Decline in liver volume and size.
Decrease in blood flow.
Reduced drug metabolism.
Decline in capability of drug clearance.
Slower repair of damaged liver cells after injury.
Decreased production and flow of bile with decline in gallbladder contraction after meals.
Atypical clinical presentation of gallbladder and bile duct disorders.
Increased cholesterol secretion in bile leading to increased occurrence of gallstones.
Slower clearance of hepatitis B surface antigen, if infected.
Rapid progression of hepatitis C infection with lower response rate to therapy.
 GERONTOLOGIC ALERT
GERONTOLOGIC ALERT
Jaundice—any yellow color of sclerae and skin, pruritus, dark tea-colored urine, light gray or clay-colored (acholic) stool?
Any dyspepsia, anorexia, nausea, vomiting, right upper quadrant or epigastric pain, or pain radiating to the back or shoulder blade? What is the relationship of pain to eating or to position?
Has there been fatigue, malaise, loss of vigor and strength, easy bruising, or weight loss?
Any fever, chills, headache, myalgias, arthralgias, photophobia?
Any steatorrhea—stools that are loose, greasy, foamy, orange in color, foul smelling, and that float?
Have there been recent blood transfusions? Are there known blood disorders? GI bleeding?
Has there been contact with a person who has an infection such as hepatitis? Any unprotected sexual activity or ingestion of potentially contaminated food?
Has there been drug or chemical toxicity, such as carbon tetrachloride, chloroform, phosphorus, arsenicals, ethanol, halothane, isoniazid, or acetaminophen? Have amanita mushrooms been ingested recently? Are certain medications being taken, such as phenothiazine derivatives, sulfonamides, antidiabetic drugs, propylthiouracil, monoamine oxidase inhibitors, methyldopa, azathioprine, corticosteroids, thiazide diuretics, estrogens, valproic acid? Any antiviral medications taken for acquired immunodeficiency syndrome such as didanosine or antineoplastic agents, as many of these drugs can cause hepatic, biliary, and pancreatic gastrointestinal symptoms?
Is there a history of nonsterile needle puncture, as in intravenous (IV) drug use or tattoos?
Does medical history include gallstones, hepatitis, pancreatitis, Wilson’s disease, Budd-Chiari syndrome, biliary cirrhosis, liver surgery, or transplantation?
Any family history of gallstones, pancreatitis, gallbladder, or pancreatic cancer or related cancers such as breast or ovarian cancer?
How much alcohol, if any, is or has been ingested during the patient’s life and what specific type of alcohol (beer, wine, whiskey)?
Skin—yellow sclerae or skin? Rashes or scratches on body from severe scratching because of pruritus? Any signs of bruising or petechiae on body, palmar erythema, or overt bleeding?
Abdomen—any tenderness or liver enlargement in the right upper quadrant? Any ascites? Any palpable masses in the abdomen? Any fluid wave?
Peripheral vascular—any edema, anasarca, or telangiectasia?
Neurologic—what is the level of consciousness (LOC)? Any asterixis (flapping tremor elicited when the arms are extended and wrists dorsiflexed)?
 Evidence Base
Evidence Base
Tell patient a blood test will be taken and the results will be ready in 1 to 3 days.
Not a screening test for pancreatic cancer, this is an adjunct with other tests to provide support for a diagnosis of pancreatic cancer and to better measure the recurrence of pancreatic cancer after treatment.
Acute pancreatitis also causes elevated levels of the antigen.
Tell patient a blood test will be taken and the results will be ready in 1 to 3 days.
Not a screening test for primary liver cancer, this is an adjunct with other tests to provide support for a diagnosis of primary liver cancer and to better measure the recurrence of primary liver cancer after treatment.
AFP may also be elevated in certain tumors of the gonads (testes and ovaries), retroperitoneum, and mediastinum.
A noninvasive test that focuses high-frequency sound waves over an area in the abdomen to generate an image of the structure.
Ultrasound of the abdomen can detect gallstones, dilated bile ducts, fluid-filled cysts, ascites, and small abdominal masses.
This test has replaced oral cholecystography as the preferred diagnostic procedure as it is rapid and accurate and can be used in patients with liver dysfunction and jaundice.
It is reported to be able to detect gallstones with 95% accuracy.
Ultrasound with Doppler can assess the patency of the portal vein, hepatic artery, hepatic vein, and direction of blood flow. It can be used to diagnose patients with Budd-Chiari syndrome or vessel thrombosis after major liver surgery or liver transplant.
No patient preparation is required.
Explain to patient that a gel is applied to the skin over the selected area and a wandlike transducer is swept across the area of interest.
Radiographic pictures will be obtained.
A noninvasive nuclear medicine study (also referred to as a hepatobiliary iminodiacetic acid [HIDA] scan based on isotope used) using radioactive materials to evaluate gallbladder function
and aid in the diagnoses of hepatobiliary disorders, such as common bile duct obstruction, acute and chronic cholecystitis, bile leaks, bile reflux, and hepatocellular dysfunction after liver transplantation.
A radioactive agent is administered in an IV line. It is taken up by the hepatocytes and excreted rapidly through the biliary tract.
The biliary tract is scanned and images of the gallbladder and biliary tract are obtained.
Table 19-1 Liver Diagnostic Studies | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Patient should have nothing by mouth (NPO) for at least 4 hours before the procedure.
If possible, no opiates should be administered for at least 6 hours before the procedure.
Inform patient that the scan takes approximately 2 hours and additional images may need to be taken up to 24 hours later.
Endoscopic retrograde cholangiopancreatography (ERCP) involves visualization of the common bile, pancreatic, and hepatic ducts with a flexible fiber-optic endoscope inserted into the esophagus, passed through the stomach, and into the duodenum.
The common bile duct and the pancreatic duct are cannulated and contrast medium is injected into the ducts, permitting visualization and radiographic evaluation.
Done to detect extrahepatic biliary obstruction, such as calculi, tumors of the bile duct, strictures or injuries to the bile duct; intrahepatic biliary obstruction caused by stones or tumor; and pancreatic disease, such as chronic pancreatitis, pseudocyst, pancreatic duct anomalies, or tumor.
May be combined with a therapeutic biliary or pancreatic procedure, such as endoscopic sphincterotomy, placement of biliary or pancreatic stents, tissue biopsy, removal of fluid for cytology, or retrieval of retained gallstones from the common bile duct.
Assess for allergies to iodine, seafood, or contrast media to determine the need for premedication with antihistamines or steroids (per facility protocol) to prevent a reaction.
Patient must be NPO for at least 6 hours before the procedure. Withhold medications according to facility protocol.
Any patient receiving heparin should have the infusion stopped for 4 to 6 hours before the procedure. If patient is receiving warfarin, aspirin, clopidogrel, or other platelet-inhibiting or blood-thinning medication, a recent International Normalized Ratio (INR)/partial prothrombin time must be available.
Make sure that dentures are removed; instruct patient to gargle and swallow topical anesthetic to decrease gag reflex, as ordered.
Verify that patient has a signed consent form before sedation is given.
Establish baseline vital signs.
Establish IV access.
Administer antibiotic prophylaxis, as ordered.
If outpatient procedure, patient must have a responsible adult to drive him or her home as patient is not allowed to drive or operate machinery for 24 hours due to the effects of mild sedation.
Monitor and document vital signs.
Observe for and report abdominal distention and signs of perforation, GI bleeding, or possible pancreatitis, including chills, fever, pain, vomiting, hypotension, tachycardia. Notify health care provider immediately.
Maintain NPO status until gag reflex returns. Check for gag reflex by applying gentle pressure with a tongue depressor placed on the back of the tongue.
In endoscopic ultrasound (EUS), a high-frequency ultrasound probe is placed at the tip of an endoscope to assess the pancreas through the GI lumen. This helps to provide images of the pancreas and adjacent organs.
It is useful in staging pancreatic tumors; establishing the size of the tumor, its extension into adjacent structures, local and regional nodal involvement, and any blood vessels that may be involved.
Tissue may also be obtained by fine-needle aspiration through EUS guidance to confirm the diagnosis of a pancreatic malignancy.
Instruct patient that tissue may be obtained for analysis.
Verify that patient has a signed consent form for the procedure and tissue aspiration before sedation is given.
Preprocedure and postprocedure care are the same as for ERCP.
A noninvasive, nonradiation radiologic technique that produces images of the pancreatic ducts and biliary tree similar in appearance to those obtained from an ERCP with the advantage of providing images of the surrounding parenchyma.
Magnetic resonance cholangiopancreatography (MRCP) can detect the level and presence of biliary obstruction, but cannot offer therapeutic intervention.
MRCP does not require the administration of contrast material and provides ideal imaging for patients with allergies to iodine-based contrast materials. Noniodine contrast agent may be given to enhance the picture of the biliary anatomy or secretin may be given as it stimulates exocrine secretion of the pancreas and improves visualization of the pancreatic duct by increasing its caliber.
Confirm that patient does not have a pacemaker or internal defibrillator because the magnetic field could cause malfunction.
Confirm that patient does not have any metal hardware in or on the body, such as intracranial aneurysm clips, intraocular metal fragments, surgically placed inner ear devices, metal joint replacements, or steel sutures, because this will cause artifact and a distorted picture from the magnetic pull by the metal.
Remove all metal attachments from patient, such as watch, rings, IV poles, and infusion devices.
Patient must be NPO for at least 4 hours before the procedure.
Inform patient that the test takes about 10 to 30 minutes.
Positron emission tomography (PET) is an imaging technique that uses positively charged radioactive particles to detect subtle changes in the body’s metabolism and chemical activities.
Fluorodeoxyglucose 18F (18F-FDG) is injected via IV line as a radiotracer and has a short half-life of 110 minutes and is cleared rapidly from the body.
The radiotracer used most often for PET scan has a glucose component; because malignant tumors use glucose and grow at a faster rate than normal tissue, PET scans are able to locate areas of high tracer uptake, which represents tumor growth.
A PET scan provides a black-and-white or color-coded image of the function of a particular area of the body, rather than its structure. Functional change precedes structural change in tissues and organs; therefore, PET scans can detect abnormalities earlier than a computed tomography (CT) scan or magnetic resonance imaging (MRI).
Current PET scan application in hepatic, biliary, and pancreatic disease includes the detection of cancer—particularly when other conventional imaging findings are negative— and response to cancer treatment. The use of PET scanning in exploring the physiology of other diseases is under investigation.
Patient must be NPO, except for plain water, for at least 4 hours before the procedure. Patient may drink several glasses of water before the scan to ensure hydration.
Patients with diabetes or patients with glucose-intolerance may require adjustments in diet and oral hypoglycemic or insulin dosage on the day of the test as blood glucose levels
must be no higher than 150 mg/dL. Adjustments should be made on an individual basis.
Advise patient to remove jewelry or other items containing metal.
Inform patient that scanning time varies from 15 minutes to 2 hours, depending on the areas to be scanned, but the total time in the imaging center is longer (2 to 3 hours).
Caution patient that it is essential to arrive on time for this test because the FDG tracer is radioactive only for a short time. Some centers order the tracer on a per case basis, scheduling delivery of the radiotracer to coincide with patient’s time of arrival.
Inform patient that an IV line will be used to inject the radiotracer. To allow the radiotracer to disperse throughout the body, the scan will be performed 30 to 60 minutes after the injection.
Make sure that a bowel preparation has been carried out, if ordered. A urinary catheter may be inserted for a pelvic PET scan.
Inform patient that the radiotracer is rapidly cleared from the body and that the test has no adverse effects.
Patient may resume usual activities.
Patient may be encouraged to increase fluid intake to assist in flushing out the radiotracer.
Percutaneous transhepatic cholangiography (PTC) is a fluoroscopic examination of the intrahepatic and extrahepatic biliary ducts after injection of contrast medium into the biliary tree through percutaneous needle injection.
Helps to distinguish obstructive jaundice caused by liver disease from jaundice caused by biliary obstruction, such as from a tumor, injury to the common bile duct, stones within the bile ducts, or sclerosing cholangitis.
A biliary catheter may be placed during the procedure to drain the biliary tree, called percutaneous transhepatic biliary drainage (PTBD). This relieves jaundice, decreases pruritus, improves nutritional status, allows easy access into the biliary tree for further procedures, and can be used as an anatomic landmark and stent of a surgical anastomosis to allow for healing.
Assess for allergies to iodine, seafood, or contrast media to determine need to be premedicated with antihistamines or steroids (per facility protocol) to prevent reaction.
Patient must be NPO for at least 4 hours before the procedure.
Verify that patient has a signed consent form before sedatives are given.
Establish baseline hemoglobin, hematocrit, and platelet count.
Make sure prothrombin time (PT) or INR is within normal limits.
Establish baseline vital signs.
Establish an IV line.
Administer antibiotic prophylaxis, as ordered.
Monitor and document vital signs and assess puncture site for bleeding, hematoma, or bile leakage.
Check for and report signs of peritonitis from bile leaking into the abdomen: fever, chills, diffuse abdominal pain, tenderness, distention, or cholangitis (infection in the biliary tree) from bacteria in the bile being released into the GI tract and then into the bloodstream.
Continue antibiotic prophylaxis per facility protocol.
If patient has a PTBD, monitor catheter exit site for bleeding or bile drainage and monitor drainage in bile bag for color, amount, and consistency. The drainage initially may have some blood mixed with bile but should clear within a few hours. The liver makes 700 to 1,000 mL of bile in 24 hours and there should be adequate drainage when bile is draining into a bile bag (called external drainage).
Report frank blood and blood clots that appear in the bile bag.
Large amounts of bile drainage may require fluid replacement.
Maintain patency and security of biliary catheter; perform routine care and dressing at catheter exit site.
Perform routine flushing of biliary catheter per order.
Cap off end of biliary catheter to allow internal drainage of bile, if indicated. Teach patient the care and flushing of biliary catheter and signs of complications, if indicated.
Signs of complications include fever, chills, persistent jaundice, inability to flush the catheter, bleeding from the catheter, leakage around the exit site of the catheter, and dislodgment of the catheter.
Notify health care provider immediately if patient complains of abdominal bloating and exquisite abdominal tenderness as patient may be bleeding into the abdomen.
 NURSING ALERT
NURSING ALERT Evidence Base
Evidence Base
Establish baseline hemoglobin level, hematocrit, and platelet count.
Make sure INR is within normal limits.
Verify informed consent.
Establish baseline vital signs.
Inform the patient that cooperation in holding their breath for about 10 seconds during the procedure is important to obtain biopsy without damaging the diaphragm.
An IV may be inserted for sedation, as needed.
Position patient on right side with pillow supporting lower rib cage for several hours.
Check vital signs and observe biopsy site frequently for bleeding or drainage.
Report increasing pulse, decreasing blood pressure (BP), increasing pain, and apprehension, which may indicate hemorrhage.
The removal of fluid from a cyst or the removal of cells from a mass to establish a diagnosis through histologic review.
A fine needle is inserted into the suspicious area and a small sample is withdrawn.
The needle is guided by fluoroscopy, CT scan, or ultrasound and can usually reach most internal organs with minimal risk to the patient.
Establish baseline hemoglobin, hematocrit, and platelet count.
Verify informed consent.
Establish baseline vital signs.
Tell patient that a mild sedative may be given and a pain block may be performed in the area where the needle will be placed.
Encourage patient to cooperate with body position to obtain the necessary cells.
An IV may be inserted for sedation, as needed. If performed as an outpatient procedure, patient must have a responsible adult to drive him or her home as patient is not allowed to drive or operate machinery for 24 hours after procedure due to the effects of mild sedation.
Monitor vital signs per facility protocol.
Assess patient for any signs of complications, including pain, hypotension, tachycardia, and abdominal distention or hematoma at the biopsy site.
Inform patient that bruising or some discomfort may be experienced at the biopsy site.
Instruct patient on resuming anticoagulants based on health care provider directions.
Storage of vitamins A, B, D; iron; and copper.
Synthesis of plasma proteins, including albumin and globulins.
Synthesis of the clotting factors vitamin K and prothrombin.
Storage of glycogen and synthesis of glucose from other nutrients (gluconeogenesis).
Breakdown of fatty acids for energy.
Production of bile.
Detoxification and excretion of waste products.
 Evidence Base
Evidence Base
Hepatitis A (HAV) is caused by a ribonucleic acid (RNA) virus of the enterovirus family.
Mode of transmission is primarily fecal-oral, usually through the ingestion of food or liquids contaminated with the virus.
Prevalent in underdeveloped countries or in instances of overcrowding and poor sanitation.
Infected food handler can spread the disease and people can contract it by consuming water or shellfish from contaminated waters.
Commonly spread by person-to-person contact and, rarely, by blood transfusion.
Incubation period is 3 to 5 weeks, with the average being 4 weeks.
Occurrence is worldwide, usually among children and young adults.
Mortality is 0% to 1%, with recovery as the rule.
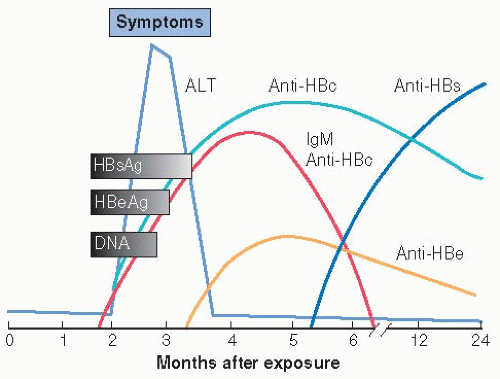
Hepatitis B (HBV) is a double-shelled particle containing deoxyribonucleic acid. This particle is composed of the following:
HBcAg—hepatitis B core antigen (antigenic material in an inner core).
HBsAg—hepatitis B surface antigen (antigenic material in an outer coat).
HBeAg—an independent protein circulating in the blood.
Each antigen elicits a specific antibody:
Anti-HBc—persists during the acute phase of illness; may indicate continuing HBV in the liver.
Anti-HBs—detected during late convalescence; usually indicates recovery and development of immunity.
Anti-HBe—usually signifies reduced infectivity.
Significance:
HBcAg—found only in liver cells, not serum.
HBsAg—usually detected transiently in blood of 80% to 90% of infected people; may be noted in blood for months or years, indicating that the patient has acute or chronic hepatitis B or is a carrier.
HBeAg—if absent, the patient is an asymptomatic carrier. If present, it indicates highly infectious period of acute, active hepatitis. If it persists, it indicates progression to chronic state.
Mode of transmission is primarily through blood (percutaneous and permucosal route).
Oral route through saliva or through breastfeeding.
Sexual activity through blood, semen, saliva, or vaginal secretions. Hepatitis B is recognized as a sexually transmitted disease.
Homosexual men are at high risk.
Incubation period is 2 to 5 months.
Occurrence is for all ages, but mostly affects young adults worldwide.
Mortality can be as high as 10%, with another 10% of patients progressing to carrier status or developing chronic hepatitis. It is the main cause of cirrhosis and hepatocellular carcinoma worldwide.
Hepatitis C (HCV) was formerly called non-A, non-B hepatitis; an RNA virus.
Mode of transmission in most cases is through blood or blood products; prior to 1992, commercial blood was not routinely tested; now, the rate of transmission through blood transfusions is less than 1%.
Found among IV drug users and renal dialysis patients.
Can be transmitted through sexual intercourse and from mother to fetus (vertical transmission).
Can theoretically be transmitted through contaminated piercing and tattooing tools and ink, but transmission by this route has not been proven.
Incubation period varies from 1 week to several months.
Occurs in all age groups.
Most common form of posttransfusion hepatitis.
May occur sporadically or in epidemic proportions.
Hepatitis D virus (HDV) is a defective RNA agent that appears to replicate only with the hepatitis B virus. It requires HBsAg to replicate.
Occurs along with HBV or may superinfect a chronic HBV carrier.
Cannot outlast a hepatitis B infection.
May be acute or chronic.
Mode of transmission and incubation are the same as for HBV.
Occurrence in the United States is primarily in IV drug abusers or multiple-transfused patients. The highest incidence exists in the Mediterranean, Middle East, and in South America.
Mortality—causes about 50% of fulminant hepatitis, which has a high mortality.
A recently identified, nonenveloped, single-strand RNA virus.
Mode of transmission is fecal-oral, but because this virus is inconsistently shed in feces, detection is difficult.
Incubation is the same as for HAV.
Occurrence is primarily in India, Africa, Asia, and Central America, but may be found in recent travelers to these areas and is more common in young adults and more severe in pregnant women.
In addition to viral hepatitis, autoimmune hepatitis (AIH) has also been identified. It is a chronic form of hepatitis that is progressive and fluctuates with degree of liver damage.
Although the cause of AIH is unknown, it is thought to be self-antigen mediated.
Treatment usually consists of anti-inflammatory or immunosuppressive agents, which may need to be taken throughout the patient’s life.
AIH may lead to chronic or fulminant liver failure and transplantation.
May have no symptoms.
Prodromal symptoms: fatigue, anorexia, malaise, headache, low-grade fever, nausea, and vomiting.
Highly contagious during this period, usually 2 weeks before the onset of jaundice.
Icteric phase: jaundice, tea-colored urine, clay-colored stool, and right upper quadrant tenderness.
Symptoms may be mild in children; adults are more likely to have severe symptoms and a prolonged course of disease.
Symptom onset usually more insidious and prolonged compared with HAV.
May be asymptomatic.
One week to 2 months of prodromal symptoms: fatigue, anorexia, transient fever, abdominal discomfort, nausea and vomiting, headache.
Extrahepatic manifestations may include myalgias, photophobia, arthritis, angioedema, urticaria, maculopapular eruptions, skin rashes, vasculitis.
Jaundice in icteric phase.
In rare cases, it may progress to fulminant hepatic failure, also called fulminant hepatitis.
May become chronic active or chronic persistent (asymptomatic) hepatitis.
Similar to those associated with HBV but usually less severe.
Symptoms usually occur 6 to 7 weeks after transfusion but may be attributed to another viral infection and not diagnosed as hepatitis.
Approximately 60% to 85% of people infected with HCV go on to develop a chronic infection. (Complications of chronic HCV include cirrhosis, decompensated liver disease, and hepatocellular carcinoma.)
In patients with HCV, the estimated risk of developing hepatocellular carcinoma after 20 years is 1% to 5%.
It is recommended that high-risk individuals be tested for HCV because many may remain asymptomatic for approximately 20 years.
Similar to HBV but more severe.
With superinfection of chronic HBV carriers, causes sudden worsening of condition and rapid progression of cirrhosis.
Elevated serum transferase levels (aspartate transaminase [AST], alanine transaminase [ALT]) for all forms of hepatitis.
Radioimmunoassays that reveal immunoglobulin (Ig)M antibodies to hepatitis virus in the acute phase of HAV.
Radioimmunoassays to include HBsAg, anti-HBc, and anti-HBsAg detected in various stages of HBV (see Figure 19-1).
Hepatitis C antibody—may not be detected for 3 to 6 months after onset of HCV illness; antibody test used for screening purposes.
Polymerase chain reaction test to confirm viral activity in HIV illness.
Antidelta antibodies of HBsAg for HDV or the detection of IgM in acute disease and IgG in chronic disease.
Hepatitis E antigen (with HCV ruled out).
Liver biopsy to detect chronic active disease, progression, and response to therapy.
Rest according to patient’s level of fatigue.
Therapeutic measures to control dyspeptic symptoms and malaise.
Hospitalization for protracted nausea and vomiting or life-threatening complications; enteral feedings may be necessary.
Small, frequent feedings of a high-calorie, low-fat diet; proteins are restricted when the liver cannot metabolize protein by-products, as demonstrated by symptoms.
Vitamin K injected subcutaneously if PT is prolonged.
IV fluid and electrolyte replacement, as indicated.
Administration of antiemetic for nausea.
After jaundice has cleared, gradual increase in physical activity. This may require many months.
First-line therapy is pegylated interferon, entecavir, or tenofovir. Treatment with nucleoside analogues is no longer considered first-line therapy due to drug resistance and viral breakthrough.
All patients should be vaccinated for hepatitis A.
Treatment of the virus with long-acting injectable interferons, such as peginterferon alfa-2a, in combination with the oral antiviral ribavirin may induce a sustained response of undetectable viral levels in about 41% to 50% of people with genotype 1 and 70% to 80% of people with genotypes 2 and 3.
Direct-acting antiviral agents recently received FDA approval for use in patients with chronic hepatitis C. These drugs include boceprevir and telaprevir and are used in addition to pegylated interferon and ribavirin to improve viral response and clearance.
Close monitoring, including complete blood count, liver function tests, and HCV viral load during the long treatment period is imperative.
Patients should be vaccinated against hepatitis A and B if they do not have immunity.
 Evidence Base
Evidence Base
Assess for systemic and liver-related symptoms.
Obtain history, such as IV drug use, sexual activity, travel, and ingestion of possible contaminated food or water to assess for any mode of transmission of the virus.
Assess size and texture of liver to detect enlargement or characteristics of cirrhosis.
Obtain vital signs, including temperature.
Imbalanced Nutrition: Less Than Body Requirements related to effects of liver dysfunction
Deficient Fluid Volume related to nausea and vomiting.
Activity Intolerance related to anorexia and liver dysfunction.
Deficient Knowledge related to transmission.
Risk for Bleeding related to coagulopathy because of impaired liver function.
Acute confusion related to encephalopathy because of impaired liver function.
Encourage frequent small feedings of high-calorie, low-fat diet. Avoid large quantities of protein during acute phase of illness.
Encourage eating meals in a sitting position to decrease pressure on the liver.
Encourage taking pleasing meals in an environment with minimal noxious stimuli (odors, noise, interruptions).
Administer or teach self-administration of anti-emetics, as prescribed.
 DRUG ALERT
DRUG ALERT
Provide frequent oral fluids, as tolerated.
Administer IV fluids for patients with inability to maintain oral fluids.
Monitor intake and output.
Promote periods of rest during symptom-producing phase, according to level of fatigue.
Promote comfort by administering or teaching self-administration of analgesics as prescribed.
Provide emotional support and diversional activities when recovery and convalescence are prolonged.
Encourage gradual resumption of activities and mild exercise during convalescent period.
Educate patient about disease and about disease transmission.
Emphasize the self-limiting nature of most forms of hepatitis and the need for follow-up of liver function tests.
Stress importance of proper public and home sanitation and of proper preparation and dispensation of foods.
Encourage specific protection for close contacts.
Immune globulin as soon as possible to household contacts of HAV patients.
Hepatitis B immune globulin as soon as possible to blood or body fluid contacts of HBV patients, followed by HBV vaccine series.
Explain precautions to patient and family about transmission and prevention of transmission to others.
Good handwashing and hygiene after using bathroom.
Avoidance of sexual activity (especially for HBV) until free of HBsAg.
Avoidance of sharing needles, eating utensils, and toothbrushes to prevent blood or body fluid contact (especially for HBV and HCV).
Report all cases of hepatitis to public health officials.
Monitor and teach patient to monitor and report signs of bleeding.
Monitor PT and administer vitamin K, as ordered.
Avoid trauma that may cause bruising, limit invasive procedures, if possible, and maintain adequate pressure on needlestick sites.
Monitor for signs of encephalopathy—lethargy and somnolence with mild confusion and personality changes, such as excessive sexual or aggressive activity and loss of usual inhibitions. Lethargy may alternate with excitability, euphoria, or unruly behavior.
Monitor for worsening of condition, from stupor to coma; assess for asterixis, the irregular flapping of the forcibly dorsiflexed outstretched hands.
Maintain calm, quiet environment and reorient patient, as needed.
Identify persons at high risk for each type of hepatitis (see pages 713-714) and advise prevention and screening. The CDC now recommends that all persons born 1945-1965 be tested for hepatitis C.
Educate adolescents about the risk of piercing and tattooing in transmission of HCV.
Encourage vaccination for HBV with series of three shots (initial shot at birth, 1, and 6 months) for high-risk patients, such as health care workers or institutionalized persons, as well as vaccination of all children from birth or at adolescence.
Instruct all patients who have received a blood transfusion to refrain from donating blood for 6 months (the incubation period of HBV). After hepatitis infection, blood should never be given if patient is an HBV carrier or was infected with HCV.
Stress the need to follow precautions with blood and secretions until the patient is deemed free of HBsAg.
Explain to HBV carriers that their blood and secretions will remain infectious.
For additional information, refer to the local public health department or the Centers for Disease Control and Prevention (www.cdc.gov).
 Evidence Base
Evidence Base Evidence Base
Evidence Base
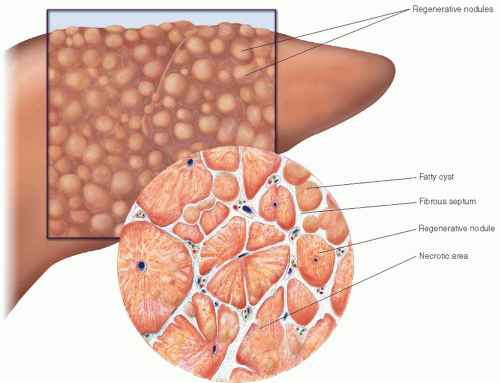
Laënnec’s cirrhosis (macronodular), also known as alcoholic cirrhosis.
Fibrosis—mainly around central veins and portal areas.
Usually due to chronic alcohol toxicity and malnutrition.
Postnecrotic cirrhosis (micronodular).
Broad bands of scar tissue.
Because of previous acute viral hepatitis or drug-induced massive hepatic necrosis.
Biliary cirrhosis.
Scarring around bile ducts and lobes of the liver.
Results from chronic biliary injury and obstruction of the intrahepatic or extrahepatic biliary system.
Partial or total obstruction of the bile ducts can lead to infectious cholangitis and cirrhosis, which is much rarer than Laënnec’s and postnecrotic cirrhosis.
Onset is insidious; may take years to develop.
Early complaints include fatigue, anorexia, ankle edema in the evening, epistaxis and bleeding gums, and weight loss.
Later complaints because of chronic failure of the liver and obstruction of portal circulation.
Chronic dyspepsia, constipation, or diarrhea.
Esophageal varices, dilated cutaneous veins around the umbilicus (caput medusa), internal hemorrhoids, ascites, splenomegaly, and pancytopenia.
Plasma albumin is reduced, leading to edema and contributing to ascites.
Anemia and poor nutrition lead to fatigue and weakness, wasting, and depression.
Deterioration of mental function from lethargy to delirium to coma and eventual death.
Estrogen-androgen imbalance causes spider angiomata and palmar erythema; menstrual irregularities in females; testicular and prostatic atrophy, gynecomastia, loss of libido, and impotence in males.
Bleeding tendencies, such as nosebleeds, easy bruising, hematemesis, or profuse hemorrhage from stomach and esophageal varices.
Liver biopsy detects destruction and fibrosis of hepatic tissue.
CT scan is helpful to determine the size of the liver, its irregularities, and in detection of a mass.
Esophagoscopy to determine esophageal varices.
Paracentesis to examine ascitic fluid for cell, protein, and bacterial counts.
PTC differentiates extrahepatic from intrahepatic obstructive jaundice.
Laparoscopy and liver biopsy permit direct visualization of the liver.
Serum liver function test results are elevated.
Minimize further deterioration of liver function through the withdrawal of toxic substances, alcohol, and drugs.
Correction of nutritional deficiencies with vitamins and nutritional supplements and a high-calorie and moderate- to high-protein diet.
Treatment of ascites and fluid and electrolyte imbalances.
Restrict sodium and water intake, depending on amount of fluid retention.
Bed rest to aid in diuresis.
Diuretic therapy, frequently with spironolactone, a potassium-sparing diuretic that inhibits the action of aldosterone on the kidneys. Furosemide, a loop diuretic, may also be used in conjunction with spironolactone to help balance potassium depletion.
Abdominal paracentesis to remove fluid and relieve symptoms (see Procedure Guidelines 19-1); ascitic fluid may be ultrafiltrated and reinfused through a central venous access device.
Administration of albumin to maintain osmotic pressure.
Transjugular intrahepatic portosystemic shunt (TIPS), an interventional radiologic procedure, may be performed in patients whose ascites is resistant to other forms of treatment. TIPS is a percutaneously created connection within the liver between the portal and systemic circulations. A shunt is placed to reduce the portal pressure in patients with complications related to portal hypertension.
Complications include bacterial infections, shunt obstruction, encephalopathy, and increase in coagulopathies.
Symptomatic relief measures, such as pain medication and anti-emetics.
Treatment of other problems associated with liver failure. Administer lactulose, rifaximin, or neomycin for hepatic encephalopathy.
Liver transplantation may be necessary.
Hyponatremia and water retention.
Bleeding esophageal varices.
Coagulopathies.
Spontaneous bacterial peritonitis.
Hepatic encephalopathy, which may be precipitated by the use of sedatives, high-protein diet, sepsis, or electrolyte imbalance.
Obtain history of precipitating factors, such as alcohol abuse, hepatitis, or biliary disease. Establish present pattern of alcohol intake.
Assess mental status through interview and interaction with patient.
Perform abdominal examination, assessing for ascites (see Figure 19-3, page 719).
Observe for bleeding.
Assess daily weight and abdominal girth measurements.