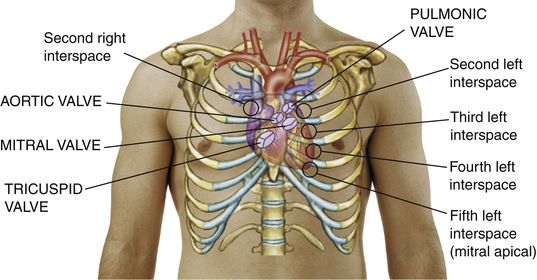
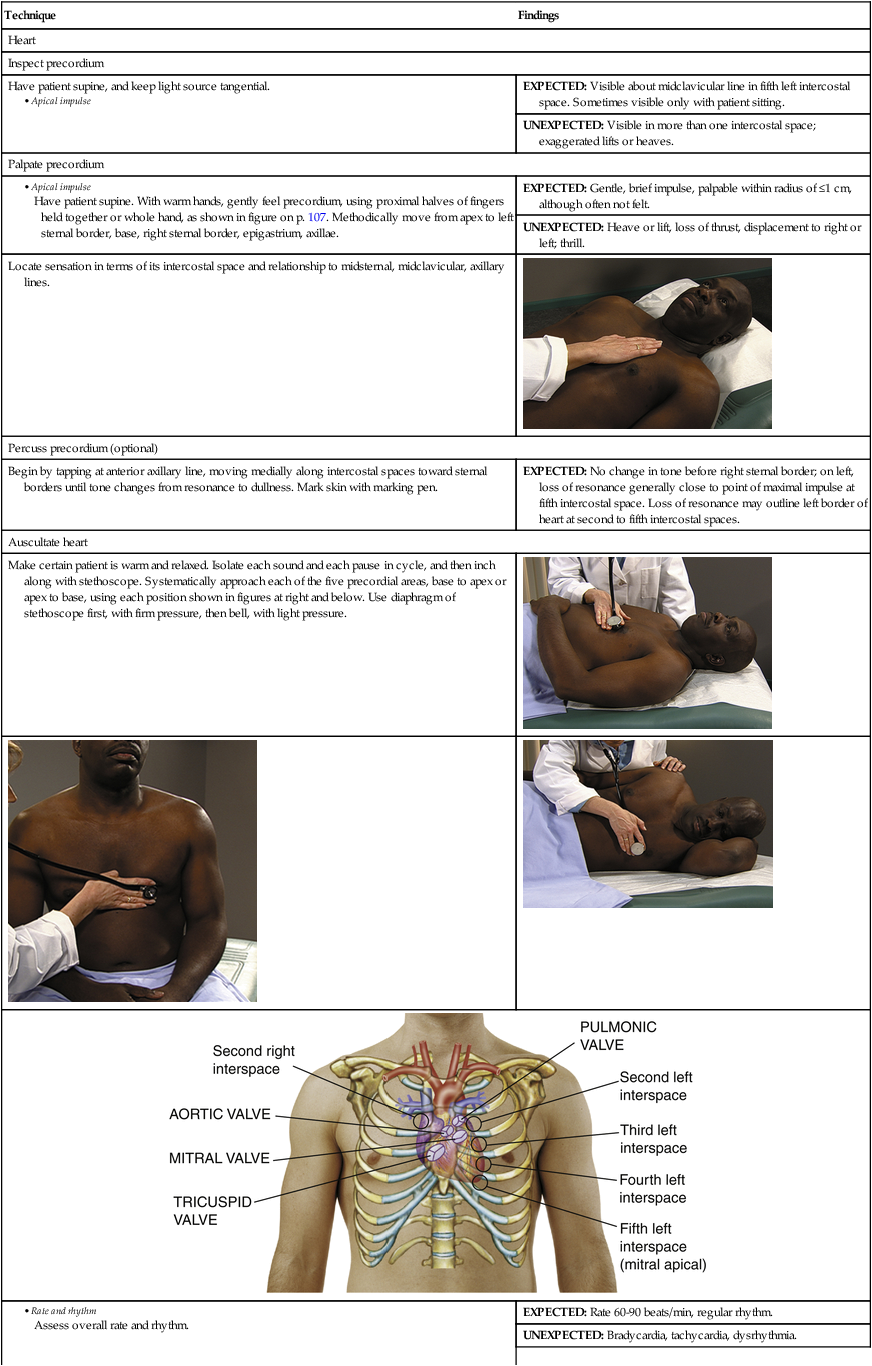
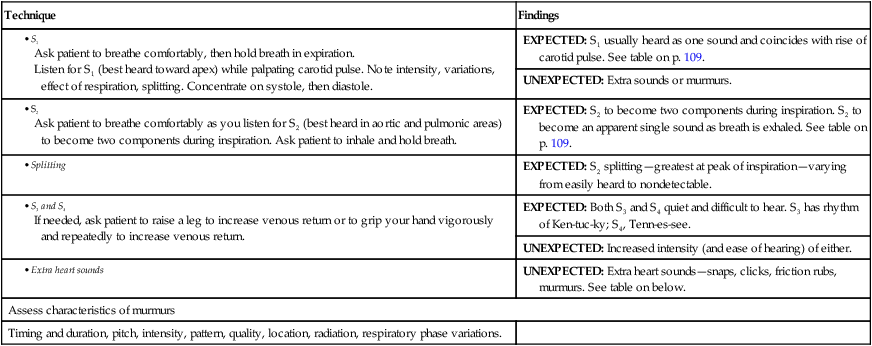
Have patient supine. With warm hands, gently feel precordium, using proximal halves of fingers held together or whole hand, as shown in figure on p. 107. Methodically move from apex to left sternal border, base, right sternal border, epigastrium, axillae. Heart Sounds According to Auscultatory Area
Heart
Examination
Technique
Findings
Heart
Inspect precordium
Have patient supine, and keep light source tangential.
EXPECTED: Visible about midclavicular line in fifth left intercostal space. Sometimes visible only with patient sitting.
UNEXPECTED: Visible in more than one intercostal space; exaggerated lifts or heaves.
Palpate precordium
EXPECTED: Gentle, brief impulse, palpable within radius of ≤1 cm, although often not felt.
UNEXPECTED: Heave or lift, loss of thrust, displacement to right or left; thrill.
Locate sensation in terms of its intercostal space and relationship to midsternal, midclavicular, axillary lines.

Percuss precordium (optional)
Begin by tapping at anterior axillary line, moving medially along intercostal spaces toward sternal borders until tone changes from resonance to dullness. Mark skin with marking pen.
EXPECTED: No change in tone before right sternal border; on left, loss of resonance generally close to point of maximal impulse at fifth intercostal space. Loss of resonance may outline left border of heart at second to fifth intercostal spaces.
Auscultate heart
Make certain patient is warm and relaxed. Isolate each sound and each pause in cycle, and then inch along with stethoscope. Systematically approach each of the five precordial areas, base to apex or apex to base, using each position shown in figures at right and below. Use diaphragm of stethoscope first, with firm pressure, then bell, with light pressure.



EXPECTED: Rate 60-90 beats/min, regular rhythm.
UNEXPECTED: Bradycardia, tachycardia, dysrhythmia.
EXPECTED: S1 usually heard as one sound and coincides with rise of carotid pulse. See table on p. 109.
UNEXPECTED: Extra sounds or murmurs.
EXPECTED: S2 to become two components during inspiration. S2 to become an apparent single sound as breath is exhaled. See table on p. 109.
EXPECTED: S2 splitting—greatest at peak of inspiration—varying from easily heard to nondetectable.
EXPECTED: Both S3 and S4 quiet and difficult to hear. S3 has rhythm of Ken-tuc-ky; S4, Tenn-es-see.
UNEXPECTED: Increased intensity (and ease of hearing) of either.
UNEXPECTED: Extra heart sounds—snaps, clicks, friction rubs, murmurs. See table on below.
Assess characteristics of murmurs
Timing and duration, pitch, intensity, pattern, quality, location, radiation, respiratory phase variations.
Aortic
Pulmonic
Second Pulmonic
Mitral
Tricuspid
Pitch
S1 < S2
S1 < S2
S1 < S2
S1 > S2
S1 = S2
Loudness
S1 < S2
S1 < S2
S1 < S2∗
S1 > S2†
S1 > S2
Duration
S1 < S2
S1 > S2
S1 < S2
S1 < S2
S1 = S2
S2 split
>Inhale
>Inhale
>Inhale
>Inhale‡
>Inhale
<Exhale
<Exhale
<Exhale
<Exhale
<Exhale
A2
Loudest
Loud
Decreased
P2
Decreased
Louder
Loudest
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Heart
Get Clinical Tree app for offline access
