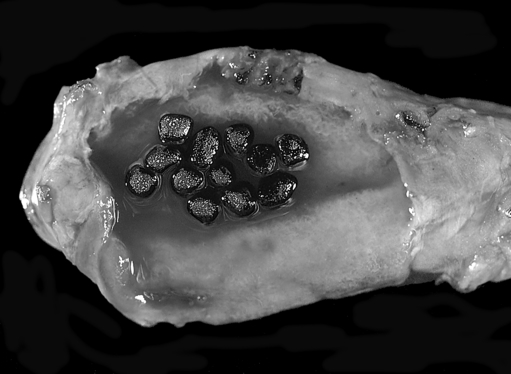
Chapter 17 Signs: Tachycardia, pallor (especially of the sclera and mucous membranes), systolic ejection murmurs (from high flow), and signs of the underlying cause (e.g., jaundice, pigment gallstones (Fig. 17-1; Plate 29) in hemolytic anemia, positive stool guaiac with a gastrointestinal [GI] bleed). Peripheral blood smear. There are many “classic” findings that can help make the diagnoses:
Hematology
2 What are the symptoms and signs of anemia?
6 What test should be ordered next?
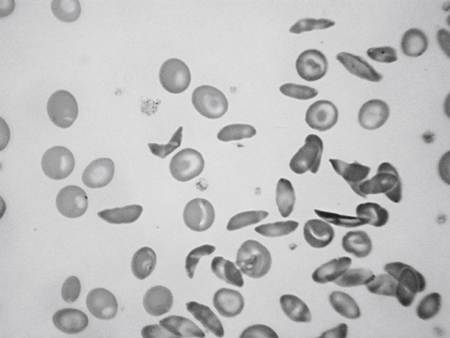
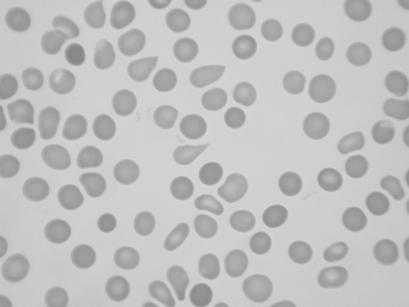
 Sickled cells (sickle cell disease; Fig. 17-2; Plate 30).
Sickled cells (sickle cell disease; Fig. 17-2; Plate 30).
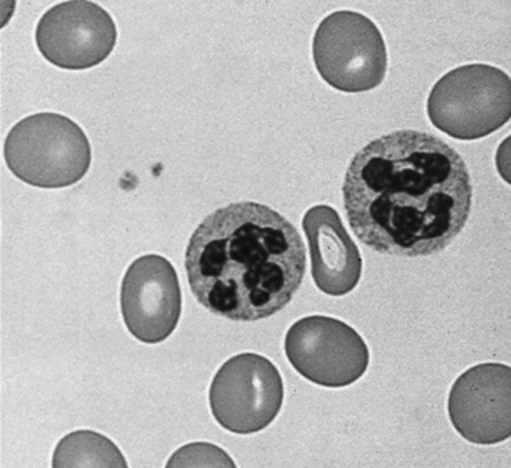
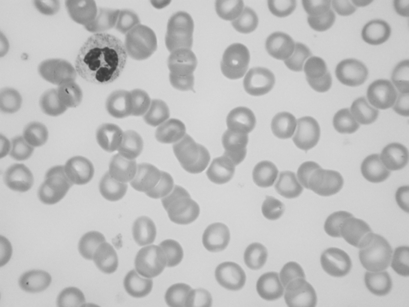
 Hypersegmented neutrophils (folate/B12 deficiency; Fig. 17-3; Plate 31).
Hypersegmented neutrophils (folate/B12 deficiency; Fig. 17-3; Plate 31).
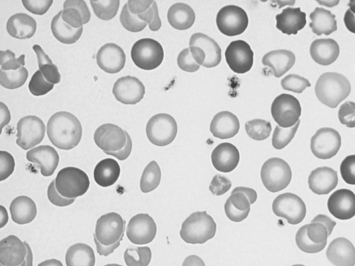
 Hypochromic and microcytic RBCs (iron deficiency; Fig. 17-4; Plate 32).
Hypochromic and microcytic RBCs (iron deficiency; Fig. 17-4; Plate 32).
 Basophilic stippling (lead poisoning; Fig. 17-5; Plate 33).
Basophilic stippling (lead poisoning; Fig. 17-5; Plate 33).
 Heinz bodies (glucose-6-phosphatase deficiency; Fig. 17-6; Plate 34).
Heinz bodies (glucose-6-phosphatase deficiency; Fig. 17-6; Plate 34).
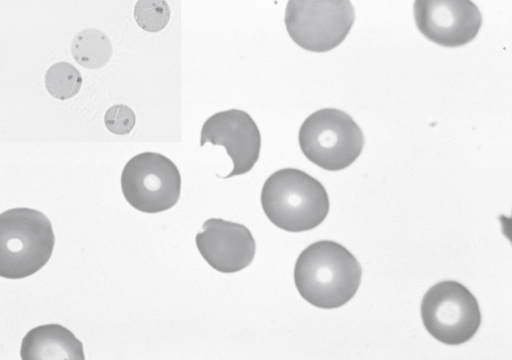
 “Bite cells” (classically, glucose-6-phosphatase deficiency; other hemolytic anemias; Fig. 17-6; Plate 34).
“Bite cells” (classically, glucose-6-phosphatase deficiency; other hemolytic anemias; Fig. 17-6; Plate 34).
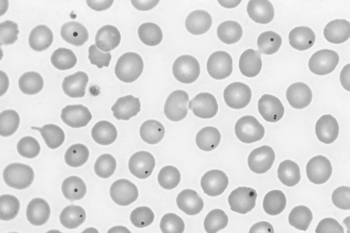
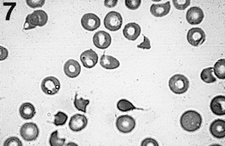
 Howell-Jolly bodies (asplenia; Fig. 17-7; Plate 35).
Howell-Jolly bodies (asplenia; Fig. 17-7; Plate 35).
 Teardrop-shaped RBCs (myelofibrosis; Fig. 17-8; Plate 36).
Teardrop-shaped RBCs (myelofibrosis; Fig. 17-8; Plate 36).
 Schistocytes, helmet cells, and fragmented RBCs (intravascular hemolysis; Fig. 17-9; Plate 37).
Schistocytes, helmet cells, and fragmented RBCs (intravascular hemolysis; Fig. 17-9; Plate 37).
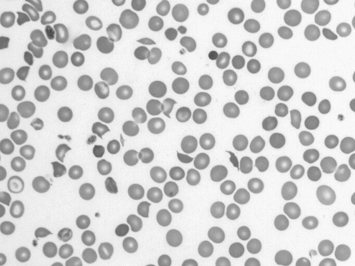
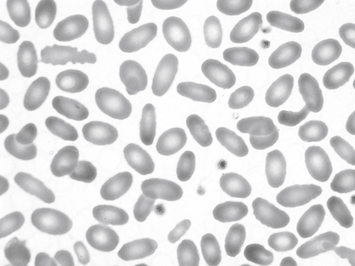
 Spherocytes and elliptocytes (hereditary spherocytosis and elliptocytosis; Fig. 17-10; Plate 38).
Spherocytes and elliptocytes (hereditary spherocytosis and elliptocytosis; Fig. 17-10; Plate 38).
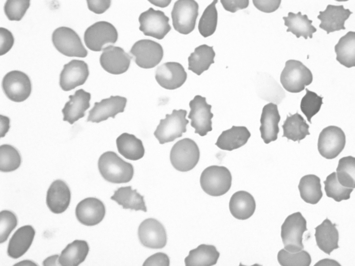
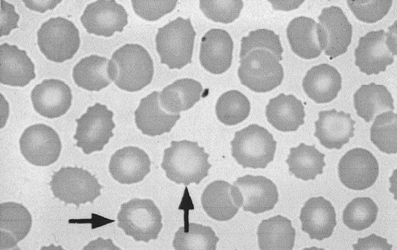
 Acanthocytes and spur cells (abetalipoproteinemia; Fig. 17-11; Plate 39).
Acanthocytes and spur cells (abetalipoproteinemia; Fig. 17-11; Plate 39).
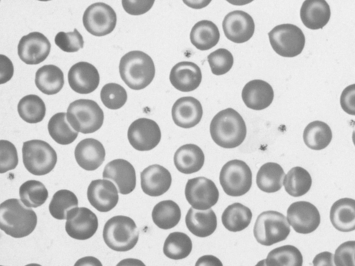
 Target cells (thalassemia, liver disease; Fig. 17-12; Plate 40).
Target cells (thalassemia, liver disease; Fig. 17-12; Plate 40).
 Echinocytes, including “burr” cells and acanthocytes (uremia; Fig. 17-13; Plate 41).
Echinocytes, including “burr” cells and acanthocytes (uremia; Fig. 17-13; Plate 41).
 Polychromasia (from reticulocytosis; should alert you to the possibility of hemolysis; Fig. 17-14; Plate 42).
Polychromasia (from reticulocytosis; should alert you to the possibility of hemolysis; Fig. 17-14; Plate 42).
 Rouleaux formation (multiple myeloma; Fig. 17-15; Plate 43).
Rouleaux formation (multiple myeloma; Fig. 17-15; Plate 43).
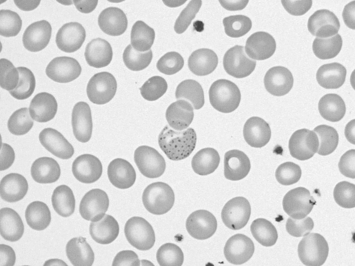
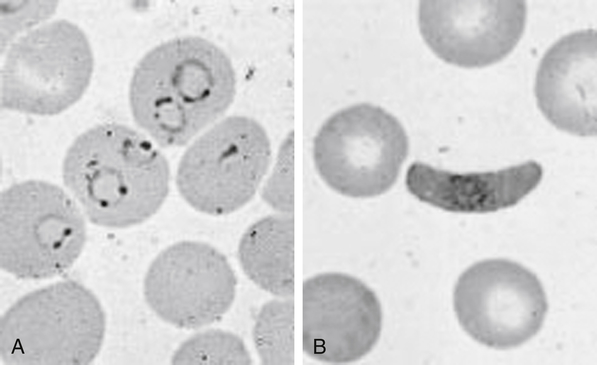
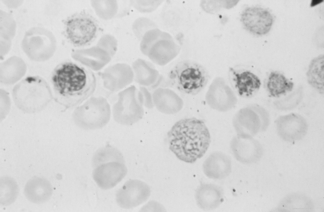
 Parasites inside red blood cells (RBCs) (malaria [Fig. 17-16; Plate 44], babesiosis).
Parasites inside red blood cells (RBCs) (malaria [Fig. 17-16; Plate 44], babesiosis).
 Iron inclusions in RBCs of the bone marrow (sideroblastic anemia; Fig. 17-17; Plate 45).
Iron inclusions in RBCs of the bone marrow (sideroblastic anemia; Fig. 17-17; Plate 45).
9 What are the classic causes of microcytic, normocytic, and macrocytic anemia? Which of these tends to have an inappropriately low reticulocyte count?
MICROCYTIC
NORMOCYTIC
With normal or elevated reticulocyte count
With normal or elevated reticulocyte count
Thalassemia/hemoglobinopathy (e.g., sickle cell disease)
Acute blood loss
Hemolytic (multiple causes)
Medications (antibody-causing)
With low reticulocyte count
With low reticulocyte count
Lead poisoning
Sideroblastic anemia
Anemia of chronic disease (some cases)
Iron deficiency
Cancer/dysplasia (e.g., myelophthisic anemia, acute leukemia)
Anemia of chronic disease (some cases)
Aplastic anemia/medications causing bone marrow suppression
Endocrine failure (thyroid, pituitary)
Renal failure
MACROCYTIC
All types have low reticulocyte count
Folate deficiency
Vitamin B12 deficiency
Medications (methotrexate, phenytoin)
Alcohol abuse (interferes with folate use)
Cirrhosis, liver disease
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access
