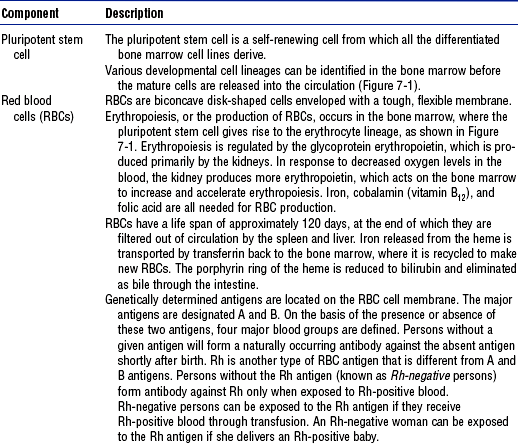
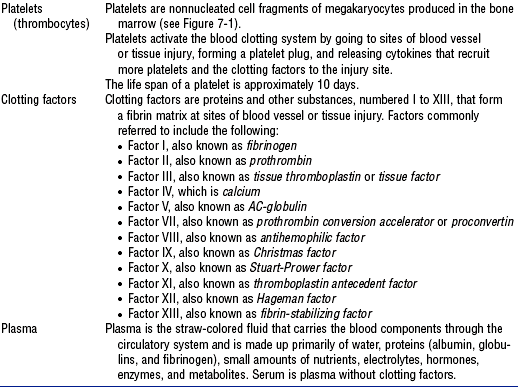
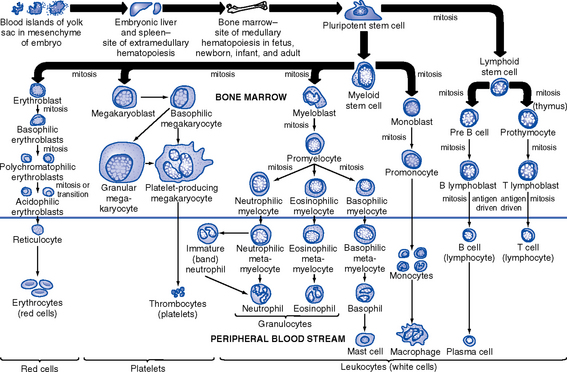
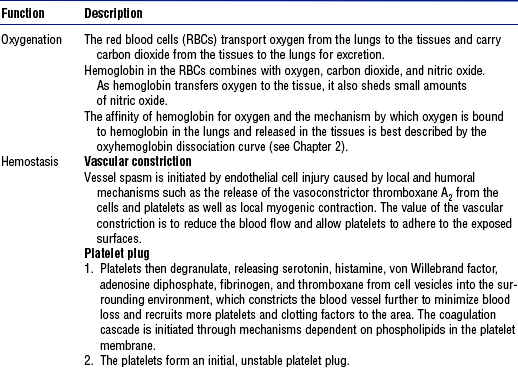
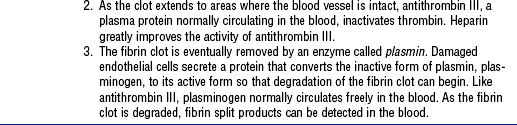
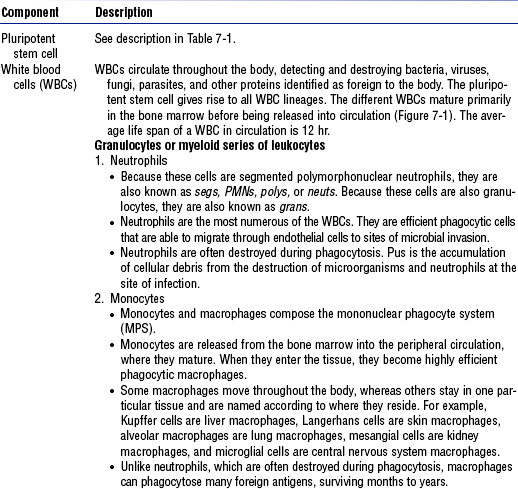
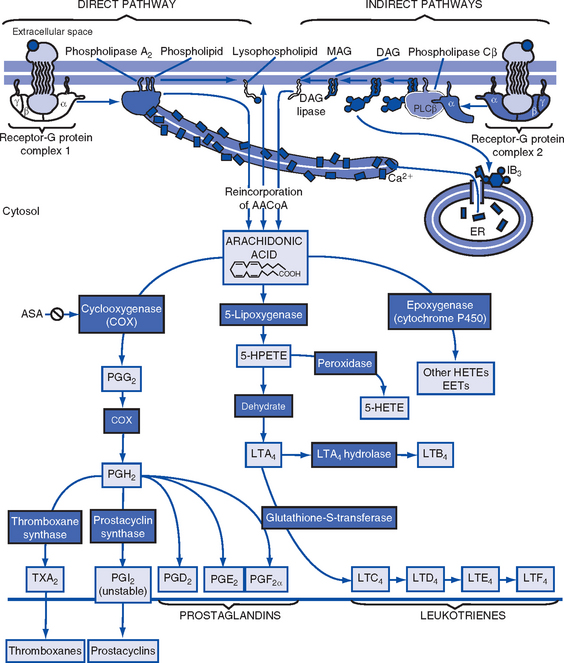
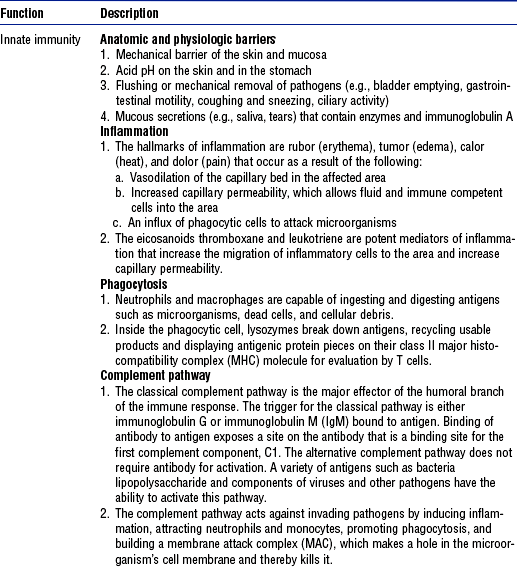
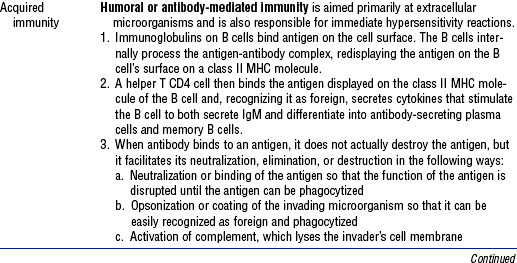
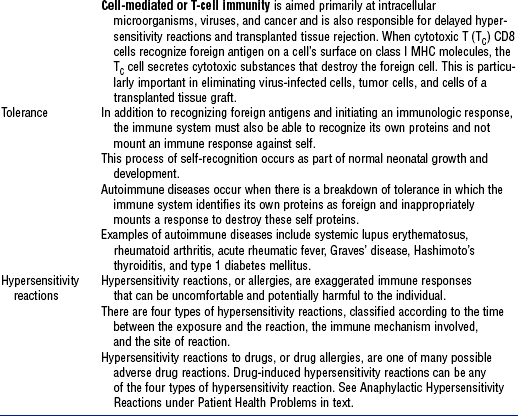
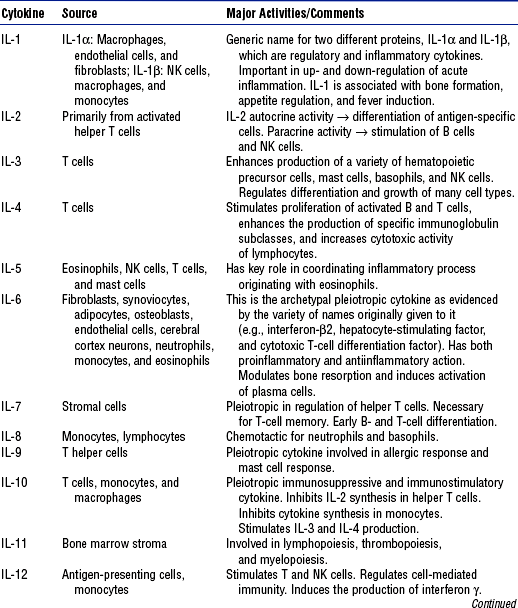
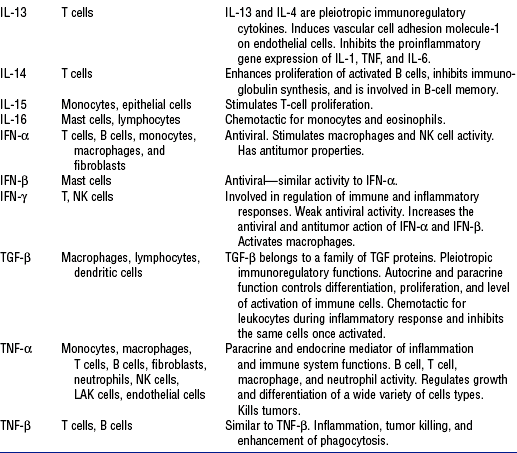
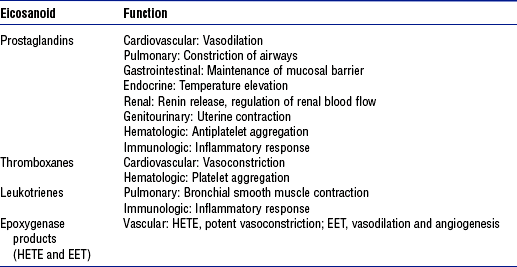
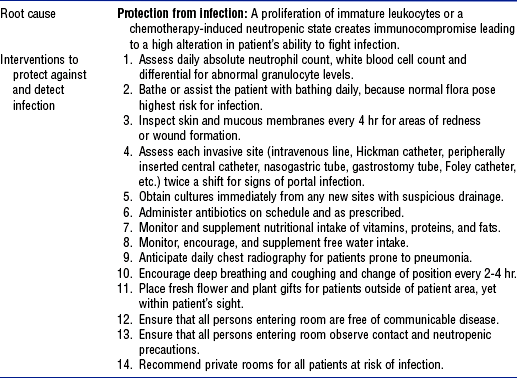
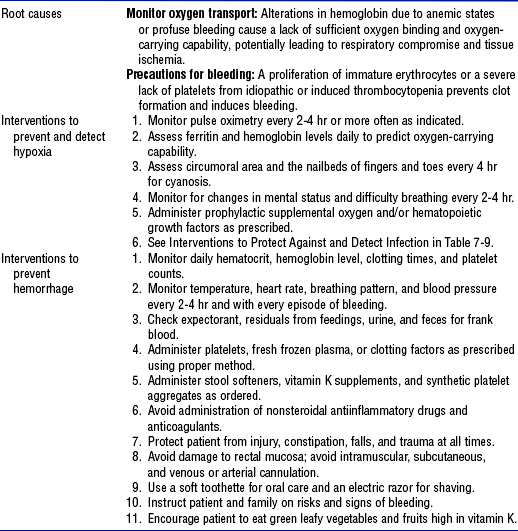
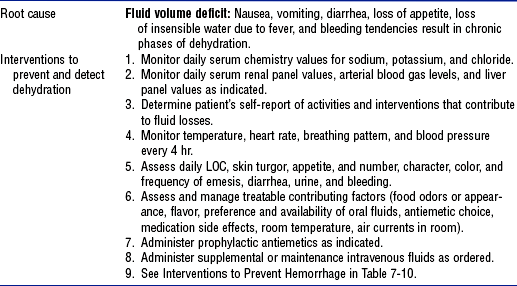
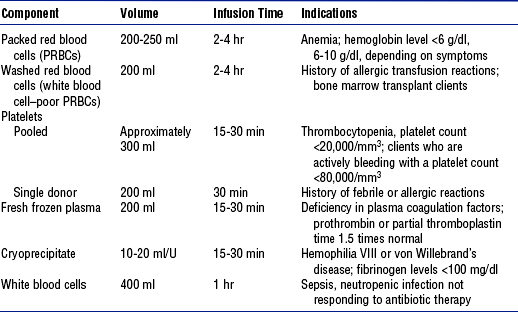
CHAPTER 7 (a) Spongy center of the bones where the hematologic and immunologic cell lines originate and mature before being released into the circulation (b) Present throughout the bones of the body, although the majority of the cells are produced in the vertebrae, ribs, sternum, pelvis, and proximal epiphyses of the femur and humerus (a) Located in the upper right quadrant of the abdomen in the peritoneal space below the diaphragm and under the rib cage. The liver receives 27% of the resting cardiac output—approximately 1350 ml of blood flow each minute—via the hepatic artery and portal vein. (b) Synthesizes various plasma proteins, including clotting factors and albumin. In addition, the liver clears damaged and nonfunctioning red blood cells (RBCs), or erythrocytes, from circulation. b. Components: See Table 7-1 and Figure 7-1 c. Functions: See Table 7-2 and Figure 7-2 i. Bone marrow (see preceding description) (a) The thymus is a bilobed lymphoid organ located in the mediastinum below the thyroid. Early in life, lymphocytes released from the bone marrow migrate to the thymus, where they mature into T cells before being released into the circulation. (b) During fetal development and throughout the first 2 years of life, the thymus grows rapidly. After puberty the thymus slowly involutes as the circulating, long-lived T-cell population is maximized. iii. The lymph system is a separate vessel system that collects plasma and leukocytes that are not returned to the circulatory system from the tissue capillary beds. This lymph fluid is filtered and returned to the circulatory system, so that appropriate tissue fluid pressures are maintained and edema is prevented. Lymph fluid is propelled along the system by the normal contraction of skeletal muscles. (a) Lymph fluid is a pale yellow liquid made up of plasma, leukocytes, enzymes, and antibodies; it lacks clotting factors and thus coagulates very slowly (b) Lymphatic capillaries and vessels are a network of open-ended tubes with one-way valves that collect lymph fluid from the tissues and eventually return it to the venous system via both the right lymphatic duct, which drains into the right subclavian vein, and the thoracic duct, which drains into the left subclavian vein (c) Lymph nodes are small, flat, bean-shaped patches of tissue located along the length of the lymphatic system that filter microorganisms from the lymph fluid before it is returned to the bloodstream (1) Lymph nodes can become swollen with white blood cells (WBCs), or leukocytes, that are responding to invading microorganisms if an infectious process is occurring in the area drained by the lymph node (2) Lymph nodes can also become swollen with metastatic cancer cells that have migrated away from the primary site and become trapped in the network of the lymph node iv. The spleen is a lymphoid organ located in the upper left quadrant of the abdomen that clears damaged or nonfunctioning RBCs and filters antigens from the blood for evaluation by lymphocytes b. Components: See Tables 7-3, 7-4, and 7-5, and Figure 7-3 TABLE 7-4 From Rankin JA: Biological mediators of acute inflammation, AACN Clin Issues 15(1):6, 2004. TABLE 7-5 Data from Boron W, Boulpaep EL: Medical physiology, Philadelphia, 2003, Saunders. EET, Cis-epoxyeicosatrienoic acid; HETE, hydroxyeicosatetraenoic acid. i. Many times a hematologic or immunologic problem is identified when the patent seeks medical attention for some other reason ii. Elements of the medical history indicating a potential or existing hematologic or immunologic problem include the following: (a) Recent, recurrent, or chronic infections (b) Cancer or prior treatment for cancer (c) Human immunodeficiency virus (HIV) infection (g) Any prolonged bleeding or delayed healing with prior surgeries and/or dental extractions (h) Receipt of a blood transfusion (j) Placement of a prosthetic heart valve (k) Placement of an indwelling venous access device, which indicates that the patient needed long-term venous access iii. Review of systems with the patient and/or family for signs and symptoms (a) General: Fatigue, weakness, lethargy, malaise, fever, chills, night sweats, dyspnea, restlessness, apprehension, pain, altered mental status, vertigo, dizziness, confusion (b) Skin: Pruritus, change in skin color, rash, unusual bruising, ulcers or other lesions (c) Head and neck: Headache, change in vision, sinus pain, epistaxis, gingival bleeding, sore throat, pain with swallowing, enlarged lymph nodes (d) Respiratory: Cough, hemoptysis, dyspnea, orthopnea (e) Cardiovascular: Palpitations, dizziness with position changes (f) Gastrointestinal: Change in eating habits, anorexia, abdominal fullness, nausea, vomiting, hematemesis, change in bowel habits, hematochezia, melena, pain with defecation, change in weight (g) Genitourinary: Hematuria, pain with urination, menorrhagia, enlarged inguinal lymph nodes (h) Musculoskeletal: Swelling of joints, tenderness or pain in the bones or joints b. Family history indicating a potential hematologic or immunologic problem: Hemophilia, sickle cell anemia, cancer, or death of a relative at a young age for reasons other than trauma c. Social history and habits that may assist with the diagnosis and treatment of the underlying condition, including the following: i. Any unusual or excessive exposure to chemicals (e.g., gasoline, benzene, solvents, glues, paints, varnishes) or radiation (e.g., x-rays) at work or in pursuit of a hobby ii. Any unusual dietary preferences, pica iii. Excessive alcohol consumption iv. Sexual preference, number of partners, history of sexually transmitted diseases, current contraceptive method, use of safe sex practices i. Current medications or a recent change in medication may suggest an underlying hematologic or immunologic problem. Always ask about over-the-counter medication use, because many of these preparations contain aspirin or nonsteroidal antiinflammatory drugs (NSAIDs). ii. Many medications used to treat nonhematologic and nonimmunologic problems can affect the hematologic and immunologic systems; examples of these drugs are the following: (a) Analgesics and antiinflammatory drugs (1) Chloramphenicol (Chloromycetin) (3) Paraaminosalicylic acid (PAS) (6) Trimethoprim-sulfamethoxazole (TMP-SMX, Bactrim, Septra) (e) Antidiabetic agents, such as chlorpropamide (f) Antineoplastic chemotherapy agents, such as (g) Antipsychotic agents, such as clozapine (Clozaril) (h) Antirheumatic agents, such as (i) Cardiovascular agents, such as (j) Diuretics, such as chlorothiazide (Diuril) (l) Immunosuppressives, such as 2. Nursing examination of patient (a) Temperature: Exceeds 101° F (38.3° C) (b) Skin: Pallor, jaundice, flushing, rash, petechiae, purpura, ecchymoses, hematomas, urticaria, integrity (c) Head and neck: Integrity of mucosal membranes, tongue appearance (e.g., smooth, coated), conjunctival bleeding (d) Chest: Shortness of breath, hemoptysis (e) Abdomen: Vomiting, hematemesis, hematuria, diarrhea, melena (b) Neck: Enlarged lymph nodes (c) Abdomen: Hepatomegaly, splenomegaly, enlarged lymph nodes in the axilla or groin 3. Appraisal of patient characteristics: Patients needing acute or life-saving care for hematologic disorders or for immunologic compromise come to critical care units as a result of their comorbidities or primary complications. The need for critical care may be brief or extended with quick to no recovery. Many hematologic and immunologic disorders are incurable. Occasionally, the focus is anticipated end-of-life care, although in no case is one able to predict with any certainty. Some patient characteristics that the nurse needs to assess for this population are the following: i. Level 1—Minimally resilient: A frail 27-year-old young man with acquired immunodeficiency syndrome (AIDS) dementia, severe stomatitis, and chronic diarrhea, who is unresponsive to antiretroviral therapy ii. Level 3—Moderately resilient: A 55-year-old woman with newly diagnosed acute lymphocytic leukemia following her second bone marrow transplant due to failed engraftment of the original donor stem cells iii. Level 5—Highly resilient: An 18-year-old man with a hemoglobin level of 8.0 g/dl recovering from a hypovolemic hemorrhage related to a table saw accident at his family’s farm i. Level 1—Highly vulnerable: A 45-year-old man with acute myelogenous leukemia who is neutropenic and has a lung abscess and thrombocytopenia ii. Level 3—Moderately vulnerable: A 36-year-old man, who is otherwise healthy, experiencing a type I hypersensitivity reaction to poison ivy hidden in the brush he was removing iii. Level 5—Minimally vulnerable: A petite 40-year-old woman with vitamin B12 deficiency anemia and alcoholism i. Level 1—Minimally stable: A 78-year-old widowed retired Air Force colonel who develops a viral pneumonia and confusion on the second day after admission for induction chemotherapy for acute lymphocytic leukemia ii. Level 3—Moderately stable: A 59-year-old housewife diagnosed with thrombocytopenia who has a platelet count of 60,000/mm3 iii. Level 5—Highly stable: A 28-year-old professor with lymphoma recovering in contact isolation from a methicillin-resistant Staphylococcus aureus toenail infection i. Level 1—Highly complex: A 48-year-old mother of four who develops disseminated intravascular coagulation (DIC) after a bilateral mastectomy and transversus rectus abdominis myocutaneous (TRAM) flap surgical reconstruction ii. Level 3—Moderately complex: A 19-year-old man with a diagnosed HIV infection that he wishes to be kept confidential from his parents and siblings iii. Level 5—Minimally complex: A 35-year-old accountant in whom autoimmune thrombocytopenic purpura (ATP) is diagnosed following a prolonged case of the flu i. Level 1—Few resources: A 47-year-old housekeeper with rheumatoid arthritis who provides the sole income for a family of six and receives a diagnosis of leukemia ii. Level 3—Moderate resources: A 32-year-old Spanish-speaking migrant worker who contracted hepatitis C after a blood transfusion and has a bilingual sister who is a United States citizen and a social worker iii. Level 5—Many resources: A 49-year-old chief executive officer of a major computer software company who is hospitalized for maintenance chemotherapy i. Level 1—No participation: An obese 26-year-old woman in anaphylactic shock with pulmonary edema and oral intubation ii. Level 3—Moderate level of participation: A 67-year-old salesman who is learning about home care for a Hickman catheter iii. Level 5—Full participation: A 32-year-old woman with AIDS who is compliant with antiretroviral therapy, exercise, and diet recommendations g. Participation in decision making i. Level 1—No participation: A 30-year-old children’s tennis coach who chooses to let God’s will be done after the physician team decides not to render further treatment for advanced cancer of the thoracic spine ii. Level 3—Moderate level of participation: A 56-year-old Mediterranean man who defers to his wife for decisions about treating his blood disorder iii. Level 5—Full participation: A 37-year-old kindergarten teacher who asks to know platelet counts before consenting to each platelet transfusion i. Level 1—Not predictable: An elegant 82-year-old grandmother with newly diagnosed chronic myelocytic leukemia ii. Level 3—Moderately predictable: A 29-year-old day care worker receiving a second bone marrow transplant (BMT) after complete engraftment of the primary BMT stem cells iii. Level 5—Highly predictable: A 27-year-old man with cognitive and behavioral challenges from AIDS dementia a. Laboratory: See Table 7-7 for normal values TABLE 7-7 Data from Kee JL: Laboratory diagnostic tests with nursing implications, ed 5, Stamford, Conn, 1999, Appleton & Lange. ii. Sputum culture: Detects and identifies microorganisms in the sputum (a) Urinalysis can detect gross amounts of blood or protein in the urine (b) Urine cultures detect and identify microorganisms in the urine (c) Urine protein electrophoresis determines the levels of proteins excreted in the urine, particularly the levels of immunoglobulins iv. Stool occult blood test (Hemoccult): Detects microscopic amounts of blood in the stool i. Spleen ultrasonography is used to estimate the size of the spleen ii. In a liver-spleen scan, a radioactive tracer is used to evaluate the size as well as the function of the liver and spleen iii. In a gallium scan, a radioactive tracer is used to detect the presence of malignant tissue, particularly malignant lymphoid tissues iv. In a lymphangiogram, contrast dye is used to radiologically visualize the lymph system, particularly the size and architecture of lymph nodes i. Bone marrow biopsy includes aspiration of bone marrow fluid and removal of a needle core biopsy sample of the bone marrow tissue for pathologic examination ii. In a lymph node biopsy, one or more lymph nodes are removed for pathologic examination d. Skin tests: Barometers of immune functioning, pointing out hyposensitivities or hypersensitivities to a particular antigen. Examples of allergens used in skin testing are allergenic extracts (e.g., dust, pollen, animal dander); purified protein derivative (PPD) for tuberculin skin tests; mumps virus; Candida albicans; and skin fungi. 1. Susceptibility to infection i. Immune compromise and/or coagulopathy increases patient risk for opportunistic and host infections ii. Clinical findings include reports of fever, chills, night sweats, sore throat, cough, malaise, pain with swallowing, pain with urination, pain with defecation, diarrhea, reddened areas, sore areas, and swollen areas (these symptoms may not be present if the patient is neutropenic and unable to mount a WBC response); flushing, lethargy, skin warm to touch; abnormal vital signs—temperature exceeding 101° F (38.3° C), hypotension, tachycardia; WBC count lower than 1500/mm3, absolute neutrophil count (ANC) lower than 500/mm3 i. Vital signs within normal limits for the patient ii. Absence of signs or symptoms of active infection iii. Maintenance of the WBC count within an acceptable range iv. Patient’s and family’s verbalization of an understanding of the underlying pathology and infection prevention c. Collaborating professionals on health care team d. Interventions: See Table 7-9 TABLE 7-9 Leukocyte Intervention Activity Bundle From Schneider S: Interventions for hematologic problems. In Ignatavicius DD, Workman ML, editors: Medical-surgical nursing: critical thinking for collaborative care, ed 4, Philadelphia, 2002, Saunders. 2. Increased risk for hemorrhage i. Disease and/or treatment creates an altered state of protection against bleeding ii. Clinical findings include reports of unusual bruising, prolonged bleeding, hematemesis, hemoptysis, hematochezia, melena, hematuria, menorrhagia i. No evidence of spontaneous bleeding ii. Maintenance of platelet counts and levels of clotting factors within an acceptable range iii. Patient’s and family’s verbalization of an understanding of the underlying pathology and bleeding precautions c. Collaborating professionals on health care team d. Interventions: See Table 7-10 TABLE 7-10 Erythrocyte Intervention Activity Bundle From Schneider S: Interventions for hematologic problems. In Ignatavicius DD, Workman ML, editors: Medical-surgical nursing: critical thinking for collaborative care, ed 4, Philadelphia, 2002, Saunders. 3. Impaired respiratory gas transport: See Chapter 2 4. Impaired fluid volume regulation (see also Chapter 5) i. Fever, vomiting, diarrhea, hemorrhage, and shock deplete body fluid volume ii. Clinical findings include reports of thirst, sweating, vomiting, polyuria, diarrhea, lightheadedness; pallor, mucosal dryness, loss of skin turgor, decreased venous filling; abnormal vital signs—fever, tachycardia, hypotension, changes in orthostatic vital signs; decreased urine output and concentrated urine with a specific gravity exceeding 1.020; altered mental status c. Collaborating professionals on health care team d. Interventions: See Table 7-11 TABLE 7-11 Dehydration Intervention Activity Bundle From Schneider S: Interventions for hematologic problems. In Ignatavicius DD, Workman ML, editors: Medical-surgical nursing: critical thinking for collaborative care, ed 4, Philadelphia, 2002, Saunders. i. Administer IV fluids and blood products as prescribed (a) Transfuse blood products (Table 7-12) TABLE 7-12 Indications for Treatment with Blood Components From Schneider S: Interventions for clients with hematologic problems. In Ignatavicius DD, Workman ML, editors: Medical-surgical nursing: critical thinking for collaborative care, ed 4, Philadelphia, 2002, Saunders, chap 40. (b) Keep in mind special considerations related to blood product administration (Table 7-13 and Box 7-1)
Hematologic and Immunologic Systems
SYSTEMWIDE ELEMENTS
Patient Assessment
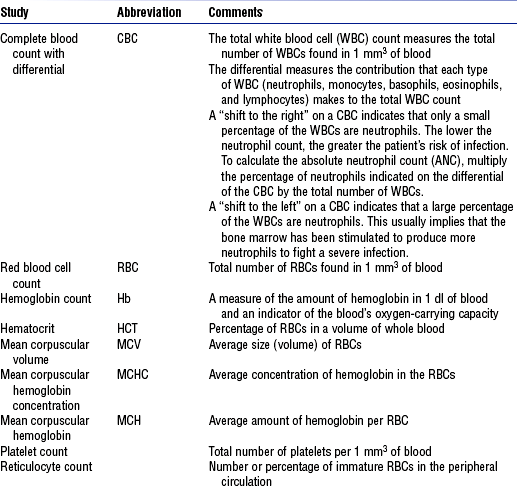
Laboratory Test
Reference Values
Description
(White blood cell (WBC) count
4500-10,000/mm3
Total number of leukocytes
Differential WBC:
Part of CBC; indicates distribution of five types of leukocytes
Neutrophils
2500-7000/mm3
Segments
2500-6500/mm3
Bands
0-500/mm3
Monocytes
200-600/mm3
Basophils
40-100/mm3
Eosinophils
100-300/mm3
Lymphocytes
1700-3500/mm3
Red blood cell (RBC) indices:
Erythrocyte indicators for anemia
RBC count
Men
4.6-6.0 million/mm3
Women
4.0-5.0 million/mm3
Mean corpuscular volume (MCV)
80-98 mm3
Indicates size of RBC
Mean corpuscular hemoglobin (MCH)
27-31 pg
Indicates weight of hemoglobin in RBC
Mean corpuscular hemoglobin concentration (MCHC)
32%-36%
Hemoglobin per volume RBC
RBC distribution width (RDW)
11.5-14.5 Coulter S
Size (width) difference of RBCs
Hemoglobin (Hb) level
Iron composition of RBC for oxygen-carrying capability
Men
13.5-17 g/dl
Women
11.2-115 g/dl
Hematocrit (HCT) of blood
Measure of the percentage of the total blood volume that is made up by RBCs
Men
40%-54%
Women
36%-46%
Panic value
<15% and >60%
Reticulocyte count
0.5%-1.5%
Indicator of bone marrow activity
Erythrocyte sedimentation rate
Rate at which erythrocytes settle (sediment) in unclotted blood
Men
0-9 mm/hr (Wintrobe method)
Women
0-15 mm/hr (Wintrobe method)
Serum ferritin level
An indicator of protein stores of iron in the tissues, where 1 ng/ml ferritin = 8 mg stored iron
Men
15-445 ng/ml
Women
10-235 ng/ml
Postmenopausal
15-310 ng/ml
Total iron-binding capacity (TIBC)
250-450 mg/dl
Total (maximum) iron-binding capacity of transferrin for transport of iron to marrow for hemoglobin synthesis
Platelet count (PLT)
150,000-400,000/mm3
Measure of thrombocytes available for coagulation of blood
Fibrin split products (FSP)
2-10 mg/ml
Indicator of fibrin degradation products acting as anticoagulant in continuous bleeding associated with hemorrhage
Clotting times
10-13 sec
Measures clotting factor ability
Prothrombin time (PT)
Partial thromboplastin time (PTT)
60-70 sec
Detects deficiencies in clotting factors
International normalized ratio (INR)
2.5-3.5
Standard for warfarin-sensitive PT
Patient Care

Hematologic and Immunologic Systems
Get Clinical Tree app for offline access