Hematologic and immunologic problems
 Just the facts
Just the factsIn this chapter, you’ll learn:
anatomy and physiology of the hematologic and immune systems
normal function of blood cells and the role of genetics in the hematologic and immune systems
tests used to diagnose hematologic and immunologic problems
treatments and procedures for children with hematologic and immunologic problems
hematologic and immunologic disorders that affect children.
Anatomy and physiology
The hematologic and immune systems are separate but interrelated. They help the body fight infection or invaders through different mechanisms but usually work together for the same goal. Both systems essentially arise from an organ known as bone marrow which, although housed within the bones, has little relationship to the skeletal system.
|
Hematologic system
Bone marrow contains the essential element in the hematologic system: the stem cell. The stem cell is sometimes referred to as the pluripotential stem cell, meaning it has the ability to
transform into more than one type of blood cell. Every blood cell in the body arises from a stem cell.
transform into more than one type of blood cell. Every blood cell in the body arises from a stem cell.
Did you say organ system?
Although it’s a fluid, blood is one of the body’s major organ systems. It continually circulates through the heart and blood vessels, carrying vital elements to every part of the body.
Blood formation
Early in utero, the process of blood formation, called hematopoiesis, occurs in the liver and spleen. These organs retain some hematopoietic ability throughout life. After birth, the red bone marrow becomes the main site of hematopoiesis.
|
Yellow with age
In infants and young children, all bones contain red bone marrow (red from the production of red blood cells [RBCs]) and are, therefore, capable of hematopoiesis. However, as the child approaches adolescence and bone growth ceases, the bone marrow in many bones can’t form blood cells because the marrow has transformed to yellow bone marrow (yellow from fat deposits), although it can usually revert to red bone marrow during times of increased blood cell demand. Only the ribs, sternum, vertebrae, and pelvis continue to contain red bone marrow and produce blood cells.
Have a blast
The stem cells contained in the red bone marrow create primitive blood cells called blast cells. Blast cells are the least mature form of blood cell and are the precursors to RBCs, white blood cells (WBCs), and platelets. These cells are normal and shouldn’t be confused with the blast cells seen in leukemia and other cancers.
Like a fine wine
These blast cells then stay in the bone marrow to mature. The maturation of blood cells, called differentiation, occurs in stages; thus, in normal bone marrow, you can see different forms of all the blood cell lines. (See Human blood cell development.) Mature blood cells travel by blood throughout the body to perform specific functions.
Blood components
Blood is composed of plasma and cells. Plasma is the fluid portion of the blood. It’s 90% water and 10% solutes, such as proteins, electrolytes, albumin, clotting factors, anticoagulants, antibodies,
and dissolved nutrients. The three main cell types in the blood originate from blast cells and include:
and dissolved nutrients. The three main cell types in the blood originate from blast cells and include:
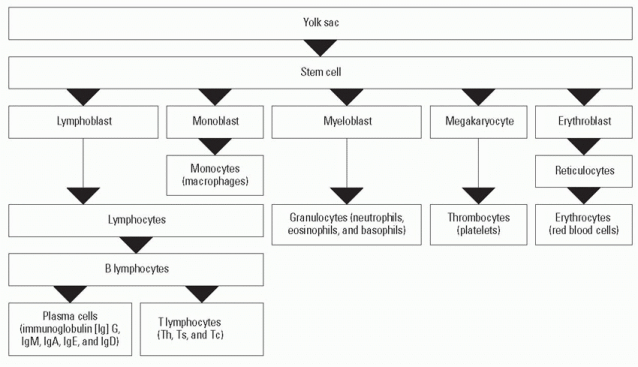
Human blood cell development
All blood cell types originate from the same stem cell. The chart below shows how this stem cell becomes differentiated, developing into each blood cell type.
|
RBCs
In addition to the bone marrow, some RBCs are stored in the liver or spleen. RBCs carry oxygen to the tissues and carry carbon dioxide away from tissues. When tissue is low on oxygen (hypoxia), a hormone from the kidneys called erythropoietin stimulates the bone marrow to produce more RBCs. Synthetic forms of erythropoietin are now used to stimulate RBC production in premature neonates and patients receiving chemotherapy to help them maintain higher blood cell levels.
The cycle of life—RBC style
An RBC’s life span is approximately 120 days, and an important waste product of RBC death is bilirubin. Bilirubin binds with albumin for transport to the liver cells to conjugate with glucuronide, forming direct bilirubin. Because unconjugated bilirubin is fat-soluble and can’t be excreted in urine or bile, it may escape to extravascular tissue, especially fatty tissue and the brain, resulting in hyperbilirubinemia and skin that appears icteric (or jaundiced). Too much bilirubin may result in brain damage—a condition known as kernicterus. In newborns, the normal range of bilirubin levels are determined by the baby’s age in hours. For instance, an infant who is 48 hours old will have a different range of acceptable levels than does an infant who is 96 hours old. Other things that may place a newborn at risk for hyperbilirubinemia are being born premature, having a sibling who has had hyperbilirubinemia, or having a blood group incompatibility with the mother (such as the mother having an O+ blood type and the baby having an A+ blood type).
Oxygen is carried in the cell in a protein (globin) and iron (heme) structure known as hemoglobin. If adequate amounts of iron aren’t available, the protein structure can’t be formed and RBCs can’t carry their normal amount of oxygen. Lead can also replace iron in the molecule, causing toxicity.
WBCs
WBCs fight different types of infection that occur in or on the body; each type of WBC has its own role in fighting infection. The two main categories of WBCs are granular leukocytes (granulocytes) and nongranular leukocytes (agranulocytes). (See Two types of leukocytes.)
Great granulocytes, Batman!
Granulocytes include:
neutrophils, which help devour invading microorganisms, such as bacteria, by phagocytosis
eosinophils, which act in allergic reactions and may defend against large parasites and lung and skin infections
basophils, which release heparin and histamine, are involved in inflammatory and infectious reactions, and are known as mast cells when they exist in body tissues.
Not a granule to be found
Agranulocytes include:
lymphocytes, which are the main cells that fight infections and include natural killer (NK) cells, B cells, and T cells
monocytes, which, along with neutrophils, help devour invading microorganisms by phagocytosis and also form macrophages in the body tissues.
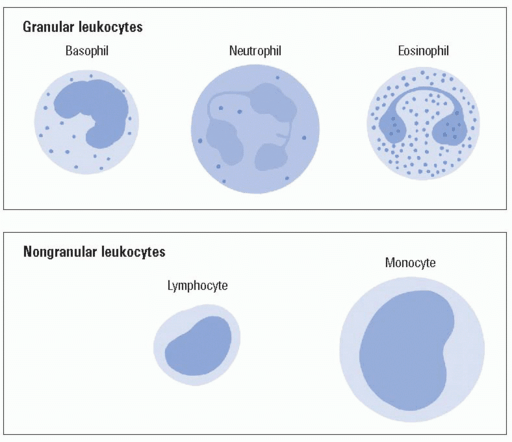
Two types of leukocytes
Leukocytes vary in size, shape, and number and are characterized as granular and nongranular.
Granular
Granular leukocytes (granulocytes) are the most numerous. They include:
basophils, which contain cytoplasmic granules that stain readily with alkaline dyes
neutrophils, which are finely granular and recognizable by their multinucleated appearance
eosinophils, which stain with acidic dyes.
Nongranular
Nongranular leukocytes have few, if any, granulated particles in the cytoplasm. They include:
lymphocytes
monocytes.
|
Platelets
Platelets adhere to one another and plug holes in vessels or tissues where there’s bleeding. This action is part of a larger coagulation (clotting) process. Platelets also release serotonin at injury sites. Serotonin, a vasoconstrictor, decreases blood flow to the injured area. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, and naproxen may affect platelet aggregation.
Hemostasis
Hemostasis is a complex process by which the body controls bleeding. When a blood vessel ruptures, local vasoconstriction and platelet clumping (aggregation) at the injury site initially help prevent hemorrhaging.
Like a waterfall
Activation of the coagulation system, called the extrinsic cascade, involves the release of thromboplastin from the damaged tissue cells. However, formation of a more stable clot requires initiation of the complex clotting mechanism known as the intrinsic cascade system.
When endothelial vessel injury or a foreign body in the bloodstream activates the intrinsic cascade, activating factor XII triggers clotting. Finally, prothrombin is converted to thrombin and fibrinogen to fibrin, which is necessary for creation of a fibrin clot.
Immune system
The body protects itself from foreign invaders, such as bacteria, viruses, parasites, and fungi, through the organs and cells of the immune system. The components of the immune system work together to recognize “self” from “nonself” and to rid the body of those substances recognized as “non-self.”
Immune system organs
Immune system organs and tissues are described as lymphoid because they’re all involved with the growth, development, and dissemination of lymphocytes. These organs and tissues include:
lymph nodes
thymus
spleen
tonsils
Peyer patches in the intestine.
Lymph nodes
Lymph nodes are small, oval-shaped structures located along a network of lymph channels. Most abundant in the head, neck, axillae, abdomen, pelvis, and groin, they help remove and destroy antigens (substances capable of triggering an immune response) that circulate in the blood and lymph. Lymph nodes filter lymphatic fluid and return it to the bloodstream.
Lymphocytes in waiting
Lymph nodes filter foreign invaders, such as viruses and bacteria, and can serve as waiting stations for lymphocytes that might be needed in that area to fight infection.
|
Nodes of concern
In children, the lymphatic system grows rapidly between ages 3 and 6 years. At this age, slightly swollen (less than 0.5 cm) lymph nodes in the neck and groin areas are common. Lymph nodes that should cause concern are:
enlarged (greater than 1 cm in diameter), firm, painless, and fixed to the skin (malignancy)
painful, soft, and producing heat (local inflammation or infection)
nodes in the supraclavicular, infraclavicular, or axillary regions.
Thymus
The thymus is located in the mediastinal area of the chest and may look quite large on the chest X-ray of a neonate. The thymus is largest in the preadolescent period. After adolescence, it begins to shrink in size.
The thymus uses hormones to enable maturation of lymphocytes, produced by the bone marrow, into T lymphocytes (T cells). The mature T cells can then function normally.
Spleen
The spleen functions as a reservoir for blood and blood cells. It also acts like a screen to filter out unwanted invaders and help break up old RBCs that lose their elasticity with age and can’t squeeze through the fine mesh of the spleen. The spleen is particularly good at filtering out one specific bacterium called Streptococcus pneumoniae. Children without a spleen or with a nonfunctioning spleen (such as those with sickle cell disease) are more at risk for invasive streptococcal infections and should be put on prophylactic penicillin (until the age of at least 5 years) and will need immediate antibiotics if they have a fever.
Tonsils
The tonsils consist of lymphoid tissue that serves as a storage site for lymphocytes and can also produce some lymphocytes. In children, the tonsils may normally be slightly enlarged between ages 3 and 6 years (while the immune system is at its peak of development).
Sounds of silence?
Parents of a 3- to 6-year-old child will commonly report that he snores. Snoring at this age is usually due to the enlarged tonsils partially obstructing the airway during sleep.
|
Immune system cells
All immune system cells are produced in bone marrow. The main cells of the immune system are B cells (B lymphocytes), phagocytes, and T cells (T lymphocytes).
B cells
B cells, which are involved in humoral immunity, produce antibodies. Each B cell is programmed to make a specific antibody. In humoral immunity, a B cell will divide and differentiate into plasma cells when it encounters its triggering antigen. The plasma cells will secrete antibodies to the antigen.
To find and bind
These antibodies then travel in the blood and lymph, which circulate throughout the body. When the antibodies find the antigen, they bind to it to tag it so other immune system cells can destroy it.
Gobs of globulins
Some antibodies are proteins that perform special functions and are called immunoglobulins. There are five types of immunoglobulins (Igs) produced by B cells:
 IgA defends external body surfaces and is present in colostrum, saliva, tears, and nasal fluids as well as respiratory, gastrointestinal (GI), and genitourinary secretions (neonates have small amounts of this Ig and are more susceptible to an overgrowth of organisms in mucous membranes such as oral Candida).
IgA defends external body surfaces and is present in colostrum, saliva, tears, and nasal fluids as well as respiratory, gastrointestinal (GI), and genitourinary secretions (neonates have small amounts of this Ig and are more susceptible to an overgrowth of organisms in mucous membranes such as oral Candida). IgD is found on the surface of B cells and functions in controlling lymphocyte activation or suppression.
IgD is found on the surface of B cells and functions in controlling lymphocyte activation or suppression. IgE is the antibody responsible for hypersensitivity reactions; it has an immediate response to an antigen and stimulates the release of heparin and histamine from mast cells.
IgE is the antibody responsible for hypersensitivity reactions; it has an immediate response to an antigen and stimulates the release of heparin and histamine from mast cells. IgG makes up the majority of plasma antibodies and is the main antibacterial and antiviral antibody; transfusions of IgG specific for viral diseases, such as varicella (chickenpox), are useful in treating children who are exposed but have decreased immune function (such as those on chemotherapy).
IgG makes up the majority of plasma antibodies and is the main antibacterial and antiviral antibody; transfusions of IgG specific for viral diseases, such as varicella (chickenpox), are useful in treating children who are exposed but have decreased immune function (such as those on chemotherapy). IgM is the first Ig produced during an immune response; because it’s very large, IgM is usually seen only in the blood and can’t pass into tissues to fight infections.
IgM is the first Ig produced during an immune response; because it’s very large, IgM is usually seen only in the blood and can’t pass into tissues to fight infections.If humoral immunity is all Greek to you, you’re right! To remember what humoral immunity is, think Greek. B-cell antibodies travel in the blood and lymph, which the ancient Greeks called the humors of the body.
|
Phagocytes
Phagocytes are immune cells that engulf, kill, and digest particulate matter and foreign invaders. Phagocytes include neutrophils, monocytes, and macrophages. Macrophages are a type of monocyte; they’re versatile scavenger cells found in tissues throughout the body. In addition to their phagocytic action, macrophages:
T cells
T cells are responsible for cell-mediated immunity. Lymphocytes derived from bone marrow migrate to the thymus, where they mature into T cells. In cell-mediated immunity, T cells directly attack antigens, including bacteria, viruses, and other pathogens. They have the ability to identify an antigen (target cell) and produce lymphokines that attack the target directly. Cell-mediated immunity is also responsible for tissue and transplant incompatibility rejections and delayed hypersensitivity reactions (such as a positive tuberculin test response).
There’s definitely a T in team
Different types of T cells work together to create the best immune response possible. Helper T cells (CD4+ cells) stimulate B cells to mature into plasma cells that produce Igs to fight antigens and to also remember them if they occur again in the future.
Search and destroy
The helper T cells also help the killer T cells (CD8+ cells) to more readily recognize the antigen and attack directly. Killer T cells bind to the surface of the invading antigen and disrupt the cell membrane, causing the antigen’s destruction.
Complement system
The complement system is composed of several proteins that are important in the inflammatory process. It’s activated by the antigen-antibody complexes (classic pathway) or toxins released by antigens (alternate pathway). The complement system is one of the body’s primary defenses; it immediately assists in mast cell degradation, which enhances vascular permeability and assists in attracting neutrophils to the site.
To remember where B cells and T cells mature, mind your Bs and Ts:
B cells = Bone marrow
T cells = Thymus
|
Hypersensitivity
Hypersensitivity reactions are one of the body’s immune responses to an antigen and may be immediate (occurring within minutes) or delayed (may take several hours). There are four types of hypersensitivity reactions, each serving a specific function.
Type I: Atopy or anaphylaxis
In some people, certain antigens (allergens) induce B-cell production of IgE, which binds to receptors on mast cell surfaces. The mast cells degranulate and release various mediators, including heparin, histamine, and prostaglandins. These mediators cause vasodilation, bronchospasm, edema, and mucus secretion, leading to such symptoms as wheezing, hives, and rhinorrhea.
Second time around
IgE is produced in sufficient quantities only with repeated exposure and, therefore, may have little effect with occasional allergic reactions. Because severe reactions may not occur with the first exposure to a drug or allergen, the body may only produce antibodies, which will react with the second exposure. In severe reactions, anaphylaxis may occur, resulting in respiratory and cardiac arrest. Someone may not react to an antibiotic the first time—even if they are allergic—but react the second or third time.
Type II: Cytotoxic response
IgG and IgM are involved in tissue-specific hypersensitivity reactions (type II). The type II hypersensitivity response generally involves the destruction of a target cell by an antibody directed against cell-surface antigens.
Deadly complement
Binding of an antigen and an antibody activates the complement system, which ultimately disrupts the cellular membranes, causing cell death. Cytotoxic T cells and NK cells also contribute to tissue death in type II hypersensitivity. Examples of type II hypersensitivity include transfusion reactions and hemolytic disease in the neonate.
Type III: Immune complex
Immune complex-mediated (type III) reactions are similar to type II in that the complex recognizes the same type of antigen. However, in type II, the antigen is found on the cell or organ surface, whereas in type III, the antigen is free-floating and is attacked regardless of where it’s located. If the antigens are left in the
circulatory system, they may cause inflammatory reactions that can result in vessel wall damage and changes in permeability.
circulatory system, they may cause inflammatory reactions that can result in vessel wall damage and changes in permeability.
Attack first, ask questions later
Autoimmune disorders are caused by type III reactions in which the immune complexes have difficulty distinguishing between normal and abnormal tissue and may attack both. These disorders include systemic lupus erythematosus (SLE), juvenile rheumatoid arthritis, and glomerulonephritis.
Type IV: Cell-mediated hypersensitivity
In type IV hypersensitivity, antigen is processed by macrophages and presented to T cells.
Release the lymphokines!
T cells function by releasing lymphokines, which recruit and activate other lymphocytes, monocytes, macrophages, and polymorphonuclear leukocytes. The coagulation (kinin) and complement pathways also contribute to tissue damage in this type of reaction. The most serious reactions occur with transplantation when the transplanted tissue is perceived as foreign and attacked. Type IV reactions also occur with exposure to plants or substances that trigger a response resulting in contact dermatitis.
Diagnostic tests
Tests used to diagnose hematologic and immunologic problems in children include allergy skin testing, bone marrow aspiration and biopsy, and CBC with differential.
Allergy skin testing
Children commonly have short-term allergic problems that may disappear as the child grows older. A child older than age 2 years with a history of chronic allergic symptoms, such as coughing, runny nose, watery eyes, and upper respiratory congestion, may need to be evaluated for allergies. Symptom management with medications (such as antihistamines) is recommended until the child reaches age 4 years or older. If symptoms persist beyond this age, allergy testing may be warranted.
|
RAST to the rescue
Allergy skin testing examines specific allergic antigens. The radio-allergosorbent test (RAST) identifies antigens in the blood that are causing an immunologic reaction mediated by IgE. The quantity of circulating IgE correlates well with the clinical severity of the allergic symptoms.
The family tree of allergy
When testing is started, a pediatric allergist obtains a detailed history from the family and the child in an attempt to identify the specific antigen. Allergy skin testing entails injecting small amounts of common allergic antigens under the skin (intradermal) to assess for localized reaction. RAST is recommended when there’s a strong suspicion that a specific substance is responsible for the allergy problem.
Nursing considerations
Allergy shots run the risk of causing an anaphylactic reaction, and the nurse should be prepared to provide emergency care. The child should remain in the facility for at least 15 minutes after the shot to be monitored for an injection site reaction and signs of an impending anaphylactic reaction.
A song and a wiggle
The child should be prepared for injections (for testing and treatment) and given a “job” to do such as holding very still. Distraction techniques (such as telling the child to wiggle his toes or sing a song) may help reduce the child’s anxiety and enhance cooperation.
Bone marrow aspiration and biopsy
Bone marrow aspiration and bone marrow biopsy are slightly different tests that are usually done for the same reason. Both tests are done to view the integrity of function of the bone marrow as an organ.
Bone bank withdrawal
In bone marrow aspiration, a specially designed needle with a stylet is inserted into the center of the bone to withdraw bone marrow. The front and back crests of the iliac bone are most commonly sampled in children. In a bone marrow biopsy, a section of bone is taken, revealing all levels of bone and bone marrow.
|
To aspirate or biopsy—that is the question
Ideally, the marrow should show a wide variety of cell types in various stages of maturation. Primary, malignant, blast leukemic cells with few normal cells are seen in leukemia. When a solid tumor, such as neuroblastoma or rhabdomyosarcoma, has metastasized to the bone marrow, a biopsy may be more helpful in showing the clumps of tumor cells among some normal cells. Both tests show whether the bone marrow is functioning normally.
Nursing considerations
Bone marrow aspiration or biopsy can be performed under light general anesthesia or with a local injection to numb the area. An oral or intravenous (I.V.) sedative may be given before the procedure. Prepare the child for the test with an age-appropriate explanation, and monitor for sedation or adverse effects of anesthesia. Tell the child that a parent may stay with him during the test.
In addition, follow these steps:
Apply a pressure dressing after the procedure, which should be sufficient to stop blood loss.
Be aware of the proper handling and labeling of the specimens to prevent the need to repeat the aspiration; multiple tests may be performed on the specimens obtained.
Provide a mild analgesic as ordered; postprocedure pain is short-term after aspiration and consists of a dull ache for about 24 hours after biopsy.
CBC with differential
One of the most important tests for general screening for hematologic and immune problems is the complete blood count (CBC). An additional test that may be ordered is the differential, which is used to determine the percentage of WBCs that are present.
Decrease = disorder
In general, the CBC reveals the numbers of the three main blood cells (WBCs, RBCs, and platelets). Decreased values in any cell line may be an indication of a disorder related to the bone marrow or the immune system or may be the result of infection.
What’s up with the whites?
WBC counts vary with age.
A healthy neonate typically has higher counts of 15,000 to 20,000/µl, with 60% to 70% being lymphocytes.
The typical adult WBC count of 5,000 to 10,000/µl is generally present in children after age 2 years.
Counts over 15,000/µl in children older than age 6 months should be considered high and abnormal (although this doesn’t necessarily indicate serious illness).
|
Seeing red
Although the RBC count is included in the CBC, the hemoglobin level and hematocrit are usually used as a gauge of the number of RBCs present:
Hemoglobin is a molecule responsible for carrying oxygen to the tissue and is somewhat affected by age. Higher levels of 15 to 20 g/dl are present in the neonate but, within 2 months, the normal range will be 12 to 15 g/dl.
Hematocrit is approximately three times the level of hemoglobin, and normal ranges are 35% to 45%. This level is affected by hydration level and may be elevated with dehydration and decreased if the child has fluid overload.
Pediatric and parental platelets
Platelet counts should be between 150,000 and 500,000/mm3, regardless of age.
Nursing considerations
Prepare the child for venipuncture and allow the parent to be present to comfort the child. After the venipuncture, monitor the site for signs of continued bleeding.
Treatments and procedures
Treatments and procedures used for children with hematologic and immunologic problems include blood transfusion and bone marrow transplantation.
Blood transfusion
Blood transfusion is necessary if levels of blood cells become too low or if the child is experiencing symptoms caused by a decrease in the number of available cells.
Pump up the vascular volume
Generally, transfusions are aimed at increasing volume within the vascular system, increasing RBCs to improve oxygenation, or increasing the number of platelets to reduce or correct bleeding problems:
Whole blood is transfused if trauma with bleeding occurs and the risk of shock is present because of decreased intravascular
volume. Blood loss from surgery may also require whole blood to replace cells and plasma.
In children who have decreased levels of RBCs only, transfusion with packed RBCs is indicated. Because plasma is removed from these concentrated RBCs, transfusion increases intravascular volume only mini mally (only small amounts of WBCs and platelets are contained in the transfused RBCs).
Platelets are transfused when counts are below 60,000/mm3 with symptoms of active bleeding. If the count is below 20,000/mm3, transfusion with platelets is recom mended due to the risk of spontaneous intracranial bleeding, which can lead to death.
Nursing considerations
Prepare the child and his parents for the procedure. Reassure the parents (and the child, if old enough) about the measures that are taken to ensure the safety of transfused blood products.
In addition, follow these steps:
Double-check the child’s name, identification number, name bracelet, ABO group, and Rh status with another nurse to help prevent hemolytic transfusion reactions. If there’s a discrepancy, don’t administer the blood product and notify the blood bank immediately.
Start the blood transfusion within 30 minutes after it arrives from the blood bank. If you can’t start the transfusion in this timeframe, return the blood product to the blood bank.
Take baseline vital signs just before the start of the transfusion and every 15 minutes during the transfusion.
Bone marrow transplantation
Bone marrow transplantation is used to treat such diseases as acute leukemia, aplastic anemia, and severe combined immunodeficiency disease. The hematopoietic stem cells may be malignant themselves or may have been destroyed by aggressive therapy for malignant disease. Sometimes the stem cells are absent or just don’t work like aplastic anemia.
|
|
Share and share alike
With transplantation, marrow or stem cells are transplanted from a twin or another human leukocyte antigen (HLA)-identical donor (usually a sibling) in the hope that the new
stem cells will produce normal, healthy cells. Autologous bone marrow transplantation is another option for some patients. In this procedure, the patient’s own marrow or stem cells are harvested from healthy tissues or harvested and then treated to remove malignant cells. The cells are then returned to the patient.
stem cells will produce normal, healthy cells. Autologous bone marrow transplantation is another option for some patients. In this procedure, the patient’s own marrow or stem cells are harvested from healthy tissues or harvested and then treated to remove malignant cells. The cells are then returned to the patient.
A harvest of plenty
During bone marrow harvest, marrow is extracted from a matched donor with multiple bone marrow aspirations; 200 to 500 ml of marrow are collected, processed, and purified.
Getting ready to receive
The recipient is given high-dose chemotherapy to destroy the malignant marrow and WBCs that might cause a reaction. On the day of the transplant, the recipient is given total-body radiation to further destroy components of the malignant bone marrow and to destroy WBCs throughout the body that may identify the transfused cells as foreign and destroy them.
From harvest to seed
The collected donor marrow, which looks like a blood product, is then transfused through an I.V. line. If the transfusion is successful, the transplanted stem cells will reseed the bone marrow and start producing normal blood cells.
Graft battles host
A great risk after bone marrow transplantation is that the new bone marrow may produce B cells that interpret the normal body tissue as being foreign and attack it. This is commonly seen in the skin, eyes, liver, and other organs and is known as graft-versus-host disease (GVHD). The donated cells must be HLA-matched to prevent GVHD. Typically, this complication will start after the stem cells have engrafted (about 2 weeks after the transplant).
Although some GVHD may not be harmful, if the stem cells continue to produce cells that attack tissue, the effect can be dramatic, with sloughing of skin, organ malfunction or failure, and eventual death.
Nursing considerations
The donor and the recipient should be prepared for the procedure with age-appropriate explanations. In addition, follow these steps:
Administer immunosuppressants, such as steroids and cyclosporine (Sandimmune), as ordered to control GVHD.
Monitor the child for signs of GVHD, such as changes in skin color or appearance, hematuria, diarrhea, jaundice, and a change in mental status (even after they leave the facility).
Because the child is at high risk for infection immediately after the transplantation, monitor closely for signs of infection.
Prevent skin breakdown by using pressure-relieving or pressurereducing beds or mattresses; turn the child frequently.
Support the child and his family throughout this stressful time because the child will be critically ill with the potential for lifethreatening complications.
|
Hematologic and immunologic disorders
Hematologic and immunologic disorders that may affect children include acquired immunodeficiency syndrome (AIDS), allergic rhinitis, aplastic anemia, atopic dermatitis, hemophilia, Hodgkin’s disease, iron deficiency anemia, leukemia, sickle cell anemia, SLE, and thalassemia.
HIV/AIDS
The identification of the human immunodeficiency virus (HIV) in the 1980s foreshadowed a worldwide epidemic that crosses all ethnic, cultural, and age barriers. Although the initial cases were primarily among gay men, the virus then expanded into all groups, including infants and children.
What causes it
HIV, a retrovirus, has the ability to enter a cell and incorporate itself into the cell’s ribonucleic acid, essentially changing the genetic structure and causing the cell to slowly die.
A stranger in friend’s clothing
Because HIV becomes part of the cell, the body’s normal defense mechanisms (from the immune system) don’t recognize it as foreign, and the virus goes unchallenged.
Out of control
From the first single cell, the virus replicates and then enters other cells, eventually infecting several cells and rendering them nonfunctional. When a large number of cells become infected, the normal ability to control common organisms is compromised, and the person develops AIDS.
|
How it happens
Transmission of HIV occurs by contact with infected blood or body fluids and is associated with identifiable, high-risk behaviors, including sexual intercourse with multiple partners, I.V. drug use, and pregnancies in HIV-infected women.
It’s different for kids
The mode of transmission in children has always been different from that in adults. Although transmission in adolescents may occur from sexual contact or I.V. drug use, these issues aren’t common factors in transmission to the younger child. Potential sources of infection in children include:
being born to an untreated, infected mother
breast-feeding from an infected mother
blood transfusions with HIV-tainted blood products (hemophiliacs with contaminated factor VIII or other factor products that were pooled from multiple donors before blood donations were routinely screened).
Destructive domino effect
HIV has a particular affinity for the CD4+ helper T cell as well as monocytes and macrophages. The virus invades these cells and renders them nonfunctional, resulting in suppressed cell-mediated and humoral immunity. The degree of immunosuppression will progress and, eventually, result in opportunistic infection and even death.
Diagnosing HIV/AIDS
HIV was historically suspected when a person developed an indicator disease listed in the following chart and a CD4+ count was monitored and the antibody was detected. The current method for diagnosing a person as being HIV positive is to detect the virus itself and look at the “viral load” to determine the extent of the infection. This allows for quicker diagnosis because the body takes time to develop an antibody. A person now is considered to have AIDS if the CD4+ lymphocyte count is below 200.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access