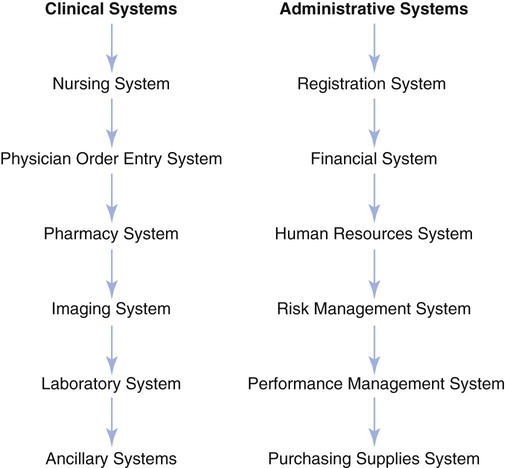
1. Define electronic health records (EHRs) and electronic medical records (EMRs). 2. Relate National Patient Safety Goals to the adoption of EMRs. 3. Analyze the driving forces behind the implementation of electronic record keeping. 4. Review the components of a hospital-wide EMR. 5. Differentiate between an EMR and a hospital information system. 6. Discuss obstacles to use of the EMR. 7. Analyze the role of the nurse in the implementation and use of the EMR. 8. Differentiate between the levels of computer competencies required of new nurses versus experienced nurses. A true electronic health record (EHR) is a complete record of an individual’s health-related data. The U.S. Department of Health and Human Services (DHHS) is spearheading an initiative to build a national electronic health care system that would allow patients and their caregivers to access their complete health records anytime and anywhere (DHHS, 2003). After this announcement, both private and public organizations joined forces to develop an EHR. Included in this effort is the DHHS, the U.S. Department of Veterans Affairs (VA), the Institute of Medicine (IOM), The Robert Wood Johnson Foundation, The Healthcare Information and Management Systems Society (HIMSS), and HL7 (Health Level 7, a health care standards developer) (HL7, 2004). A goal of this project is to have a sharing of data on a nationwide level across institutions. For example, if an individual from California entered a trauma center in New Jersey, the trauma center would be able to access the individual’s record from California. While the health care system has not reached such a level of integration, the VA has a system that allows access of the medical record across the nation for all patients of the VA system. The term electronic health record is loosely used to include any patient care record that is collected and stored in an electronic fashion. A majority of health care institutions are moving toward the creation of computerized medical records to be used within the organization. The patient record has a variety of uses. The first use is the documentation of patient care and a means of communication among members of the health care team. The second use is to provide legal and financial records, and the third is to provide data for research and continuous performance improvement (Young, 2000). In the era before computers, the management of patient records in health care organizations was based on manual file processing systems. In many hospitals, the medical records department remains a large filing system for all paper charts. Ask any nurse with experience, and he or she will tell you about requesting the “old chart” for a patient and receiving a truckload of paper documentation that may go back years. Additionally, one of the major complaints of individuals reading paper charts has always related to the illegible handwriting often seen in many areas of the chart. The IOM reports (1997, 2000, 2001) dealing with the patient safety issues facing the U.S. health care system all discussed the importance of electronic patient records in the improvement of safety, quality, and efficiency of health care in the United States. In 1991, the IOM issued a report calling for the elimination of paper-based records within 10 years. Progress, however, has been slow and the goal has not been met (IOM, 2000; Overhage et al., 2002). The financial costs for the implementation of such systems are high, and in this era of cost containment, many institutions do not have the financial resources to initiate such systems. The motivation is not to have a paperless system per se but rather to make important patient information available and useable to all appropriate caregivers. Box 11-1 lists advantages and disadvantages of the EHR. The primary and secondary uses of the hospital-wide information system are as follows (adapted from IOM, 1997): • Improve patient safety—Each year in the United States, tens of thousands of people die as a result of preventable adverse events in health care (IOM, 2000). • Support the delivery of effective care—It has been suggested that only about 55% of Americans receive recommended medical care that is consistent with evidence-based practice guidelines (McGlynn et al., 2003). • Facilitate the management of chronic illness—More than half of people with chronic conditions have three or more health providers. Physicians and patients report difficulty in the coordination of care with multiple providers (Leatherman and McCarthy, 2002; Partnership for Solutions, 2002). • Improve efficiency—Efficiency is the avoidance of waste. With the staffing and financial challenges faced by many institutions, it is imperative that processes be improved. • Feasibility of implementation—This takes into account the financial capability of an institution to support such a system, as well as the personnel capacity for support (Committee on Data Standards for Patient Safety, 2003). The core functionalities for a computerized health information system are as follows: • Health information and data—EHRs with defined datasets such as medical and nursing diagnoses, a medication list, allergies, demographics, clinical narratives, and laboratory test results can ensure access to current patient data by those who need it. • Results management—Managing all types of results (laboratory tests, radiograph results) electronically has the distinct advantage of allowing access to the results in a more efficient timeframe than with paper-based results. The automated display of results may also lead to a decrease of redundant testing (Bates and Gawande, 2003). • Order entry—Computerized provider order entry (CPOE) has been shown to decrease the number of medication errors by up to 83% (Bates and Gawande, 2003). • Decision support—Several studies have shown that computerized decision support improve drug dosing, drug selection, and screening for drug interactions (Abookire et al., 2000; Schiff and Rucker, 1998). • Electronic communication and connectivity—Improved communication between care partners, such as pharmacy, radiology, laboratory, and nursing departments, can enhance patient safety and quality of care (Schiff et al., 2003). • Patient support—A multidimensional telehealth system has demonstrated the ability to decrease the stress for some caregivers of patients with Alzheimer’s disease (Bass et al., 1998). • Administrative processes—Electronic staffing systems allow nurse managers extra time to manage care instead of creating staffing schedules. • Reporting and health management—Health care agencies have multiple reporting manually. An example of a decision support system is the Virtual Hospital. The Virtual Hospital is known as a digital library for health information. Established by the University of Iowa, this medical multimedia textbook takes full advantage of hypertext links to provide navigation between documents and figures embedded in the text. The seamlessly constructed links to off-site databases bring to the screen digitized audio and visual material. It is an impressive demonstration that allows professionals and consumers to quickly seek peer-reviewed information on a variety of adult and pediatric topics. This type of reference, accessible from anywhere in the world at any time of day, offers resources to support geographically isolated practitioners and makes teaching materials available to anyone (Virtual Hospital, 2003 [http://www.vh.org]; Kearney Nunnery, 2005). There are a wide variety of hospital information systems (Figure 11-1) with which the nurse will come in contact. The most common functions are detailed next. There are numerous nurse management information systems with which the new nurse will become familiar. One such nursing administrative system is the Automated Nurse Staffing Office System (ANSOS). Nursing management information systems provide shift reports of personnel by type needed and assigned, staffing and productivity data by unit and area, average data on the intensity of care needed, and the cost of patient care (Rousel, 2006).
Hospital Information Systems
ELECTRONIC HEALTH RECORDS
Secondary Uses
THE VIRTUAL HOSPITAL
HEALTH CARE INFORMATION MANAGEMENT SYSTEM
Administrative Systems
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Hospital Information Systems
Get Clinical Tree app for offline access