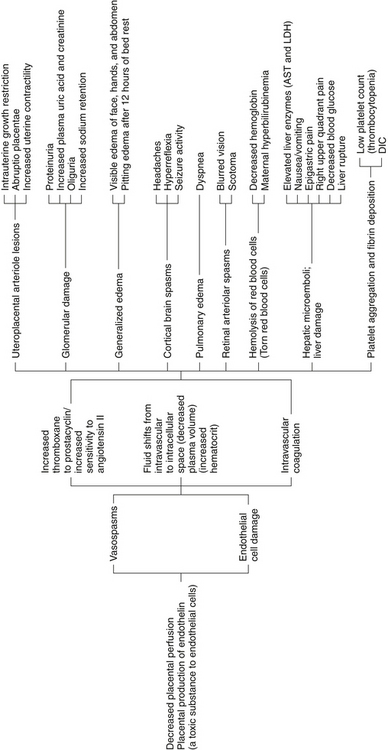
CHAPTER 19 1 Describe the characteristics of gestational hypertension, preeclampsia, eclampsia, and chronic hypertension. 2 List the risk factors for the development of preeclampsia. 3 Review the pathophysiology and physiologic alterations associated with preeclampsia and HELLP syndrome. 4 Identify assessment and physical examination techniques used in clinical practice. 5 Describe the care management of the woman with mild and severe preeclampsia. 6 Evaluate the use of anticonvulsant and antihypertensive medications. 7 Identify the priorities for management of eclamptic seizures. 8 Describe the care management of a woman with chronic hypertension. A Hypertensive disorders are the most common complication that occur during pregnancy (Sibai, 2007). 1. Hypertension complicates 5% to 10% of all pregnancies. 2. Hypertensive disorders occur in 37.8 per 1000 births (Martin et al, 2005). a. Highest rates: Native American (46.5 per 1000) and African American (41.5 per 1000) women b. Intermediate rate: Hispanic women (25.9 per 1000) c. Lowest rate: Asian or Pacific Islander women (19.6 per 1000) 3. Hypertensive disorders are a major cause of maternal and fetal or neonatal morbidity and mortality (Sibai, 2007). a. Account for 10% to 15% of maternal deaths worldwide (Askie, Duley, Henderson-Smart, & Stewart, 2007) 4. Potential maternal complications include placental abruption, intracranial hemorrhage, hepatic and renal dysfunction, disseminated intravascular coagulation (DIC), adult respiratory distress syndrome (ARDS), hypervolemia, and inhalation of gastric content (Gruji 5. Potential neonatal complications include intrauterine growth restriction, prematurity, and necrotizing enterocolitis. B Classification of hypertensive disorders of pregnancy 1. Hypertensive disorders in pregnancy are classified into five groups (Gilbert, 2007; Peters, 2008; Sibai, 2007). a. Development of hypertension without proteinuria b. Hypertension develops after 20 weeks of gestation and resolves by 12 weeks’ postpartum c. Hypertension is defined as: a. Most common hypertensive disorder of pregnancy b. Development of hypertension and proteinuria after 20 weeks of gestation c. Vasospastic, multisystem disease process d. Classified as mild or severe, depending on the severity of organ dysfunction 6. Preeclampsia superimposed on chronic hypertension C Risk factors for developing preeclampsia (Gilbert, 2007; Peters, 2008; Sibai, 2007) 1. Occurs most often with first pregnancies 2. Age extremes (younger than 19 or older than 40 years) 3. First pregnancy with a new partner 4. Preexisting medical conditions 5. Antiphospholipid antibody syndrome 6. Exposure to abundance of trophoblast tissue 7. History of severe preeclampsia 8. Family history of preeclampsia a. Increases the risk threefold b. Women with a body mass index (BMI) greater than 35 have a fourfold increased risk. D The etiology of preeclampsia is unknown (Sibai, 2007). E Normal physiologic adaptations to pregnancy (Dix, 2007; Gilbert, 2007; Peters, 2008; see also Chapter 5 for further discussion) b. Increased blood plasma volume (30% to 50%), which is greater than red cell mass expansion c. Hemodilution leads to physiologic anemia of pregnancy d. Increased cardiac output, stroke volume, heart rate, and oxygen consumption e. Decreased systemic vascular resistance; diastolic blood pressure (BP) drops 7 to 10 mm Hg by midgestation f. Decreased plasma colloid osmotic pressure; increased venous capillary hydrostatic pressure g. Fluid shifts to extracellular space in dependent limbs, resulting in edema. h. Increased clotting factors, and decreased serum albumin levels a. Increased renal plasma flow and glomerular filtration rate b. Decreased serum creatinine, increased creatinine clearance F Pathophysiology of preeclampsia has two stages (Gilbert, 2007; Peters, 2008). 1. Disruptions in placental perfusion a. The trophoblast cells of the placenta alter the spiral arteries to accommodate increased blood flow. b. The vessels seen in preeclampsia are abnormally thick walled and have higher resistance. c. Lesions develop within the vessels, along with an increase in placental infarcts. d. These abnormalities result in decreased placental perfusion. a. Hypersensitivity to vasoactive hormones b. Vasoconstriction occurs, which decreases the plasma volume and cardiac output. c. Results in hypertension and increased peripheral resistance d. Leads to hemoconcentration, increased hematocrit, and development of microthrombi e. The blood vessel walls are damaged, which leads to endothelial cell dysfunction. f. Vasospasm and poor perfusion impede blood flow to all organ systems. g. These abnormalities result in multiorgan system dysfunction (Figure 19-1) G Physiologic alterations with preeclampsia (Gilbert, 2007; Peters, 2008) a. Decreased serum albumin and plasma colloid osmotic pressure b. Endothelial cell damage leads to increased capillary permeability. c. Fluid shifts result in edema, possible rapid weight gain and risk of pulmonary edema. d. Endothelial cell damage leads to the activation of the clotting cascade and risk of DIC. e. Decreased platelet production can result in thrombocytopenia. a. Reduced kidney perfusion decreases the glomerular filtration rate. b. This damages the glomerular membrane, increasing permeability to proteins (albumin). c. Blood urea nitrogen (BUN), serum creatinine, and serum uric acid levels increase. d. Reduced uric acid and creatinine clearance can lead to acute tubular necrosis and oliguria. 4. Central nervous system (CNS) a. Fibrin deposits, hemorrhages, and cerebral edema lead to increased CNS irritability. b. Manifests as headache, hyperreflexia with clonus and seizure activity H HELLP syndrome (Gilbert, 2007; Peters, 2008; Sibai, 2007) 1. A severe complication that occurs in 5% of women with preeclampsia a. H—Hemolysis of red blood cells b. EL—Elevated Liver enzymes (aspartate transaminase [AST], alanine transaminase [ALT]) 3. Pathophysiology of HELLP syndrome a. Endothelial cell damage leads to fibrin deposits and adherence of platelets in blood vessels. b. Red blood cells are damaged passing through narrowed blood vessels and hemolyzed c. Leads to decreased red blood cell and platelet count d. Hyperbilirubinemia and hemolytic anemia may develop. e. Fibrin deposits in the liver result in impaired function and elevated liver enzymes. f. Hemorrhagic necrosis can result in a subcapsular hematoma (rare occurrence, but life threatening). 4. Signs of HELLP syndrome usually develop in the third trimester, or within 48 hours after birth. a. Most often present with influenza-like symptoms and malaise b. Epigastric or right upper quadrant pain, possibly jaundice A Predicting or preventing preeclampsia 1. No reliable test has been developed as a routine screening tool for preeclampsia (Dix, 2007; Peters, 2008). a. Several studies found that women were more likely to develop preeclampsia with low levels of placental growth factor (PIGF) in their urine, and high levels of two proteins in their blood (soluble endoglin and fms-like tyrosine kinase) (Cockey, 2005; Hellwig, 2007). b. Preeclampsia was correlated with very low levels of 25-hydroxyvitamin D in an epidemiologic study (Ravin, 2008). 2. Use of antioxidants, calcium, magnesium, zinc; restricted protein or sodium intake and fish oil supplementation have not been found to be helpful in preventing or reducing the severity of preeclampsia (Sibai, 2007). a. Low-dose aspirin therapy (60 to 75 mg a day) demonstrated a small to moderate benefit in the reduction of preeclampsia and was found to have no harmful effects (Gilbert, 2007). B Assessment (Dix, 2007; Duckitt & Harrington, 2005; Peters, 2008; Sibai, 2007) a. First pregnancy or new partner with this pregnancy c. Age extremes (younger than 19 or older than 40 years) e. Preexisting renal disease, diabetes, collagen disease, or chronic hypertension c. Drug, tobacco, and alcohol use (1) Tobacco use may decrease risk of preeclampsia, but it increases risk of low birthweight, placental abruption, and overall maternal health (2) Advised to avoid alcohol and tobacco, and limit caffeine intake. d. Activity level: exercise—amount and frequency C Physical examination (Dix, 2007; Gilbert, 2007; Peters, 2008; Sibai, 2007) a. Use correct cuff size; cuff should cover 80% of the upper arm or be 1.5 times the length of the upper arm. b. BP measurement is altered by position. (1) BP is lowest (by 10 to 20 mm Hg) in a lateral recumbent position. (2) BP is highest when supine or standing, and intermediate when sitting. (3) Sitting position is recommended for prenatal assessments. c. The arm should be supported on a desk at the level of the heart. d. BP may vary by >10 mm Hg with each arm; record the higher reading. e. Diastolic pressure should be recorded at: f. If the BP is elevated, allow the woman to rest for 5 to 10 minutes, then retake it. g. Measurements with an automated device should be checked with a manual device. a. Dependent edema (lowest or most dependent parts of the body) is common during pregnancy. b. Assessment of degree of edema (1) Minimal edema of lower extremities—1+ (2) Marked edema of lower extremities—2+ (3) Edema of lower extremities, face and hands—3+ c. Pitting edema leaves a small indentation or pit after finger pressure is applied to the area a. Average weight gain during pregnancy is 25 to 35 pounds b. Excessive weight gain is 2 pounds per day or 5 pounds per week 4. Deep tendon reflexes (DTRs; usually patellar reflex) (1) Briskly dorsiflex the foot while slightly flexing the knee. (2) Apply continuous pressure to the sole of the foot. (3) Involuntary oscillations are seen between flexion and extension.
Hypertensive Disorders in Pregnancy
INTRODUCTION
 & Milasinovi
& Milasinovi , 2006).
, 2006).
CLINICAL PRACTICE
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree