Chapter 27 HYGIENE AND COMFORT
Many factors influence whether or not a client is comfortable; they relate to physical, emotional and spiritual needs being met. To most people, physical comfort means being clean, dry, warm and free of hunger and pain. Emotional comfort relates more to being relatively free from stress and feeling satisfied with interpersonal relationships; in particular, people are more likely to be emotionally content when they feel loved and are able to love others. Spiritual comfort is connected to a sense of purpose and satisfaction in life that may or may not be entwined with religious meaning. The nurse considers all these interrelated elements when caring for clients’ comfort. This chapter deals with the physical elements of comfort, specifically in relation to hygiene care and moving and positioning clients. Management of pain is dealt with in depth in Chapter 35. Information about assisting clients with stress and spiritual comfort is provided in Chapters 11 and 13.
SKIN AND SKIN CARE
The skin is a semipermeable layer that protects underlying tissues and organs from injury or invasion by microorganisms. It is waterproof, controls the rate at which water is lost from the body by evaporation, helps regulate body temperature, and produces keratin, melanin, sweat and sebum. The skin also plays an important role in perception of sensation through the sensory nerve endings it contains, which are sensitive to touch, pressure, pain and temperature. (See Chapters 37 and 42 for more information about the skin and sensory abilities.)
INFANTS
In infancy the skin is soft and smooth and less resistant to injury or infection. It is very sensitive to heat or cold, so it is vital that the temperature of bath water is tested before bathing. Mild non-irritating soaps and lotions should be used on the skin and, as the infant has no bladder or bowel control, thorough cleansing of the genital and anal areas is necessary to prevent excoriation. After washing, the infant’s skin should be patted dry with a soft towel paying particular attention to skin creases and folds. Cradle cap, a crusting on the scalp, which may occur as a result of an accumulation of sebum, can usually be prevented by regular gentle washing and drying of the scalp and hair (Barker 2007; Pantley 2003).
OLDER ADULTS
Older age is associated with increasing changes in the dermis, with the result that skin is thinner, less elastic and dry. The decreased production of sebum and associated dryness mean that the skin of older people is less able to tolerate soap. To help counteract the dryness, a mild soap or soap-free washing lotion can be used. Oil may be added to the bath water, or a moisturising lotion applied after a bath or shower. To prevent skin irritation caused by dry skin some older people choose to change from a daily shower or bath to every second day or less frequently (Clinical Interest Box 27.1).
NURSING OBSERVATIONS OF THE SKIN
The skin should be observed for:
Care of the skin includes maintenance of cleanliness and protection from injury. The skin must be protected against injury by gentle handling and the use of appropriate bed linen and equipment. Cleansing involves the use of soaps and lotions that do not cause irritation or dryness, and careful drying of the skin, particularly in folds or creases. If the client wishes, and it is not contraindicated, deodorants, powders and perfumes may be used to enhance the feeling of freshness and to improve morale. Cleansing of the skin may be achieved by several means and the method selected depends on the client’s level of mobility and independence. Some clients will be able to have a bath or shower, while more dependent clients may require a bed or trolley bath. Whichever method of cleansing is used the nurse must ensure the client’s privacy, comfort and safety. It is now sometimes a reality that male and female clients are accommodated in the same ward or unit area and some even share bathroom and toilet facilities. This can increase the client’s discomfort and concerns about privacy, especially during hygiene and toileting procedures. The nurse will need to be sensitive to the concerns of clients faced with this situation and make every possible effort to reassure them that every effort will be made to maintain their personal privacy (Crisp & Taylor 2005; deWit 2005; Springhouse Staff 2007).
BATHING AND SHOWERING
A client may have either a bath or a shower, depending on individual preference and general condition. Both methods of cleansing refresh the client, stimulate circulation and promote relaxation. They also provide an opportunity for the nurse to observe the condition of the client’s body, including assessment of mobility and strength.
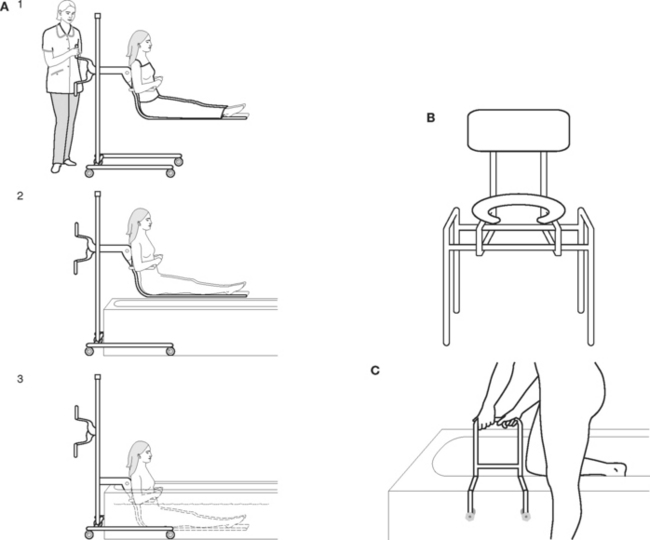
DEVICES TO ASSIST WITH BATHING OR SHOWERING
Whenever and wherever mechanical aids are used, nurses must be familiar with the operational safety aspects of each one. A full explanation about the aid being used, reassurance about its safety, and maintaining the client’s personal privacy and dignity during use are important components of reducing stress and embarrassment for the client. Examples of some aids that are available are illustrated in Figure 27.1.
CLIENTS REQUIRING SPECIAL CONSIDERATION
Clients who are weak, frail, unsteady or confused will require the nurse’s assistance to bath or shower. Key aspects of assisting a client are outlined in Table 27.1. A client may feel faint and collapse in the bath or shower. If this occurs the nurse should immediately drain the bath or turn off the shower. Towels should be used to cover the client for warmth and dignity and extra towels should be placed under the client’s legs and feet to increase venous return. The nurse should summon immediate assistance and remain with the client, ensuring that the airway is clear. (See Chapter 48 for full emergency care actions in situations in which a person has fainted.)
TABLE 27.1 GUIDELINES FOR ASSISTING A CLIENT TO BATH OR SHOWER
| Review and carry out the standard steps in Appendix 1 |
| Action | Rationale |
|---|---|
| Prepare the bathroom: | |
• Ensure there is a non-slip mat or strips in the bottom of the bath or shower recess and a bathmat on the floor • Place a chair beside the bath or shower, or in the shower if needed (unless a mechanical hoist is used) | |
| Assess the client’s mobility and strength, and gain assistance if necessary to assist client to the bathroom | Adequate assistance is necessary to promote safety and comfort |
| Offer the client use of toilet facilities before procedure | Helps to promote comfort |
| Adjust the water flow and temperature (if not automatically regulated) before client begins cleansing. Water temperature of 38–41°C is comfortable and safe for most clients. Turn on cold water first, then hot water when filling bath. Turn hot water off first | Prevents scalding. Water that is too hot may cause peripheral vasodilation and faintness |
| Help the client sit down and undress | Reduces the risk of falls |
| Observe the condition of the client’s skin | Detects any abnormalities |
| Using mechanical devices if appropriate, assist the client into the bath or shower. Offer a chair to sit on in the shower | Promotes safety, prevents falls |
| Ensure that the client is positioned away from the taps | Reduces risk of scalds |
| Encourage the client to participate as much as able, ensuring that all body areas are washed and that the skin is rinsed free of all soap | Promotes independence and adequate cleansing |
| When the client has completed washing, drain the bath or turn off the shower | Facilitates easier and safer exit from the bath or shower |
| Assist the client from the bath or shower and ensure that drying is thorough | Prevents excoriation, promotes comfort |
| While being dried the client should be seated or standing, holding supporting rails if able | Reduces fatigue, promotes safety |
| Enquire if the client wishes to use powder or deodorant. Avoid excessive amounts of powder | Powder can accumulate and ‘cake’ on the skin |
| Ensure that the client is dressed without delay | Helps to minimise fatigue and prevent chilling |
| Ensure that the client’s oral hygiene and hair-care needs are attended to. | Promotes comfort and self-esteem |
| Assist a male patient with a facial shave as required | |
| Escort the client back to their room and allow a rest period if required | Restores energy after the exertion of the bath |
| Ensure that the client is comfortably positioned with all requirements within reach | Helps to promote comfort, sense of security and safety |
| Attend to the bathroom: | |
| Ventilates the room and removes steam, prepares area for further use and minimises risk of cross-infection | |
| Report and document | Client’s condition is evaluated so that appropriate care can be planned and implemented |
A client with a plaster cast on a limb
A waterproof cover must be applied securely over the limb to protect the plaster from moisture.
BATHING THE CLIENT IN BED
A complete bed bath involves washing the entire body of a client in bed. It is performed by the nurse when a client is unable to wash unaided. Clients who may require a bed bath include those who have a debilitating illness or are paralysed or unconscious. A bed bath is also frequently needed after surgery. Depending on the client’s level of mobility, either one or two nurses perform the procedure. Health care facilities commonly adopt their own specific guidelines concerning how to perform a bed bath. An alternative to the traditional sponge bowl method is the bag bath method (Clinical Interest Box 27.2).
Key aspects related to performing a bed bath or sponge are:
Table 27.2 provides the complete guidelines for performing a bed bath.
TABLE 27.2 GUIDELINES FOR PERFORMING A BED BATH
| Review and carry out the standard steps in Appendix 1 |
| Action | Rationale |
|---|---|
| Offer the client use of toilet facilities before starting the procedure | Helps promote comfort during the procedure |
| Clear the top of the locker or over-bed table | Provides space for bath equipment |
| Shut windows and doors and/or draw the screens around the bed and close blinds | Promotes privacy and warmth |
| Adjust the bed to a suitable height | Facilitates the procedure and prevents strain on the nurse’s back |
| Assemble all the items necessary at the bedside | Nurse must remain with the client throughout the procedure |
| Ascertain whether the assistance of a second or more nurses or a mechanical lifting device is necessary | Promotes comfort and safety |
| Wash and dry hands | Prevents cross-infection |
| Remove the upper bed covers and place them on a chair. Place a towel over the client | Facilitates the procedure and promotes warmth and privacy |
| Remove the client’s upper nightclothes | Exposes the body for adequate cleansing |
| Position the client lying back on one or two pillows, unless contraindicated | Allows a relaxing position, facilitates the procedure and prevents it from causing discomfort or distress |
| Begin to wash and dry the client (using one towel to protect the bedclothes) in the following suggested order: | Logical progression that ensures that all areas of the body are washed |
| Roll the client onto one side of the bed to wash the back. Straighten or replace the bottom bed sheets | Avoids moving the client again unnecessarily |
| Roll the client onto the other side and fit the bottom sheet into position over the mattress | To complete making the bottom part of the bed |
| Dress the client in clean nightclothes | Promotes warmth and comfort |
| Replace pillows and assist the client into position | Promotes comfort |
| Attend to the client’s hair and oral hygiene and a facial shave if necessary | All hygiene needs must be attended to |
| Replace the upper bedclothes and remove the towel | Promotes comfort and warmth |
| Replace equipment (e.g. the client’s personal items in the locker, and the signal device in easy reach) | Ensures that the surroundings are tidy and that client has easy access to their belongings |
| Disinfect wash bowl and tooth mug after use, in accordance with agency protocol | Infection control |
| Remove soiled linen container | |
| Wash and dry hands | |
| Note client’s response, document the procedure and report observations | Appropriate care can be planned and implemented |
Perineal care
Care should be taken to retract the foreskin of uncircumcised adult male clients so that the head of the penis can be cleaned effectively. Once the area is cleaned the foreskin should be returned to its natural position. The scrotum should be lifted and the area below washed, rinsed and dried thoroughly. Retraction of an infant’s or child’s foreskin is not recommended. The foreskin is resistive to retraction until separation of the foreskin and glans penis occurs naturally at about age 3–5 years. After this it is recommended that the child’s foreskin be checked only very occasionally for retraction. It is recommended that the child’s mother undertake this during the routine bath at home (Leifer 2007; Pantley 2003). Therefore, under normal circumstances the nurse will not need to retract the foreskin of children during their hygiene care. However, if the tip of a child’s penis shows signs of irritation this should be reported and documented. Normally this will clear up within a few days if a protective ointment, such as oil of vitamin E or an antibiotic ointment is applied after gentle cleansing (Peron 1991).
Providing intimate care can cause embarrassment to the nurse and to the client, but this should never result in personal hygiene being neglected. A professional, dignified and sensitive manner can help with uncomfortable feelings. Chapter 12 addresses issues of embarrassment during intimate care (Crisp & Taylor 2005; deWit 2005).
BATHING AN INFANT
The procedure for bathing the infant is as follows:
The infant is then returned to the cot, which is made up with clean linen. A second nurse may be available to make the cot while the infant is being bathed, or the infant may be placed in an infant chair while the cot is made up. The infant should be placed in the cot lying on the back — the position recommended to reduce the incidence of sudden infant death syndrome (SIDS) (Barker 2007; Leifer 2007; Pantley 2003). Very young infants feel more secure if they are wrapped in a light blanket before the upper bedclothes are placed over them. The nurse should ensure that the sides of the cot are pulled up and fastened securely.
The used items are then attended to and the bath cleaned before it is used again. After washing the hands the nurse reports and documents anything of concern relating to the infant. (Areas that should be observed and assessed and abnormalities that may occur in infants are outlined in Chapter 23). As the infant grows rapidly in the first 12 months, the procedure is adapted to suit the child’s developmental level and, as the child grows, most of the actual washing is done in the bath, with the nurse supporting the infant as needed. Infants and young children must never be left unsupervised in a bath. Nurses have an important role in providing support and reassurance for new mothers, particularly when instructing them how to bath their babies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree