectants.
Fungi
Fungi have a more complicated structure than bacteria and contain a nucleus. They are either branch shaped (e.g. mushrooms) or form buds (e.g. yeasts). There are over 700 000 species but few are pathogenic (see Box 5.1).
Candida, the yeast that is responsible for causing thrush, destroys the normal bacteria of the area it infects, namely the mouth, large bowel and vagina. The most common, C. albicans, causes vaginal thrush. Tinea is a fungus that produces a superficial infection. It is responsible for athlete’s foot, causing a painful and irritant rash in the folds of skin, most commonly between the toes. Deeper fungal infections are more common in hot climates.
Protozoa
Protozoa are microscopic single-celled animals (see Box 5.1), and although unusual in the UK, they are very common in other parts of the world. Associated with poor sanitation, UK cases are often acquired from abroad. Two pathogens found in the UK are Cryptosporidium, a water borne pathogen which is a common cause of gastroenteritis in children under the age of 5 years, and Trichomonas vaginalis, a sexually transmitted infection which causes a foul-smelling, green–yellow vaginal discharge (Wilson 2006). Malaria, caused by the protozoon Plasmodium falciparum, remains an endemic disease in many parts of the African, Indian and Asian continents. Although malaria does not occur in the UK, nearly 2000 cases are reported in travellers returning to the UK each year (Health Protection Agency 2005); it can be easily avoided by taking antimalarial medication and other precautionary measures. Neither Trichomonas nor malaria poses any risk of cross-infection in hospitals. A third protozoon, Toxoplasma gondii, is a parasite that lives in the intestine of cats, cysts of which are released in their faeces. These parasites can remain alive in soil and it is possible for humans to become infected by either handling cat faeces or contaminated soil. People at particular risk are women in early pregnancy when the infection can cause foetal death or brain damage.
GROWTH REQUIREMENTS OF LIVING ORGANISMS
All living organisms require nutrients: water, oxygen, light, temperature and a suitable pH to grow and thrive (Box 5.2). It is necessary to understand the growth requirements of organisms so that infection control measures can be based on scientific principles, not on rituals. For example, most bacteria that cause HCAI, such as Pseudomonas, are not demanding and will readily multiply in any warm moist environment. Others – anaerobic bacteria – require little or no oxygen and are able to flourish deep in the body. Unlike bacteria, viruses depend on living cells for their replication and therefore need an environment that will maintain them.
Box 5.2
| Water | Most organisms require water Bacteria require a moist external environment to thrive and multiply Spore-forming bacteria can live without water Some organisms die rapidly on drying (e.g. Candida, E. coli) |
| Oxygen | Aerobic bacteria require oxygen Anaerobic bacteria require no oxygen to survive, e.g. Clostridium Others require it when available, e.g. Streptococcus, Staphylococcus |
| Food | All organisms require food, e.g. organic matter – Clostridium, undigested food stuffs – E. coli Food can include inorganic matter, e.g. bed linen, work surfaces soiled with body secretions |
| Temperature | Organisms require a certain range of temperature Some can survive in extremes, e.g. some viruses are resistant to boiling water Cold temperature prevents bacterial growth |
| Light | Organisms can thrive in dark environments, e.g. in body cavities Ultraviolet light kills some types of bacteria |
| pH | Acidity determines the viability of organisms Most prefer a slightly alkaline environment with pH 5–8 Some thrive in a high pH, e.g. bacteria in alkaline urine Most organisms cannot tolerate the acid environment of the stomach |
TRANSMISSION OF INFECTION
A series of interconnecting events has to take place for an individual to acquire an infection. This is called the ‘chain of infection’ (Fig. 5.2). All microorganisms require a reservoir where they live and multiply, which may be in the environment, in a person or in an animal. To cause an infection, microorganisms need to find a way to enter the human body – a portal of entry – and in order to spread to another person they require a way to leave the body – a portal of exit (Box 5.3). Once the microorganisms have left the body in excretions and secretions, they are important sources of infection and may spread by a number of different routes.
 |
| Figure 5.2 |
Box 5.3
| Respiratory tract | Inhalation and exhalation |
| Gastrointestinal system | Ingestion and excretion |
| Skin and mucous membrane | Inoculation |
| Reproductive system | Sexually transmitted |
| Urinary tract | Sexually transmitted and excretion |
| Blood | Congenital and trauma |
These routes are categorized into airborne, direct contact and indirect contact (Table 5.1). A common example of the indirect route is the faecal–oral route of transmission by which food is indirectly contaminated by unwashed hands, and this remains a common cause of disease. Some diseases spread by a specific route while others might spread by more than one route. For example, if you sneeze the tiny droplets from the nose will become airborne, but if you then put your hand up to your nose as you sneeze the droplets will come into contact with your hand. If you did not then wash your hands you could pass it on by indirect contact to the next object you touch. For this reason it is important that all healthcare workers have an understanding of appropriate infection prevention and control measures (see Care Delivery section).
| Route of spread | Source | Example |
|---|---|---|
| Airborne | Human | Bedding, skin scales, coughing, sneezing, talking |
| Aerosols | Nebulizers, humidifiers, showers, cooling towers | |
| Dust | Sweeping, dusting, building work | |
| Direct contact | Human | Hands, uniform, sexual contact |
| Food | Hands, equipment, uncooked food | |
| Fluids | Disinfectants, antiseptics, blood, body fluids, water | |
| Insects | Flies, mosquitoes | |
| Animals | Cows, pigs | |
| Indirect contact | Inanimate objects | Bedpans, bedclothes, needles, washbowls, surgical instruments |
The sources of microorganisms causing infections or diseases can be classified as either:
• endogenous (or self-infection) which refers to microorganisms that exist harmlessly in one part of a person’s body but become pathogenic when transferred to another site
• exogenous (or cross-infection) which refers to microorganisms that do not originate from the patient but are transmitted from another source.
Think back to a patient during a placement who had either a MRSA or Clostridium difficile infection.
• Using the chain of infection (see Fig. 5.2) – consider the ways that their particular infection might have entered the body, the potential reservoir(s) and exit site(s).
• Reflect upon the specific practices that are required to be undertaken by staff to prevent the spread of infection to staff and other patients.
• Discuss your answers with a member of staff and record your findings in your portfolio.
The host
The patient or host is the final link in the chain (see Fig. 5.2) and is the most common reservoir or source of microorganisms in hospital departments, particularly their body secretions, excretions and skin lesions. A person who acquires microorganisms does not necessarily develop an infection; they may simply act as a source but be a risk to other susceptible patients. These patients are sometimes called ‘carriers’ as they carry infections around and transfer them to other patients.
The hepatitis B virus and the meningitis bacterium (Neisseria meningitidis) are two examples of microorganisms present in carriers. There are between 2% and 10% of those infected who fail to completely eliminate the virus and continue to carry it in their blood (Wilson 2006). Similarly many people are unknowingly carriers of N. meningitidis bacteria in their respiratory tract; they show no symptoms but can pass the bacteria on to other susceptible people.
Antimicrobial resistance
Prior to the introduction of antibiotics death from sepsis was common and until recently many infections could be successfully treated despite the increasing problems of resistance to antibiotics. While few microorganisms show resistance to all antibiotics, there are key pathogens which pose significant problems in healthcare settings in the UK. These include MRSA and multidrug-resistant Mycobacterium tuberculosis (Wilson 2006). A number of factors are considered to play a key role in the increasing resistance of antimicrobials, including the unnecessary and inappropriate use of antibiotics (Wilson 2006).
Staphylococcus aureus, a gram positive coccus, is an important cause of infection in both hospitals and the community, and remains the commonest cause of wound infection, after either accidental injury or surgery (Department of Health 2005b). Today, owing to this bacterium’s remarkable ability to adapt to the presence of antibiotics, approximately 90% of hospital strains and 50% of community strains are resistant to penicillin. Today MRSA occurs worldwide with strains usually resistant to two or more antibiotics (see Evolve 5.1 for more detailed information).
Resistance to drugs originally used to treat tuberculosis has occurred since streptomycin was first used in the 1940s. Treatment regimens were then devised using a second drug to destroy resistance to the first drug. Today treatment now requires a combination of three or four drugs for at least 6 months. A World Health Organization report has indicated resistance to the four first-line drugs in 35 countries (Lawrence & May 2003). In England, Wales and Northern Ireland, a report covering the years 2002–5 showed 8.7% had a resistance to one or more of the first-line drugs (isoniazid and rifampicin), and 0.9% were multidrug-resistant (Health Protection Agency 2006a). Of particular concern worldwide is HIV related drug-resistant tuberculosis, with infection more likely to become active or a latent infection more likely to reactivate. The poor absorption of drugs and interactions with other drugs makes the treatment of tuberculosis in HIV-positive patients much more complicated.
CONTROLLING THE SPREAD OF INFECTION
Both physiological and physical systems of control can be used in the prevention of infection. For such control the chain of infection (see Fig. 5.2) needs to be broken.
In the past the isolation of patients has been a recognized way to prevention. But since the 1980s and the rise in bloodborne infections a universal approach is for staff to use blood and body fluid precautions regardless of infectious status – i.e. a risk assessment approach. As there is a particular need to prevent the spread of MRSA, ‘source isolation’, with its aim to prevent the transfer of microorganisms from infected patients, has been recognized as a significant measure in the prevention of its spread (Coia et al 2006). Please access Evolve 5.2 for more information on isolation care.
Physiological controls
The body’s immune system resists the invasion of microorganisms and protects against foreign material. The first line of defence is the non-specific or passive immune response. Body systems play unique roles providing anatomical and physical barriers against the invasion of pathogens (Table 5.2).
| Route of spread | Source | Example |
|---|---|---|
| Skin | Layers of skin | Mechanical and waterproof barrier |
| Sebaceous glands | Secrete sebum – bactericidal properties Fatty acid kills bacteria | |
| Eyes | Tears | Lysozyme – digests and destroys bacteria |
| Eyelashes | Blinking reflex protects cornea from injury | |
| Mouth | Mucosa | Mechanical barrier |
| Saliva | White blood cells destroy bacteria | |
| Stomach | Gastric secretions | High acidity destroys bacteria |
| Duodenum | Bile | Alkaline pH inhibits bacterial growth |
| Small intestine | Lymphatic tissue | Destroys bacteria |
| Rapid peristalsis | Prevents bacteria from remaining in intestine | |
| Nostrils | Hairs | Trap inhaled particles and microorganisms |
| Turbinal bones | Trap inhaled particles and microorganisms | |
| Pharynx and nasopharynx | Tonsils | Lymphoid tissue traps inspired particles |
| Respiratory tree (except alveoli) | Cilia | Beat mucus and particles away from lungs |
| Mucus | Traps particles during inhalation | |
| Lung tissue | Isolates focus of infection | |
| Vagina | Secretions | Acid pH inhibits bacterial growth |
| Urethra | Male length | Prevents migration of bacteria to bladder |
| Urine | Flushing action | Washes away microorganisms |
The body’s specific or active immune response involves innate (non-specific) immunity and acquired immunity. Innate immunity is provided by genetic and cellular factors and can be influenced by age, nutritional status and any underlying disease. Active immunity results when the host develops antibodies following immunization. The active immune system is made up of two types of white blood cells:
• B lymphocytes, which produce antibodies.
• T lymphocytes, which attack cells invaded by microorganisms.
Lymphocytes have memory cells and if they encounter a particular antigen – a response that may trigger an immune response – they become active and respond by producing large numbers of specific lymphocytes and create an antibody to fight the invading microorganisms.
The body also acquires immunity artificially, through immunizations. Vaccines have been developed since the 19th century, after Edward Jenner demonstrated in 1796 that human beings could be protected from smallpox by inoculation with a similar virus that caused cowpox in cows. Vaccines are given to stimulate the production of antibodies; this induces a specific immune response, but without causing the actual disease.
The ability for people to resist and fight infection varies widely and can depend upon many factors, such as age, nutritional status and previous exposure to vaccinations and organisms. Young children with an immature immune system and the elderly with a diminished immune response are both at particular risk.
Physical stress from disease or major surgery are also recognized as important factors when assessing a patient’s individual risk of acquiring an infection. Today there are increasing numbers of patients who have or are recovering from illnesses that have caused them to become immunocompromised. They are therefore at much greater risk of acquiring infections. Patients include those with HIV/AIDS, and those who have had an organ transplant, received chemotherapy for cancer, or had multiple episodes of antibiotic treatment when very young.
Physical controls
Decontamination is the collective term used to describe the three important physical processes of cleaning, disinfection and sterilization. Inadequate decontamination has been cited as being responsible for outbreaks of infection in hospital (Wilson 2006).
The choice of decontamination method depends on the level of risk the item poses as a source of infection and the toleration of the method of decontamination (Lawrence & May 2003). The emergence of infections such as HIV, CJD and hepatitis C has seen an increased focus on decontamination procedures and policies, with particular attention paid to the potential of medical equipment to transmit such infections. An EU Directive (93/42EEC) prevents the reuse of single-use items by healthcare staff, and national standards for the provision of decontamination processes (NHS Estates 2003) ensures that all reusable medical devices are decontaminated to an acceptable standard.
CONTROL IN RELATION TO RISK
The decision as to whether an item requires cleaning, disinfection or sterilization depends upon whether it carries a low, medium or high risk of causing infection to the patient or client. The use of all disinfectants is regulated by the Control of Substances Hazardous to Health (COSHH) Regulations (Department of Health 2002) which requires employers to carry out a full risk assessment of products to be used and provide staff with appropriate information and training (Royal College of Nursing 2005).
Low risk
Cleaning – the physical removal of microorganisms and organic matter on which they thrive – is considered appropriate for equipment or practices that are considered low risk (Box 5.4). After cleaning, any article should have fewer microorganisms on it, but the dry method might simply redistribute the microorganisms into the air, while the wet method might distribute and increase the microorganisms through the use of contaminated articles such as mop heads and cloths or contaminated water. Approximately 80% of microorganisms are removed during the cleaning procedure, with drying equally important to prevent any remaining bacteria from multiplying (Wilson 2006). While cleaning alone may be an adequate method of decontamination, it is also an essential preparation for items requiring disinfection or sterilization.
Box 5.4
| Low risk | ||
|---|---|---|
| Cleaning | Dry | Mechanical action to loosen and remove large particles but may increase airborne count of bacteria up to tenfold Does not remove stains Sweeping redisperses bacteria in dust and larger particles Dry mops may be specifically treated to attract and retain dust particles Vacuum cleaning should not increase airborne counts of bacteria Expelled air from machine should not blow dust from uncleaned surfaces back into the air Dry dusting increases the air count of dust and bacteria and recontaminates cleaned surfaces |
| Wet | Water containing detergents or solvents to dissolve adherent dirt and dust Dispersal of microorganisms into the air is less likely Cleaning fluids may grow bacteria due to contamination Damp dusting is less likely to disperse bacteria into air Need to rinse after cleaning with detergent to prevent build-up of detergent film All surfaces need to be dry before use to prevent contamination from bacterial growth | |
| Medium risk | ||
| Disinfection | Heat | 80°C for 1 minute or 65°C for 10 minutes kills vegetative organisms Steam heat is most effective, e.g. autoclave Damage relates to time and temperature Disinfection at a lower temperature for a longer time is possible for heat-sensitive equipment |
| Chemical | Phenolics, e.g. Stericol, Hycolin, widely used for disinfecting inanimate objects Not active against bacterial spores or some viruses Toxic, unsuitable for living tissue until thoroughly rinsed Chemicals should not be used for food preparation or storage surfaces Hypochlorites (bleach), e.g. Milton, Sanichlor, mainly used for environmental disinfection, active against many microorganisms including viruses May corrode metals and bleach fabrics Chlorhexidine is used clinically, should not be used to disinfect inanimate objects Active against gram positive cocci (S. aureus), less active against bacilli and spores, little virucidal activity Inactivated in the presence of soap Alcohol (70% ethyl or 60% isopropyl) is rapidly active against vegetative bacteria, poor sporicidal Acts rapidly – useful surface disinfectant for physically clean surfaces, e.g. trolley tops, injection sites, hands Evaporates rapidly to leave a dry clean surface Peracetic acid (Nucidex) rapidly kills bacteria, fungi and viruses within 10 minutes. Has a strong smell and needs to be used in an area with exhaust ventilation Goggles and gloves should be worn No adverse health effects known | |
| High risk | ||
| Sterilization | Heat | Autoclaves sterilize using moist heat – steam at an increased pressure (134°C) for 3 minutes Suitable for most metal instruments, plastics, glass, fabrics Sterilizing ovens use dry heat, 160°C, for 45 minutes, 190°C for 60 minutes Heat distortion can occur, materials may become brittle or scorched |
| Gas | Ethylene oxide is very toxic and requires careful control of temperature, humidity, gas concentration and pressure Used to sterilize manufactured goods | |
| Chemicals | Used when heat or other methods are not possible or reliable sterilization is difficult Grease, proteins (blood, tissue) or air will prevent fluids coming into contact with all surfaces Prolonged immersion times are required to kill bacterial spores | |
| Irradiation | Gamma rays are used industrially, e.g. for disposable plastics after packaging Repeated irradiation causes plastics to become brittle Is expensive and uneconomical to use in hospital | |
Medium risk
Disinfection – the destruction of vegetative microorganisms to a level unlikely to cause infection – reduces the number of viable microorganisms but may not inactivate some bacterial spores (Lawrence & May 2003). It is associated with equipment that may come in close contact with mucous membranes but is not used for invasive procedures (see Box 5.4). Pathogens remaining after disinfection may pose an infection risk to particularly susceptible patients, for example those receiving cytotoxic (chemotherapy) therapy.
The two main methods of disinfection are heat and chemicals (see Box 5.4). Heat is the preferred method for disinfecting articles (e.g. surgical instruments) as it is more penetrative and easier to control than chemicals. Chemical disinfection may be required if heat is unsuitable, for example skin disinfection and heat sensitive items such as fibreoptic endoscopes. The choice is complex and requires a working knowledge of the disinfectants available and the make-up of the article that requires disinfecting (see Box 5.4).
High risk
Sterilization is the complete destruction or removal of all living microorganisms including bacterial spores (Lawrence & May 2003) and involves the use of heat, gas, chemicals or irradiation (see Box 5.4). Items requiring sterilization are described as being high risk to patients. Sterilization is recommended for all instruments and equipment used during invasive procedures (for example intravenous (IV) cannulas, surgical instruments, urinary catheters). As with disinfection, the choice of method used depends upon the item being sterilized (see Box 5.4).
OTHER METHODS OF INFECTION PREVENTION AND CONTROL
Other methods of control include hand hygiene, waste disposal and personal hygiene. These will be discussed in detail in the Care Delivery section. It is now recognized that an unclean clinical environment may contribute towards infection rates (Royal College of Nursing 2005). To assist with this important aspect of infection prevention and control, several pieces of guidance, including a resource to assist in training and setting standards (The NHS Healthcare Cleaning Manual, NHS Estates 2004), are available to promote the cleanliness of hospitals. Since the implementation of the Health Act (Department of Health 2006a), all NHS bodies have a duty to provide and maintain a clean healthcare environment.
Individual susceptibility to infection
Individual susceptibility varies enormously and can be caused when a person’s immunity is impaired. Particular groups of patients are known to be at a greater risk (Table 5.3). The Third Prevalence Survey of HCAI in acute hospitals showed that in 2006 one in seven (7.6%) of patients in UK and Ireland had an infection or were being treated for an infection that they did not have on admission to hospital (Hospital Infection Society 2006). The cost to the National Health Service has previously been approximately £1000 million per year (National Patient Safety Agency 2004). While it is acknowledged that not all HCAI are preventable, the 2005 Lowbury lecture stated that globally 10–70% are preventable (Hambraeus 2006).
Identify some of the equipment you have used for moving and handling patients, e.g. sliding sheets, hoist slings.
• How were they cleaned?
• Were they cleaned between patients?
• Do you consider these items to be low, medium or high risk in terms of transmission of infection?
• Discuss your decision with your mentor/educator in terms of current practice observed on your placement area/s.
| Group | Examples |
|---|---|
| Extremes of age | Very young and elderly |
| Critically ill | Patients in intensive care, multiple injuries |
| Chronically sick | Patients with heart and respiratory disease |
| Surgical patients | Abdominal surgery, trauma |
| Patients with underlying diseases | Patients with diabetes mellitus, malignancy |
| Immunosuppressed | Patients on steroids or chemotherapy; transplant patients |
Although hospital patients are considered to be at an increased risk due to cross-infection between staff and patients, individuals being cared for in their own homes still remain at risk, especially where they have wounds or urinary catheters in situ.
It is important to recognize not only the causal relationship and influence of physical sources and controls of infection and disease, but also the complex psychosocial issues that can be involved.
PSYCHOSOCIAL
BEHAVIOUR
Behaviour is influenced by personal beliefs and attitudes. In the past disease and infections were normally perceived as being outside an individual’s own control. For example, in the 19th century, dirty water was associated with infections and diseases such as cholera and typhoid, but it was perceived to be the responsibility of the government to prevent and control such infections (Lawrence & May 2003). Today many psychological, social and emotional factors are acknowledged as being particular influences, with the relationship between individuals and their lifestyle choices recognized as potential causes of infection and disease (Lawrence & May 2003). For example, the practice of sharing blood-contaminated needles and injecting equipment has resulted in the spread of bloodborne viruses (Department of Health 2002); and the practice of unprotected sex despite national campaigns to persuade young people of the benefits of using condoms is still resulting in a rise of newly diagnosed sexually transmitted infections (STI) in genitourinary clinics (Health Protection Agency 2007b).
However, many other groups and individuals also have a particular risk of developing life-threatening diseases and are often ignorant or unaware of them, for example people living in communal or shared accommodation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access


