Chapter 6 HEALTH PROMOTION AND EDUCATION
Owing to technological developments and medical and scientific achievements over the last century, the world’s population is generally living longer and healthier lives. However, major disparities in health still exist for some of the world’s population, with some countries still experiencing high morbidity and mortality rates. In recognition of these disparities in world health, the World Health Organization (WHO) began its work towards achieving health for all the world’s population. Health promotion and education provide the key to minimising or eliminating disparities in world health and play fundamental roles in achieving the goals and objectives as determined by WHO. By raising the level of health awareness and providing health education for both the individual and the community, nurses play a vital role in health promotion.
HEALTH
Health is generally understood to be an absence of disease or illness. The WHO defines health as ‘a state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity’ (WHO 1978). WHO’s definition of health is holistic in that it considers physical, psychological, cultural and social factors. According to WHO, ‘health depends on our ability to understand and manage the interaction between human activities and the physical and biological environment’ (WHO 1992: 409). Good health is a major resource for social, economic and personal development and an important dimension of quality of life. An understanding of what constitutes ‘good’ health may vary from one person to another. Political, economic, social, cultural, environmental, behavioural and biological variables can all have an impact on health. Health, then, may be defined according to circumstances, context and perceptions, and experiences, which may vary between individuals and between communities.
MAINTAINING HEALTH
Maintaining health requires achieving a balance of all aspects of life. Factors such as age, sex, family relationships, cultural influences and economic status may have an impact on achieving that balance. Several models have been developed to provide nurses with frameworks to assist people to achieve optimal health. The most common model was developed in the 1940s by Abraham Maslow. He believed that a person’s motivations and behaviour are formed by attempting to meet their basic needs. Maslow defined basic human needs as physiological needs, safety and security, love and belongingness, self-esteem and self-actualisation. Maslow’s ‘Hierarchy of Needs’ model (Figure 6.1) emphasises that some needs are more basic than others and that the more basic needs need to be met before consideration of higher needs. Nurses need to recognise each client’s individuality and own value system, which will impact on prioritisation of needs.
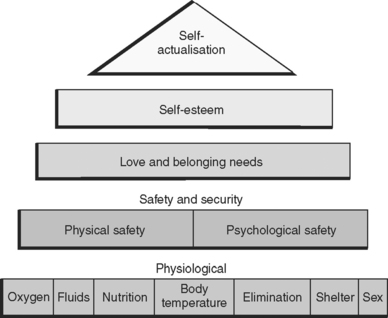
Figure 6.1 Maslow’s Hierarchy of Needs
(redrawn from Maslow AH (1970) Motivation and Personality. Prentice Hall, Upper Saddle River, New Jersey)
Many factors affect individual definitions of health. Definitions vary according to an individual’s previous experiences, expectations of self, age and sociocultural influences. A person’s definition of health influences behaviour related to health and illness. By understanding clients’ perceptions of health and illness, nurses can provide more meaningful assistance to help them gain or attain a state of health (Berman et al 2007).
COMMUNITY HEALTH
Community health occurs when there is a commitment by the community to work towards achieving the health and wellbeing of individuals, families and groups. This does not necessarily mean the community needs a vast number of medical services or an array of healthy lifestyle gurus and experts. Rather, healthy communities are those that feel empowered to shape their own destiny. They enjoy broad participation in health policies and in decisions that affect daily life; members of healthy communities are able to feel they have some control over the design and sustainability of the community’s current and future potential. In short, they feel a sense of commonality or cohesion with others, which becomes beneficial for all members of the community (Hertzman 2001).
EARLY RECOGNITION AND DETECTION OF DISEASE
Health care services recognise the need to focus on health rather than illness; therefore the emphasis is on health promotion and illness prevention at an individual and community level. Health promotion and illness prevention have become an important focus of health care for several reasons; for example, there are still no cures for many diseases, health care costs are rising rapidly, and the community is more aware of the value of health maintenance. Advancements in technology and scientific and medical achievements have led to the development of advanced diagnostic equipment. The early detection and recognition of the contributing factors that influence health and illness can prevent the spread of disease at both an individual and a community level. An example is the free breast-screening programs for women aged over 50 to detect tumours early and significantly reduce the need for radical surgery and improve recovery rates.
FACTORS INFLUENCING HEALTH AND ILLNESS
A person’s health status depends on many personal, social and environmental factors, including:
HEALTH PROMOTION
Health promotion is the process of enabling people to increase their control over, and to improve, their health. To reach a state of complete physical, mental and social wellbeing an individual or group must be able to identify and realise aspirations, satisfy needs and change or cope with the environment. Health is therefore seen as a resource of everyday life, not the objective of living. Health is a positive concept emphasising social and personal resources as well as physical capacities. Therefore, health promotion is not just the responsibility of the health sector but goes beyond healthy lifestyles to wellbeing (WHO 1986). As opposed to illness prevention activities, which aim to protect the client from actual or potential threats to health, health promotion aims to help people maintain their present level of health or increase control over, and improve, their health.
The concepts of health promotion and illness prevention are closely related (Clinical Interest Box 6.1). Nurses focus on health promotion and illness prevention when providing health care, which assists clients to maintain good health and improve health, as well as providing care after illness has occurred. Health promotion activities can be passive or active. Active health promotion activities require the client to be motivated to adopt a specific health program such as giving up smoking. Passive health promotion occurs when the client benefits from the activities of others without necessarily acting themselves, such as in the fluoridation of drinking water.
A dynamic improvement in health and life expectancy has occurred in the last century in line with significant advances in technology. However, major disparities and inequalities in access to, and equity in, better health is recognised for different world populations. The WHO was set up in 1948 to deal with international health matters and concerns and is comprised of 192 countries. This worldwide organisation agreed that ‘Governments have a responsibility for the health of their peoples, which can be fulfilled only by the provision of adequate health and social measures’ (WHO 1992). The Declaration of Alma-Ata (health for all by the year 2000) came about after the 1978 WHO conference. This was to be the milestone for world health. The declaration called for:
These principles from the Declaration of Alma-Ata provide the underpinning concepts for ‘Primary Health Care’. Primary Health Care is essential care based on practical, scientifically sound and socially acceptable methods and technology, made universally accessible to people and families in the community through their full participation and at a cost that the community and country can afford to maintain at every stage of their development, in the spirit of self-reliance and self-determination (WHO 1978).
Primary Health Care focuses on social justice, equity, community participation, socially acceptable and affordable technology, the provision of services on the basis of the needs of the population, health education and work to improve the root causes of ill-health. It emphasises working with people to enable them to make decisions about their needs and how best to address them. These guiding principles of Primary Health Care should be applied throughout the health system and adopted by all health workers (Wass 2000).
To distinguish between other often misconstrued concepts of Primary Health Care, and to understand exactly what Primary Health Care is, Wass (2000) provides an explanation of what Primary Health Care is not:
MODELS OF HEALTH PROMOTION
Various models of health promotion have been developed by nurses to provide conceptual frameworks for identifying a client’s health behaviour and beliefs. A client’s health beliefs may stem from many factors, including health perception, demographics and personality type. Tannahill’s model, for example, shows health promotion as being made up of three areas: prevention, health protection and health education (Downie et al 1996). Beattie’s model (1991), which is useful for charting ethical and political tensions, can be used as a planning tool. This model has four approaches to health promotion: health persuasion, personal counselling, community development and legislative action for health.
The Health–Illness Continuum Model
This model describes the relationship between health and illness and provides a method of identifying a client’s level of health (see Chapter 8). This model is valuable when comparing a client’s present health status with their previous level of health and for then setting nursing goals and objectives to promote a future level of health (Crisp & Taylor 2005).
The Health Belief Model
The health belief model (see Chapter 8) is one of the most widely used conceptual health promotion models and was developed to assist in understanding health behaviour. This model can be effective in developing health education strategies and can also be a useful framework for designing change strategies.
PREREQUISITES FOR HEALTH
The fundamental conditions and resources for health are peace, shelter, education, food, income, a stable ecosystem, sustainable resources, social justice and equity. To work effectively, improving health requires a secure foundation in these basic prerequisites. The Ottawa Charter for Health Promotion (Clinical Interest Box 6.2) highlights the need for health workers to be effective in advocacy, enabling and mediation to enable people to gain greater control over their lives (WHO 1986).
CLINICAL INTEREST BOX 6.2 The Ottawa Charter for Health Promotion
The charter states that actions to promote health require:
ENABLING
Health promotion focuses on achieving equity in health. Health promotion action aims at reducing differences in current health. The charter states that ‘People cannot achieve their fullest health potential unless they are able to take control of those things which determine their health. This must apply equally to women and men’ (WHO 1986).
MEDIATION
Australian Government policy on health activity began in the mid 1980s. In 1986 the Better Health Commission formulated Australia’s response to the goal of Health for All by 2000. The Health for all Australians report represents the beginning of Australia’s commitment to health goals and targets, carried through in several subsequent documents, including Health Goals and Targets for Australian Children and Youth (Child, Adolescent and Family Health Service 1992), Goals and Targets for Australia’s Health in the Year 2000 and Beyond (Nutbeam et al 1993) and Better Health Outcomes for Australians (Commonwealth Department of Human Services and Health 1994).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


