Introduction
In this chapter we discuss the importance of personal and oral hygiene. Keeping oneself clean and well groomed is a normal human activity that is taken for granted in the fit and healthy. As a nursing student, you are likely to meet people who are having difficulty achieving their preferred state of hygiene, especially if they have some degree of dependency, either in a hospital, in their own home or in a nursing home. Maintaining personal hygiene is such an important daily function that the Department of Health (2003) provided a definition of personal hygiene as being the:
Physical act of cleansing the body to ensure that the skin, hair and nails are maintained in an optimum condition.
and of oral hygiene as being the:
Effective removal of plaque and debris to ensure the structures and tissues of the mouth are kept in a healthy condition.
and a healthy mouth as a:
Clean, functional, and comfortable oral cavity and free from infection.
Giving a patient assistance in their personal hygiene can be an enjoyable social occasion for the patient and for the nurse. Assisting someone with their personal grooming can also provide the nurse with an opportunity to assess the patient’s physical and emotional well-being and so identify any nursing or health care needs that require attention. Helping someone in this way may appear daunting if you have never had physical contact with a stranger before. If you can develop an attitude that, through the act of washing and making a fellow human being as comfortable and refreshed as possible, you are in a position of privilege and engaged in an act of moderated love (Campbell 1984), then you can transform the experience for your patient as well as for yourself. In the process you are developing the artistic skill that is an essential part of nursing.
Maintaining personal hygiene is such an important activity in society that many religions and cultures have embodied the process in their rituals. So in this chapter we shall be considering some of these different aspects of promoting hygiene and comfort. To help you understand the importance of this process and the kinds of professional observations you should be making, we shall introduce you to the anatomy and physiology of the skin (otherwise known as the integumentary system), the appendages such as hair and nails and the different glands of the skin. Temperature regulation (or thermoregulation) of the body is an important activity of the integumentary system, along with providing the first line of defence against bacterial and parasitic infections. In Chapter 8 you were introduced to the structure and functions of the buccal cavity as part of the digestive process. In this chapter, we discuss the importance of maintaining the health of the mouth and how this can be achieved. When bathing someone or giving any form of assistance, touch is an important technique to develop and we shall explore its significance when delivering care. Throughout this chapter we will be stressing the importance of your role in ensuring that your patient is always protected from emotional, physical, social and spiritual harm, and that their comfort, privacy and dignity are promoted.
Benchmarks for personal and oral hygiene
The ‘Personal and oral hygiene’ benchmarks developed by the UK Department of Health to support their ‘Essence of care’ programme (Department of Health 2003) emphasize the importance of assessment when caring for patients so that the nurse can identify the appropriate advice and care that is needed to maintain and promote personal and oral hygiene. As you will have read in Chapter 5, it is important to maintain your patient’s dignity and self-respect by ensuring that any care is negotiated with the patient and, if relevant, their carers. Such care plans must be based on your patient’s specific and unique needs.
To help you develop a care plan for a patient that is concerned with personal and oral hygiene, you should consider the benchmarks describing best practice listed in Box 9.1.
Box 9.1
Essence of care benchmarks (Department of Health 2003)
Planned care is negotiated with patients and carers and is based on assessment of the patient’s individual needs.
Patients have access to an environment that is safe and acceptable to them.
Patients are expected to supply their own toiletries, but single-use toiletries are provided until they can supply their own.
Patients have access to the level of assistance that they require to meet individual personal and oral hygiene needs.
Patients and carers are provided with information and education to meet their individual personal and oral hygiene needs.
Patients’ care is continuously evaluated, reassessed and the care plan re-negotiated.
Anyone working in the health or social care environment, who has received the appropriate training and is considered to be safe to undertake the delegated activity, can assess patients for their oral and personal hygiene needs, but the ultimate responsibility remains with the registered practitioner responsible for that patient’s care.
When assessing your patient’s needs you should focus on their specific and individual needs, and the assessment should be conducted at the earliest opportunity, carefully recorded in their care notes and signed by the person making the assessment. It may be necessary to discuss your patient’s needs with other members of the health care team if there is a specific issue that requires particular attention. An example might be a patient who is noted to have an infestation, or a wound that appears to be infected; in such situations, the infection control nurse needs to be notified. a patient admitted with a decubitus ulcer (pressure sore) may need to be seen by the tissue viability nurse. When planning the care it is important to make use of any relevant research or other source of evidence to support the nursing practice. The care plan should be reviewed regularly to monitor its effectiveness and, if necessary, revised. It is important that an evaluation of the patient’s condition is made daily and signed by the key worker for the patient. Care plans may need to be adjusted to reflect the individual needs of patients if there are, for example, religious reasons that prescribe a particular approach.
Indicators of best practice
Infection control arrangements must ensure that the safety of both health care personnel and patients is preserved. If care is being delivered under the supervision of a registered practitioner, it is important that the student nurse is aware of any changes in the person’s condition or needs. To ensure this happens, the registered practitioner must make sure there are clear guidelines about what to observe and how to respond if necessary. The care plan should also specify the nature of care and assistance to be provided; this should be based on negotiated agreement with your patient. The aspects of essential care that should be included in the care plan are opportunities for the patient to carry out their personal hygiene particularly before and after meals, before and after using the lavatory (bedpan, commode or urinal), the nature of care they prefer and so on.
Providing health care education is an important aspect of your role as a nursing student. This may require you to check your patient’s understanding, to reinforce any health and hygiene principles using information that is based on best practice and to use language that is understandable and culturally appropriate to your patient. You may need to ensure your supervisor is aware of any situations that could cause a breach in best practice and to discuss any issues with your patient and their carers. This is particularly important if there is a risk of cross-infection (Nicol 2004). To ensure that you can recognize situations that may breach best practice guidelines you need to be knowledgeable about the biological, psychological and sociological sciences related to caring for patients’ personal hygiene needs and disposal of excreta.
Providing effective psychosocial support that is culturally sensitive is crucial when planning hygiene or elimination needs. Elimination mainly involves the urinary system and the gastrointestinal tract, but it also includes the skin and the respiratory system in the form of sweat loss and exhaled water vapour.
The significance of providing personal hygiene
The social perspective of intimacy
Healthcare providers need to go beyond sensitivity to diversity if they are effectively to assess the health of culturally diverse groups and the individuals that comprise them.
In Western society, the social meaning of nakedness is connected to intimacy, and sexual intimacy in particular. For many people, being naked is to feel deprived of protection. Clothes are used to protect the body and assist the wearer to feel that they are in keeping with what is correct socially. By removing your patient’s clothes or denying them the opportunity to wear their own clothes, the relationship between nurse and patient changes and is related to a change in the power–relationship balance. The patient is naked and the nurse is not. Avoiding the embarrassment that this imbalance may cause requires sophisticated communication skills by the nurse.
Touch in delivering care
Touch has profound emotional significance. Preceding speech as a form of communication, it takes us back to our earliest experiences… Skin is the largest sense organ of the body…
Twigg goes on to note that touch in contemporary Western life is increasingly associated with erotic relationships and, as such, adults and men in particular, live a life of limited touch except for sex. It is this that can lead to embarrassment for the nurse and the patient due to the inappropriate connection between nudity, touch and sex. Twigg also notes that men in particular regard touch in a sexualized manner and that male touch may be interpreted as homosexual. In order to deal with these often unspoken issues, the nurse must give the patient very strong, business-like cues without giving the impression that their feelings of unease are of no importance (see Case history 3.6). For example, there must be no sense, for the patient, that the nurse is in any way affected by the nature of the work or the patient’s condition. Being able to deliver care in a professional and aloof manner whilst maintaining a caring attitude takes great skill. Being able to mask any feelings towards the patient is important and finding strategies to cope with such feelings is an essential part of learning to nurse. It is not uncommon to have feelings of personal embarrassment, revulsion, curiosity or attraction, but it is essential to handle such feelings discretely and professionally. By contrast, with frequent involvement in caring for people to meet their hygiene needs, it is possible to forget any personal feelings of inhibition and at the same time to lose the insights into how your patient may be feeling with the result that they may become a work object rather than another human being and consequently dehumanized, to the detriment of good nursing practice. The key concepts for the nurse to keep in mind are communication, dignity and privacy (Twigg 2000).
The symbolic nature of hygiene
This introduction to the principles of providing intimate care when meeting your patient’s hygiene needs has explored some of the psychosocial aspects. Washing and personal hygiene have significance other than their main purpose relating to maintenance of health. Water is a very ancient, natural symbol of purification and cleansing in religious and ritual practices.
Baths have often been rites of passage into institutions and something of this sense remains in relation to their use by individuals… to mark the passage of the day or week.
There are many different religious and cultural attitudes to personal hygiene. By working closely with your patients and by reading widely about health, religion and ethnicity, you will be able to appreciate the important health issues and how to address them without causing affront to your patients in terms of their belief structure and faith. Many faiths have strict hygiene laws concerning preparation for prayer, meal times and following excretion of waste products. The following sections identify some of the different bathing preferences that you might encounter, but it is important that you find out about your patient’s preferences before making assumptions.
Muslim patients
Patients who adhere to the Muslim faith may require running water in which to wash, and so may prefer to be offered a shower. It is considered imperative for people who are Muslim to clean the genital area after going to the toilet and this requires the provision of a jug and washbasin or a bidet. The left and right hands in the Muslim faith have very specific purposes, and for some patients it is considered an insult if these purposes are ignored. A person’s left hand is used to provide hygiene, the right hand for nourishment. This can have important implications for a nurse who is left-handed and feeds a patient with their left hand, or the siting of intravenous fluids if it means the patient can not use their hand for the appropriate purpose.
The mouth, hands and feet are cleansed five times a day prior to praying. The sanctity and privacy of the female Muslim patient is considered paramount, and she may require that she is completely covered from head to toe to shield her from the gaze of male visitors, patients or male health care workers who may come into the clinical setting. You need to bear in mind that your patient may object to wearing hospital clothes and you will need to negotiate suitable alternatives.
Hindu patients
Hindu patients may require running water in which to bathe. Hindu religious laws require that the genital region must be washed after using the toilet, so patients will need to know that there is a jug and washbasin within the toilet area or will be made available if they are confined to their bed space. If you are caring for a Hindu patient, you need to make sure that this care is documented in their care plan and that it is carried out. Female Hindu patients may wish to ensure that they can keep their legs, breasts and upper arms covered at all times. They may prefer to wear their own clothing during medical procedures and may object to wearing hospital clothing. Some Hindu patients may wish to wash prior to praying.
Sikh patients
Sikh patients may prefer to shower. The adult, male Sikh patient will have long hair, a beard and be required to wear a turban on his head. The hair of the female Sikh patient is held in a ‘bun’. The hair of the Sikh patient must never be cut, as the head is the most sacred part of the body. Devout Sikhs may never completely remove their underclothes. They are required to push their underclothes down leaving them over one ankle, only removing them completely when clean underclothes are in position over the other leg. The Sikh patient may need to wash once or twice daily before praying.
Summary
The above discussion is a huge oversimplification of the religious issues involved with hygiene and religion, and we are indicating only the most frequent nursing interventions that you may need to provide. Reading widely about differing cultures and being open to learning from your patients are important if you are to provide effective nursing care.
Help with bathing involves nakedness, touch and the transgression of the normal boundaries of adult life. To receive such help thus represents one of the greatest watersheds of aging or disability… Only the very young, or people who cannot manage, are helped in these ways, and this is a powerful source of the infantilizing tendency in care work.
Twigg’s statement is of great importance, and warns nurses of the dangers of infantilizing pa-tients by robbing them of independence and thus providing poor nursing care. During any episode of delivering hygiene care, it is important to promote and preserve your patient’s independent activity as far as possible. Your goal when providing personal hygiene care is to promote your patients’ ability to care for themselves, and to assist them only until they have the necessary knowledge or strength to be independent. There is usually some small part of the care delivery process that your patient can undertake independently, unless they are too young or suffering from a chronic condition such as dementia, or if they are unconscious.
Having an understanding of the skin or the integumentary system will help you to appreciate the differences you might notice when delivering personal hygiene, and can alert you to signs and symptoms that may need attention.
Anatomy and physiology of the integumentary system
The integumentary system is considered to be the largest system of the human body. In an adult it is estimated to weigh about 4 kg (9 lb) and has a surface area of approximately 1.5–2 square metres (m2). Its thickness varies depending upon where it is located and its function, so in some areas it is only 1.5 mm thick and in others it is as much as 4 mm (Marieb 2005). The integumentary system has two well-defined regions: the epidermis and the dermis. Enclosed within these two layers are the organs of the epidermis and dermis and the skin appendages: sweat glands, sebaceous glands, hair and nails. All of these structures provide a warning system, through receptors responsible for pain, pressure and touch, and a defence system of protection so that everyday encounters do not damage the internal structures of the human body. The skin is the body’s first line of defence and is also important in the regulation of body temperature and fluid balance.
The structure of the skin
The epidermis is the outermost region of the skin and is composed of layers of epithelial cells that naturally regenerate. Beneath the epidermis is the dermis. This is made up of connective tissue and constitutes the bulk of the skin (Figure 9.1). The dermis and epidermis are firmly attached to each other through a basement membrane. To keep the dermis healthy, it has a blood supply that in some areas of the body is very rich and involves a process called diffusion from dermal blood vessels. Beneath the dermis lies the subcutaneous tissue. This is not strictly considered to be part of the skin, but it does contribute to its protective nature. It is made up of mainly adipose tissue and it anchors the skin to underlying organs. It acts as a shock absorber and provides a storage place for excess lipids and so insulates deeper body tissues.
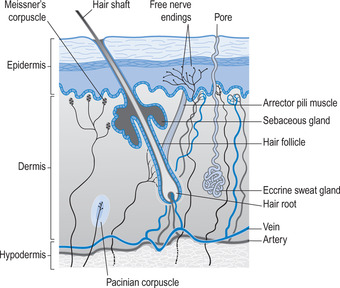 |
| Figure 9.1A cross-section through the skin. |
The epidermis
The epidermis is avascular (without blood vessels), stratified (in layers), squamous (sheds and replaces its cells) epithelium, containing keratin (a protein) and cells that have important functions. These cells are:
• Keratinocytes.
• Melanocytes.
• Langerhans cells.
• Merkel cells.
Keratinocytes
Most of the epithelial cells of the epidermis are keratinocytes. Their main role is to produce keratin, a tough protein that contributes to the protective qualities of the epidermis. As keratin is made within a cell, the cell becomes harder and flatter (Herlihy & Maebius 2003). Without keratin the skin would not be able to provide protection against water loss and provide resistance to biological, chemical and physical damage. Keratin also makes the skin waterproof. Some substances, however, can gain entry to the body via the skin, including steroids, fat-soluble vitamins (A, D, E and K), acetone, lead and mercury (Marieb 2005). This also means that some types of medication can be administered via the skin (e.g. nicotine and glyceryl trinitrate). If the skin becomes excessively dry, then it may crack and provide a route of entry for invading micro-organisms such as methicillin-resistant Staphylococcus aureus (MRSA). This would also occur if the skin were subjected to trauma (cuts and abrasions). When trauma occurs, a localized inflammatory response takes place, leading to redness, pain, swelling, increased heat and possible loss of function of the affected area. These features of inflammation arise as a result of increased blood flow (hyperaemia) to the area with an associated dilation of the underlying dermal blood vessels. There is also migration of white blood cells and macrophages to the area in order to destroy any bacteria or other foreign substances present at the site and to initiate the healing process (Marieb 2005).
Melanocytes
Skin colour is made up of a pigment known as melanin; this is produced by melanocytes, which are found distributed amongst the keratinocytes of the deeper layers of the epidermis. Once melanin has been made by the melanocytes, it is transported along slender ‘highways’ (processes) that protrude from the main body of the melanocyte. It is then exported out of these processes where it is taken up by the surrounding keratinocytes, which become stained by the melanin. Differences in skin colour appear to be attributed to the amount of melanin made by the melanocytes rather than the number of melanocytes, as all humans have approximately the same number of melanocytes (Marieb 2005). The skin is protected from the harmful effects of ultraviolet light (UV) radiation by the action of melanin. Once melanin is taken up by the keratinocytes it accumulates and forms a shield to protect the nucleus of the cell (and the deoxyribonucleic acid inside the nucleus) from the damaging effects of UV radiation from the sun.
Exposure to ultraviolet light (sunlight) increases the amount of melanin made by the melanocytes and contributes to changes in skin colour. In fair-skinned people who have had exposure to sun burn, particularly in their childhood, these melanocytes are known to change and develop tumours known as melanoma (see Case history 9.1). During exposure to strong sunlight and ultraviolet light, it is important to protect the skin by clothing and where this is not possible to wear a high-protection sun screen (see Case history 9.2); this is particularly important for babies and young children.
Case history 9.1
Caring for a patient with a mole on her back
Andrea is on placement in a gynaecology ward and is caring for a glamorous 30-year-old fashion model, Jerry, who has been admitted for minor surgery the next day. While Andrea is chatting to Jerry, she notices that she has unseasonably brown skin and discovered that Jerry uses a sunbed every week to top up her tan, because of her naturally pale complexion. Andrea is a bit concerned to hear about this as she knows that the incidence of malignant melanoma is rising in the UK, particularly in younger people. She asks Jerry if she has any itchy moles that she has noticed. Jerry shares that she does have one on her back that seems to be getting larger, and tends to bleed if she scratches it. Andrea realizes that these are the signs of skin cancer and that Jerry ought to be seen by a dermatologist or melanoma specialist as quickly as possible.
The house officer comes to see Jerry’s mole and decides that it does need to be investigated further as a matter of urgency, and makes the necessary arrangements.
Andrea is curious to know more about these kinds of skin lesions as she thought it was only older people who are at risk, so she arranges to spend an afternoon in the melanoma clinic and observe patients being seen. She also visits the website of the National Institute for Health and Clinical Excellence (www.nice.org.uk) to see if there are any guidelines on treating people with skin tumours. On the website under ‘cancer service guidance’ she finds ‘Skin tumours including melanoma. Improving outcomes for people with skin tumours including melanoma’ (NICE 2006). This document provides an overview of the incidence of skin tumours as well as guidance on best practice in their management.
Case history 9.2
Caring for a patient with a mole on his face
First-year nursing student Michael was assisting Mr Marsh (a 65-year-old retired teacher) with his daily shower following knee surgery. Mr Marsh had had a kidney transplant 10 years previously and was taking immunosuppressant therapy to prevent his kidney being rejected. Michael noticed that Mr Marsh had a pale raised skin lesion on his forehead and asked him if he had noticed it. Mr Marsh thought it was probably a basal cell carcinoma as they are common in people who are taking immunosuppressants. Mr Marsh said he normally tried to protect his skin from the sun as these carcinomas tend to pop up quite often. In fact, he had already had three removed from his face and hands. Michael had read about skin cancers and was interested to speak to Mr Marsh about his experience of them. Mr Marsh was hoping that the house officer would arrange for him to be seen by the dermatologist or the melanoma specialist so that he could have it removed with a dose of radiotherapy. Michael agreed to talk to his mentor about it and perhaps get the house officer to come and see Mr Marsh. He documented his findings and his actions in Mr Marsh’s care notes.
Langerhans cells
Langerhans cells are star-shaped and migrate to the epidermis from the bone marrow. They are a form of macrophage (a white blood cell that can ingest foreign protein such as bacteria) and are important for activation of the immune system. They too have slender processes protruding from a main body and these processes extend between the keratinocytes. Langerhans cells are responsible for the normal response of the skin to chemical or physical damage to the skin, and alert the lymphocytes of the immune system to their presence.
Merkel cells
Merkel cells are found where the epidermis and dermis meet. There are not so many of these and they are semicircular in shape. Adjoining each one is usually a sensory nerve ending. This arrangement is known as a Merkel disc and operates as a sensory receptor (touch).
The layers of the epidermis
The layers of epithelial cells found in the epidermis are divided into four or five sublayers. Most areas of the skin have four layers, but in areas where there is a great deal of friction and wear, such as the heels or soles of the feet, there are five layers (Richardson 2003). The cells that compose the epidermis are capable of regenerating, and their progeny migrate from the basal layer to the surface, or stratum corneum, as they age.
From the base of the epidermis to the topmost visible layer, the layers of the epidermis are:
• Stratum basale (germinativum).
• Stratum spinosum.
• Stratum granulosum.
• Stratum corneum.
Of these, the two most important are the stratum basale and the stratum corneum.
Stratum basale
This is the deepest layer of the epidermis and is the region in which new epithelial cells (keratinocytes) are constantly being made. A small percentage of the cells in this layer are stem cells that continually produce new keratinocytes via mitosis (cell division). Each stem cell divides approximately every 19 days and produces one daughter cell and one stem cell. The stem cells remain in the stratum basale and the daughter cells migrate towards the stratum corneum. It can take about 14 days for the daughter cells to reach the stratum corneum, and another 14 days to move through it (Haake et al 2001). Melanocytes are found here as well as some Merkel cells. As the epidermis does not have blood vessels, the cells in this layer receive their oxygen and nutrient supply via diffusion from the blood vessels in the dermis below. The further these daughter cells move from the basal layer towards the stratum corneum the fewer nutrients they receive and so they age and eventually die and are shed from the body (on a daily basis, millions of cells are lost through wear and tear).
Stratum spinosum
As the daughter cells move into this layer, they become less able to divide and are connected to each other via specialized intracellular connections called desmosomes. This layer is between five and twelve cells thick and it is here the cells become filled with keratin-rich filaments that become arranged around the nucleus.
Stratum granulosum
In this layer, which is between three and five cells thick, the keratinocytes are flattened. As well as containing the keratin-rich filaments, they also contain keratohyaline granules. These contribute to the formation of keratin in the upper layers of the epidermis. Lamellated granules are also evident within the keratinocytes here and they contain a glycolipid that has waterproofing qualities. The glycolipid is secreted into the extracellular spaces and helps to slow down water loss via the epidermis (Marieb 2005). Other changes that take place include loss of the intracellular organelles and the nucleus (Penzer 2002). By this stage in their progress to the upper layer of the dermis the keratinocytes are dead and they form an important part of the stratum lucidum.
Stratum lucidum
This layer provides protection to the more delicate tissues beneath the dermis. It is much thicker and is found in areas that are subjected to pressure or frequent wear and tear such as the soles of the feet and the palms of the hand or calluses.
Stratum corneum
This is the thickest layer of the epidermis ranging from either 15 cells thick on the upper arm, to hundreds of cells thick on the palms of the hands and soles of the feet. The cells in this layer are fully keratinized, dead cells and are continually being sloughed off as a result of friction (via washing, putting on clothes and taking them off, scratching, etc). However, as these cells are lost, they are constantly replaced by cells that have been moving up through the lower layers of the epidermis from the stratum basale. On average, an adult can shed 18 kg (40 lb) of skin cells in a lifetime (Marieb 2005).
The dermis
The dermis is connected to the epidermis through a basement membrane, covered with the basal layer. This basement membrane provides the skin with some protection from stretching and shearing forces. The dermis is made up of connective tissue, making it flexible and strong and has two distinct regions: the uppermost papillary layer and a lower reticular layer. It is richly supplied with nerve fibres, lymphatic vessels and blood vessels, and also contains oil and sweat glands, hair follicles and sensory receptors. These structures are embedded in a gel-like matrix called the ‘ground substance’.
The ground substance is a formless gel-like substance made up of proteins, interstitial fluid and proteoglycans (Marieb 2005). It fills the spaces between the fibres and cells of the dermis. The proteins act like glue, allowing the cells to adhere to other structures of the matrix, and the proteoglycans help to trap water. Nutrients and other substances are able to diffuse through this watery ground substance. Embedded within the ground substance are three different types of fibres (see Table 9.1).
| Fibre | Composition | Action |
|---|---|---|
| Collagen fibres | Protein | Provide the dermis with its tensile strength |
| Able to bind with water providing hydration to the skin | ||
| Elastic fibres | Protein called elastin | Provide the dermis with its ability to stretch and recoil |
| Are visible when the person has lost weight (such as after pregnancy) and leave marks known as stretch marks | ||
| Reticular fibres | Finer than collagen and elastic fibres | Provide support for the structures found within the dermis (e.g. blood vessels) |
The layers of the dermis
The papillary layer
This is a thin layer of connective tissue that is highly vascular with a loose arrangement of fibres. Some sensory receptors are found in this layer; for example, Meissner’s corpuscles, which are stimulated by light pressure (e.g. stroking) applied to the epidermal surface. There are also pain receptors in this region.
The reticular layer
This constitutes 80% of the dermis (Marieb 2005). The fibres in this layer are more densely packed. In the lower part of the reticular layer may be found other sensory receptors; for example, Pacinian corpuscles, which are stimulated by heavy pressure applied to the epidermal surface. It is within this layer that many of the other structures of the skin are embedded (e.g. hair roots and sweat glands).
Cells of the dermis
These include fibroblasts, macrophages and mast cells.
Fibroblasts
These are mitotic cells that are responsible for making the fibres of the dermis.
Macrophages
These are cells that actively phagocytose (engulf) foreign substances such as bacteria, dust etc. They are especially important in the process of wound healing in the skin.
Mast cells
These contain large numbers of granules of histamine. The role of mast cells is to initiate an inflammatory reaction as part of the first-line defence mechanism when foreign substances (e.g. an insect sting, chemicals from a plant or animal bite, or bacteria) have invaded the dermis. Once activated, mast cells release histamine. Histamine then initiates the local inflammatory response. Blood vessels in the immediate area around the invasion, or tissue damage, dilate and become more permeable. Fluid then leaks out of the blood vessels into the surrounding tissue causing a localized oedema. Histamine is also involved in the local anaphylactic reaction which may be seen in the skin when it comes into contact with an allergen, as indicated by dermatitis, which some people contract from contact with hand soaps or detergents.
Hair
In humans, hair does not appear to have any physiological function. Eyebrows and eyelashes do protect the eyes by preventing dust and sweat from entering them. Adults have two type of hair: vellus, which is usually fine and pale and covers the body; and terminal hair, which covers the scalp and is found in the eyebrows (Marieb 2005). At puberty, terminal hair begins to grow in the pubic and axillary regions of both males and females. Areas of the body that do not have hair include the palms of the hands, the soles of the feet, the lips and around the nipples.
You will see from the diagram of the skin in Figure 9.1 that each hair has a root surrounded by a bag-like structure called the follicle embedded in the dermis. The hair follicle is derived from the epidermis and is composed of epithelial cells that are surrounded by a dermal connective tissue layer. Extending down from the root is the hair bulb where new hair cells are made through a process known as mitosis. These newly made cells produce keratin, which is the hard kind to give the hair durability, take up melanin from the melanocytes found in this region, to gain their hair colour, and then become part of the hair shaft. Our unique hair colour is through the action of these melanocytes found in the base of the hair follicle. Our genetic profile will determine how these different coloured melanins combine to create the hair colour. With age, melanin production decreases and the hair follicles can only generate grey and white hair. In times of famine or starvation many people develop a condition caused by a protein deficiency, known as kwashiorkor. It is characterized by the hair becoming coarse and losing its pigmentation. Some endocrine disorders cause similar changes to the hair.
On average we lose about 50 hairs every day. This process takes place in much the same way as we lose epidermal cells from the skin. Sometimes people lose more hair and this can indicate ill health or vitamin deficiency such as vitamin A deficiency, stress, fever, surgery, emotional trauma (Marieb 2005, Penzer 2002). By contrast, during pregnancy, there is an increase in hair growth, followed by hair loss in the 3 months after giving birth. Some medications such as minoxidil and phenytoin, may also increase hair growth (Quinn 2000). It seems that as humans grow older their hair growth starts to slow down, often in the fourth decade of life. This phenomenon appears to be related to atrophy of the hair follicle so that, as hair is lost, it is not replaced as quickly as it is when younger, leading to thinning of the hair or, more frequently in men, baldness (alopecia), and may be genetically determined (Marieb 2005).
Hair and heat retention
Heat retention can be assisted through the smooth muscle cells collected around the base of the hair follicle. These smooth muscle cells (called the arrector pili) contract and pull the hair follicle into an upright position. If you are exposed to cold temperatures, you can see this response with the effect of ‘goose bumps’ or ‘goose flesh’, caused by the surrounding skin of each hair being raised into a dimple. This action then traps a layer of warm air against the skin surface. Its effect is thought to help to maintain body temperature. However, its value for humans is questionable, as they have very little body hair compared to fur-coated animals for which this effect is undeniably important.
Sebaceous glands
Sebaceous glands are found all over the body except in areas such as the palms of the hands and the soles of the feet (Marieb 2005). They produce an oily substance called sebum, which is secreted either into a hair follicle or directly onto the skin surface. The sebum provides lubrication for the skin and hair, keeping them soft and moist. Without sebum the skin may become dry or the hair brittle. Many adolescents are only too well aware of the action of these sebaceous glands on their face, neck and back of the body when hormonal changes take place. Acne appears to be caused by an overproduction of sebum with an associated infection of the gland (caused by the bacteria Propionibacterium acnes), leading to a localized inflammatory response (Botek & Lookingbill 2001). Whiteheads are closed, blocked seba-ceous glands and babies often have a lot of them over their face. Blackheads are simply the accumulation of oil and dust in the sebaceous gland, giving it a black appearance (Martini & Welch 2005).
Other factors that appear to affect sebaceous gland activity include fasting and age, which cause sebum secretion to decrease. Sebaceous glandular activity is high at birth, slowing down in early childhood and rising again at about 6–8 years of age. Maximum secretion occurs in the late teens and early twenties with a slow decline into old age (Botek & Lookingbill 2001) (see Case history 9.3). With sebum production low in young children and in the older adult, appropriate skin and hair care for patients in these age groups becomes extremely important.
Case history 9.3
Marianne advises a teenager about skin care
Nursing student Marianne has been on placement in the outpatients clinic; some of the placement has been in a dermatology clinic. During her last shift, Marianne had an opportunity to speak with Rehana aged 13 years, who is concerned about the recent development of blackheads (comedones) on her nose and chin. Rehana has also noticed that spots are appearing (papules and pustules) on her face and neck. Marianne explains that the changes are due to normal hormonal influences causing an increase in the production of sebum through enlargement and overproduction of the oil glands. Marianne also knows that when the oil glands are overactive and the canals become blocked, bacteria that normally live on the skin and in the oil multiply, leading to inflammation and infection.
Marianne suggests that Rehana should wash her face with a mild antibacterial soap twice a day and if her skin becomes more oily over the next few months she should wash her face more often. Marianne stresses that over-washing and the use of exfoliates tends to irritate the skin and will make acne worse; therefore, Rehana should not use any abrasive cleaners/pads.
Rehana then asks Marianne how often she should wash her hair. Marianne knows that the oilier a person’s hair is the more often they should shampoo it; also that it is best to keep the hair off the face so that the oils from the hair are not transferred to the face. Rehana is concerned about her appearance and has taken to wearing an oil-based foundation cream as it provides a more effective cover for her acne. Marianne encourages Rehana to use a light cosmetic that is water-based and suggests she checks the ingredients to ensure that the first ingredient on the label is listed as water. Greasy applications such as cold creams, Vaseline and vitamin E products should be avoided.
Sweat glands
There are approximately 2.5 million sweat glands in the human body; there are two main types: the eccrine glands and the apocrine glands (Marieb 2005).
Eccrine glands
Living in a temperate climate, our bodies each produce daily an average of 900 ml of a watery substance with a low (acidic) pH of 4–6. This acidity maintains the ecology of the surface of the skin by creating a hostile environment for the bacteria that normally occur there (Marieb 2005). This acidic sweat is produced by the eccrine glands, of which there are between 144 and 339 per cm2 of skin (Kuno 1956, cited by Hurley 2001), located all over the body. You may have noticed that your own sweat has a salty taste due to its composition of various salts (0.1–0.4% of sodium, potassium), small amounts of normal waste products from protein metabolism (urea, ammonia, uric acid), vitamin C and lactic acid. Sweat is colourless and odourless.
You will see from the diagram of the skin (Figure 9.1) that each sweat gland is a coiled tube embedded in the dermis, where the sweat is manufactured, and has a duct that extends to the skin surface where sweat is released. On contact with the skin sweat normally evaporates through a process of convection from the skin surface. This process takes with it heat from the body, making it an important component in the process of temperature regulation (we shall talk about this further on in this chapter). Deodorants containing aluminium compounds inhibit the production of sweat and act as a bacteriostatic, thereby reducing the odour that arises from the increase in bacteria that would otherwise occur.
Sweating and fluid conservation
Consider Case history 9.4 and Case history 9.5 concerning sweating and fluid conservation.
• What advice do you think Mrs Bailey should be given about drinking fluids?
• In the case of baby Abrahams, what should be your first action?
Case history 9.4
Mrs Bailey
Mrs Bailey is an 80-year-old lady who takes tablets for her heart condition. These medications include a diuretic that is intended to ensure that any fluid that she retains due to her heart condition is excreted. However, on this day, the weather is extremely hot and Mrs Bailey is sweating profusely to keep cool. Her urine output is very low, but she has no swelling of her ankles. She is reluctant to drink very much as she believes it could make her heart condition worse.
Case history 9.5
Baby Abrahams
You are giving Baby Abrahams a bath. You notice that his skin is very sweaty and that his fontanelles are quite depressed. He is listless and, although he is making repeated sucking noises, his tongue is dry. All these are signs of a baby who is severely dehydrated.
Sweat loss can also have important implications for fluid balance of the body. On a hot day, an excess of sweat can be lost, taking with it important salts such as sodium and potassium salts. Normally, as sweat travels up the duct to the skin surface, electrolytes such as sodium are reabsorbed back into the body. However, with excessive sweat loss, the sweat travels so quickly along the duct that much less of the sodium is reabsorbed. Fluid and, in some instances, salt replacement are therefore vital, especially in older patients or babies, and those who are unable to obtain their own drinks. Because a fever may also cause excessive sweating, fluid replacement therapy is fundamental to the care of these affected individuals. In some circumstances, fluid and salts may need to be given intravenously. Babies and young children are particularly vulnerable in hot weather due to dehydration and loss of vital electrolytes, leading to loss of consciousness and death if their condition is not resolved quickly.
Apocrine glands
The second type of glands that are in the skin are the apocrine glands. These are not so widely distributed over the body and are found predominantly in areas where there are hairs and lymphatic glands, such as the axillary and genital areas. Apocrine glands are larger than eccrine glands and empty their secretions via ducts directly into the hair follicles. The sweat produced by these glands is similar in composition to that produced by the eccrine glands; however, it also contains lipids and proteins, giving it a milky, odourless appearance. If a person is unable to maintain good hygiene of these areas, the bacteria normally living on the skin surface are able to multiply by feeding off the lipids and proteins from the secretions from the apocrine glands. Their subsequent decomposition results in the characteristically musky odour, also known as body odour (BO). The volume of apocrine sweat is quite small, although it increases during pain, or when an individual is frightened or upset and during sexual stimulation (Herlihy & Maebius 2003). It has no role in thermoregulation.
Nails
Nails are a modification of the epidermis and evolve from the stratum basale, which also forms the nail bed. The structure of each nail comprises a body (the transparent visible region), a free edge and a root that is embedded in the skin. Beneath the body of the nail is the nail bed which has a good blood supply, giving nails their pink hue and the necessary nutrients for regeneration. Like the dermis, the nail is constantly changing its cell structure. This may be noticed if your patient is a child or young adult with a congenital abnormality of the heart or in an adult with a chronic cardiac or respiratory disorder causing severe dyspnoea (breathlessness) such as congestive cardiac failure or emphysema. In patients with these kinds of disorders their nail shape changes, with the finger tips becoming broader and the nail curved, giving a distinctive club shape (Martini & Welch 2005).
Nail growth starts from the nail matrix in the nail bed, with nail cells filling with keratin to provide strength; then as the nail cells move away from the blood supply they die and are pushed outwards across the nail bed, extending the length of the nail body. The hard keratin that makes nails tough gives them the ability to protect the soft distal aspects of the fingers and toes. Without fingernails it is often difficult to pick up or to open objects.
Functions of the skin
You will have gathered by now that the skin has a range of functions:
• Protection.
• Thermoregulation.
• Sensory reception.
• Store and synthesizer of essential substances.
• Excretion.
Protection
By providing a continuous barrier that envelopes all the body structures, the skin provides an effective first line of defence against damage from a range of pathogenic substances. This protective function of the skin takes place in three ways: chemical, physical and biological (see Table 9.2).
| Protective function | Active agents | Process |
|---|---|---|
| Chemical | Melanocytes pH of the skin | Melanin protects the skin against ultraviolet radiation light from the sun Acidity of the secretions kill off any bacteria |
| Physical | Intact skin Keratin Glycolipids | Whilst the skin is intact no micro-organisms can penetrate the epidermis Keratin provides durability and toughness Glycolipids provide lubrication and this in turn waterproofs the skin |
| Biological | Epidermal Langerhans cells | Present foreign substances (bacteria/viruses) to cells of the immune system (lymphocytes) |
| Dermal macrophages | Macrophages in the dermis can actively ingest (phagocytose) foreign substances and present them to lymphocytes to be destroyed |
Thermoregulation
An equally important feature of the skin is its role in the maintenance of body temperature. Normal core body temperature is 37°C, but it is often within a range of 35.6–37.8°C (Marieb 2005). The maintenance of core temperature is essential for the normal functioning of cellular enzymes within the body. The temperature-control centre in the body is the hypothalamus. It is situated within the brain, just under the thalamus at the top of the brainstem (Marieb 2005).
Decreasing body temperature
The body has two kinds of thermoreceptors, which are able to monitor the core temperature of the body. These thermoreceptors are responsive to information from both peripheral thermoreceptors (in the skin) and central thermoreceptors that monitor the temperature of the blood and these provide the hypothalamus with important information about temperature changes. Once the hypothalamus receives information about an increase in body temperature, various mechanisms are activated in order to promote the loss of heat from the body. These mechanisms use the structures in the skin to activate three specific processes to maximize heat loss: radiation, convection and conduction. Enabling this to happen is the good blood supply to the dermis. The hypothalamus sends chemical messengers to the peripheral blood vessels to dilate, increasing their diameter and thus increasing the flow of blood through the capillaries. This allows more blood to enter those vessels just below the skin surface, causing heat to be lost via radiation, conduction and convection. A good example of this happening is if you take a very hot bath, or shower. You will notice that if you are fair-skinned it becomes very pink, and warm, due to the vasodilation and consequent increased blood supply. You may well feel sleepy as the brain attempts to reduce energy (and thus heat) production in order to reduce the body temperature.
If the vasodilation does not resolve the high temperature, then sweating will occur. Sympathetic nerve fibres activate the sweat glands to increase sweat production. The sweat rises to the skin surface where it then evaporates, absorbing and dissipating body heat in the process.
Providing the surrounding environment is dry, heat loss via evaporation is very effective. However, if there is high air humidity, evaporation is less effective and heat loss is impaired. Generally though, as a result of the above mechanisms, body temperature will return to its normal range.
Increasing body temperature
By contrast, if the core body temperature starts to fall, the hypothalamus responds with contrasting mechanisms to ensure that heat is generated and the core temperature is maintained as far as possible.
With constriction of the blood vessels within the dermis, the blood flowing to the skin is reduced and heat loss is restricted. Because blood flow to the skin has reduced, the skin temperature drops to that of the external environment and will feel cold to touch. If this process is insufficient to maintain the core temperature then shivering occurs. Shivering is involuntary, intermittent contraction and relaxation of skeletal muscle and creates heat within the body. If the person is conscious and mobile, they will also want to move around to generate more energy and heat.
A further strategy of the body is to increase the metabolic rate by secreting a substance called norepinephrine (also known as noradrenaline). Norepinephrine is released from sympathetic nerve fibres, increasing the metabolic rate and thus causing heat production to go up. It also causes the person to feel very energetic (or jumpy) and to move around, thus generating heat. These mechanisms are designed to ensure that body temperature is able to return to within its normal range. However, if this does not happen (e.g. when the person is paralysed, or unconscious or immobile for other reasons) and the body temperature continues to fall lower, then the person will suffer from hypothermia and, unless artificial means of slowly warming them are used, they will gradually lose consciousness and die.
The skin as a sensory organ
The skin has a very good supply of various sensory receptors that are located in the dermis to help the body to monitor external stimuli such as pressure or pain, hot or cold. To protect the body from extremes of heat and cold it has a plentiful supply of nerve cells specially designed to interpret the sensation throughout the dermis – the peripheral thermosensors.
Meissner’s corpuscles respond to light touch or caresses of the skin and are located close to the surface of the dermis (papillary layer). The Pacinian corpuscles, on the other hand, sit deep in the dermis and respond to deep pressure and impact to the skin. All these receptors are wired up to the central nervous system and so the brain receives stimuli from these cells rapidly, when the system is functioning effectively. Certain parts of the body that are more likely to be exposed to these kinds of extremes (e.g. the lips and face, fingertips and genital areas) have a higher ratio of nerve sensors and so are more sensitive than other parts (Scanlon & Sanders 1995). People who have damage to the sensory nerve pathways (e.g. those with some vitamin B deficiencies, or neurological disorders) will not feel pain and so are at risk of tissue damage. People who are confused or who have brain damage or cognitive disorders may not recognize the significance of pain and so are also at risk of tissue damage.
The skin as a store and synthesizer of essential products
The skin has the capacity to store excess substances such as calcium and iron and some forms of fatty substances. Sometimes these fatty substances are stored as part of a system of synthesizing other agents such as vitamin D. We need vitamin D to absorb some essential minerals such as calcium and phosphorus, which are derived from our food through the digestive system (small intestine). However, we can not normally take vitamin D in our diet and it has to be derived from a chemical reaction with ultraviolet light sunlight in our skin. The epidermis contains a modified form of cholesterol which when exposed to ultraviolet sunlight is converted to vitamin D. This synthesized vitamin D becomes absorbed via the capillaries in the dermis into the venous blood and is transported around the body to those cells needing vitamin D for their normal functions (see also Chapter 8).
Beneath the dermis is the adipose tissue. This is an essential store for fatty acids and glycerol that has been removed from the lacteals and the bloodstream following a fatty meal and are surplus to the immediate needs of the body (see also Chapter 8). During the subsequent period, or postabsorptive state, the body draws on this store to replenish the level of energy available for normal cellular function. If you take more than is necessary, then the store of fat deposited in the adipose tissue will get bigger (Martini & Welch 2005).
Excretion
The most important organs responsible for excretion of water and water-soluble waste products are the kidneys. However, a small amount of excretion does take place via the skin. You will remember from our description of the eccrine and apocrine sweat glands that they secrete small amounts of urea (produced as a result of protein metabolism), ammonia and uric acid, along with minerals such as sodium and water. You will remember that sweating is greatest on hot days, during intensive exercise or during a fever. In normal circumstances when sweat is excreted and travels up the sweat gland duct to the skin surface, most sodium chloride in the sweat is reabsorbed. However, on a hot day, or if an individual has a fever, there may be a dramatic increase in the amount of sweat produced. In such events, sweat often travels up the duct so quickly that there is less time for the sodium chloride to be reabsorbed and consequently more of it is lost.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


