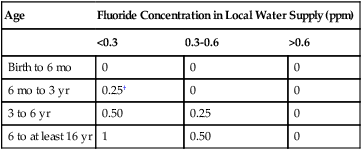
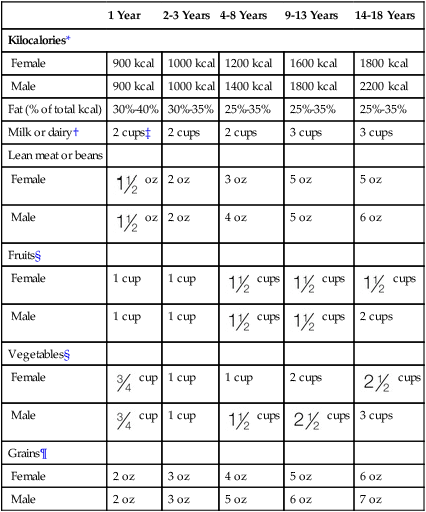
Symbol http://evolve.elsevier.com/Wong/clinical Patient and Family Education — Spanish Translations • Infant Cardiopulmonary Resuscitation for the Layperson (Resucitación Cardiopulmonar de Infantes para el Público General) • Child Cardiopulmonary Resuscitation for the Layperson (Resucitación Cardiopulmonar de Niños para el Público en General) Patient and Family Teaching Guides • Administering digoxin at home • Applying a topical anesthetic • Caring for a central venous catheter • Caring for an implanted port • Caring for an intermittent infusion device • Caring for the child in a cast • Caring for the child with a colostomy • Caring for the child with a tracheostomy • Caring for the choking child • Caring for the choking infant • Caring for your child’s teeth • Child cardiopulmonary resuscitation for the layperson • Giving aerosolized medications (nebulizer treatments) • Giving intramuscular (IM) injections • Giving medications to children • Giving nasogastric tube feedings • Giving rectal medications—suppositories • Giving subcutaneous (Sub Q) injections • Infant cardiopulmonary resuscitation for the layperson • Interpreting peak expiratory flow rates • Measuring oxygen saturation with pulse oximetry • Measuring your child’s temperature • Minimizing pain of blood glucose monitoring • Monitoring peak expiratory flow • Performing clean intermittent bladder catheterization • Preventing spread of HIV and hepatitis B virus infections • Safe disposal of needles and lancets • Suctioning the nose and mouth The Institute of Medicine (IOM) has developed guidelines for nutritional intake that encompass the Recommended Dietary Allowances (RDAs) yet extend their scope to include additional parameters related to nutritional intake. The Dietary Reference Intakes (DRIs)* are composed of four categories. These include estimated average requirements (EARs) for age and gender categories, tolerable upper-limit (UL) nutrient intakes that are associated with a low risk of adverse effects, adequate intakes (AIs) of nutrients, and new standard RDAs. The new guidelines present information about lifestyle factors that may affect nutrient function, such as caffeine intake and exercise, and about how the nutrient may be related to chronic disease (Table 2-1). TABLE 2-1 Dietary Reference Intakes (DRIs) See also Unit 1 for select DRI values. *Women of childbearing age and with expectation of becoming pregnant should consume 400 mcg/d from supplements or fortified foods, or both, in addition to intake of folate from a varied diet. Portions adapted from Dietary Reference Intakes (DRIs): Food and Nutrition Board, Institute of Medicine, National Academy of Sciences, 2004. Available at www.nap.edu; and Dietary Reference Intakes: An Update, International Food Information Council Foundation, 2005. Available at http://ific.org. The American Heart Association dietary guidelines (Table 2-2) may also be used to encourage healthy dietary intakes designed to decrease obesity and cardiovascular risk factors and subsequent cardiovascular disease, which is now known to occur in young children as well as adults. For more information on healthy dietary habits and child nutrition, visit the American Heart Association website, available at http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/Dietary-Recommendations-for-Healthy-Children_UCM_303886_Article.jsp. TABLE 2-2 *For children age 2 years and older. Nutrient and energy contributions from each group are calculated according to the nutrient-dense forms of food in each group (e.g., lean meats and fat-free milk). †Milk listed is fat-free except for children younger than age 2 years. If 1%, 2%, or whole-fat milk is substituted, this will use, for each cup, 19, 39, or 63 kcal, respectively, of discretionary calories and add 2.6, 5.1, or 9 g, respectively of fat, of which 1.3, 2.6, or 4.6 g, respectively are saturated fat. ‡For 1-year-old children, calculations are based on 2%-fat milk. If 2 cups of whole milk are substituted, 48 kcal of discretionary calories will be used. The American Academy of Pediatrics recommends that low-fat or reduced-fat milk not be started before age 2 years. §Serving sizes are ¶Half of all grains should be whole grains. Data from American Heart Association. Available at www.americanheart.org/presenter.jhtml?identifier53033999; and American Heart Association, Giddings SS, Dennison BA, and others: Dietary recommendations for children and adolescents: A guide for practitioners, Pediatrics 117(2):544-559, 2006. Reprinted with permission www.heart.org. Copyright 2011 American Heart Association, Inc. In 2011 the United States Department of Agriculture replaced the Food Guide Pyramid (MyPyramid) with MyPlate (http://www.choosemyplate.gov/) (Figure 2-1). This colorful plate shows the 5 main food groups—fruits, grains, vegetables, protein, and dairy—with the intended purpose to involve children and their families in making appropriate food choices for meals and decrease the incidence of overweight and obesity in the United States. MyPlate provides an online interactive feature that allows the individual to select (click on) an individual food group and see choices for foods in that group. Approximate serving sizes are suggested and vegetarian substitutions are also provided.
Health Promotion
 indicates material that may be photocopied and distributed to families.
indicates material that may be photocopied and distributed to families.
![]()
Nutrition
Dietary Reference Intakes
DRI Populations and Life Stage Groups
Recommended Dietary Allowance (RDA)
Estimated Average Requirements (EARS)
Adequate Intake (AI)
Tolerable Upper Intake Level (UL)
Average daily dietary intake level sufficient to meet the nutrient requirement of most healthy individuals in a given life stage or gender group. May be used to evaluate nutrient intake of a given population (e.g., vegetarian).
Daily nutrient intake value estimated to meet the requirement of half the healthy persons in a given life stage or gender group (used to assess dietary adequacy and is the basis for RDAs).
Recommended intake value based on observed or experimentally determined approximations of nutrient intake by a group of healthy persons, which are assumed to be adequate when an RDA cannot be determined. In healthy breastfed infants (0-6 mo), AI is the mean intake.
Highest level of daily nutrient intake likely to pose no risk of adverse effects for most individuals in the general population. Risk increases as intake above the UL increases. May be used to set limits on nutrient supplementation, especially for vitamins and minerals that could be harmful.
Clinical Applications
Folate
600 mcg/d
520 mcg/d
400 mcg/d*
1000 mcg/d
Iron
10 mg/d
4.1 mg/d
10 mg/d
40 mg/d
Vitamin C
65 mg/d
56 mg/d
65 mg/d
1800 mg/d
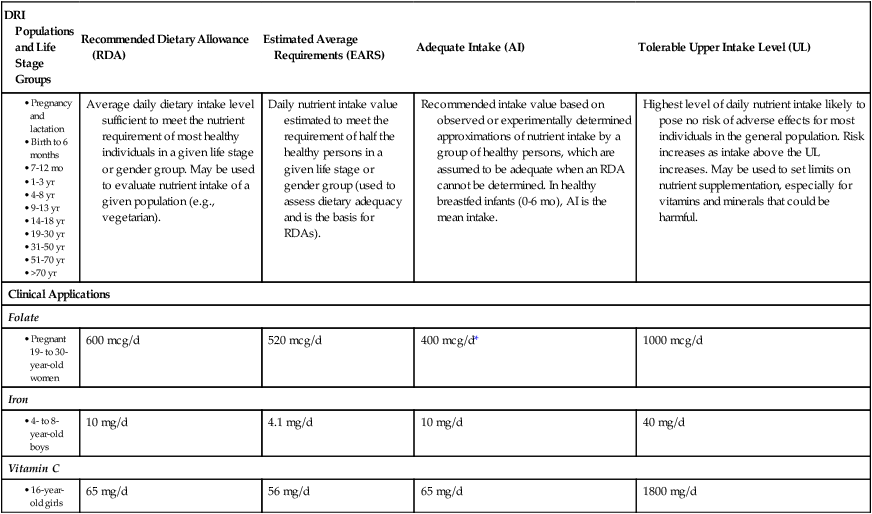
Dietary Guidelines for Children (American Heart Association)
1 Year
2-3 Years
4-8 Years
9-13 Years
14-18 Years
Kilocalories*
Female
900 kcal
1000 kcal
1200 kcal
1600 kcal
1800 kcal
Male
900 kcal
1000 kcal
1400 kcal
1800 kcal
2200 kcal
Fat (% of total kcal)
30%-40%
30%-35%
25%-35%
25%-35%
25%-35%
Milk or dairy†
2 cups‡
2 cups
2 cups
3 cups
3 cups
Lean meat or beans
Female
 oz
oz
2 oz
3 oz
5 oz
5 oz
Male
 oz
oz
2 oz
4 oz
5 oz
6 oz
Fruits§
Female
1 cup
1 cup
 cups
cups
 cups
cups
 cups
cups
Male
1 cup
1 cup
 cups
cups
 cups
cups
2 cups
Vegetables§
Female
 cup
cup
1 cup
1 cup
2 cups
 cups
cups
Male
 cup
cup
1 cup
 cups
cups
 cups
cups
3 cups
Grains¶
Female
2 oz
3 oz
4 oz
5 oz
6 oz
Male
2 oz
3 oz
5 oz
6 oz
7 oz
 cup for age 1 year,
cup for age 1 year,  cup for ages 2 to 3 years, and
cup for ages 2 to 3 years, and  cup for age 4 years and older. A variety of vegetables should be selected from each subgroup over the week.
cup for age 4 years and older. A variety of vegetables should be selected from each subgroup over the week.
MyPlate for Kids
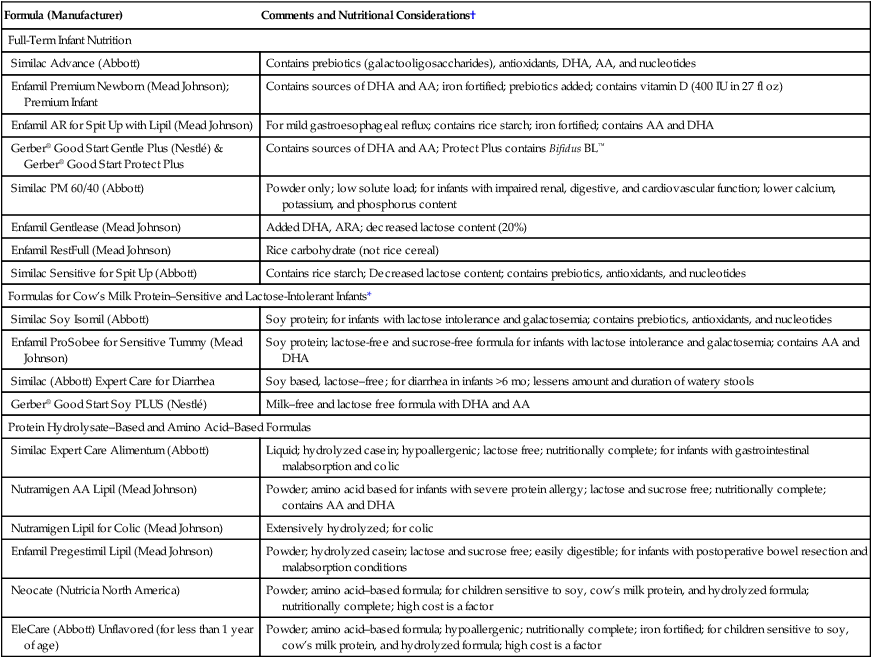
Normal and Special Infant and Child Formulas*
Formula (Manufacturer)
Comments and Nutritional Considerations†
Full-Term Infant Nutrition
Similac Advance (Abbott)
Contains prebiotics (galactooligosaccharides), antioxidants, DHA, AA, and nucleotides
Enfamil Premium Newborn (Mead Johnson); Premium Infant
Contains sources of DHA and AA; iron fortified; prebiotics added; contains vitamin D (400 IU in 27 fl oz)
Enfamil AR for Spit Up with Lipil (Mead Johnson)
For mild gastroesophageal reflux; contains rice starch; iron fortified; contains AA and DHA
Gerber® Good Start Gentle Plus (Nestlé) & Gerber® Good Start Protect Plus
Contains sources of DHA and AA; Protect Plus contains Bifidus BL™
Similac PM 60/40 (Abbott)
Powder only; low solute load; for infants with impaired renal, digestive, and cardiovascular function; lower calcium, potassium, and phosphorus content
Enfamil Gentlease (Mead Johnson)
Added DHA, ARA; decreased lactose content (20%)
Enfamil RestFull (Mead Johnson)
Rice carbohydrate (not rice cereal)
Similac Sensitive for Spit Up (Abbott)
Contains rice starch; Decreased lactose content; contains prebiotics, antioxidants, and nucleotides
Formulas for Cow’s Milk Protein–Sensitive and Lactose-Intolerant Infants*
Similac Soy Isomil (Abbott)
Soy protein; for infants with lactose intolerance and galactosemia; contains prebiotics, antioxidants, and nucleotides
Enfamil ProSobee for Sensitive Tummy (Mead Johnson)
Soy protein; lactose-free and sucrose-free formula for infants with lactose intolerance and galactosemia; contains AA and DHA
Similac (Abbott) Expert Care for Diarrhea
Soy based, lactose–free; for diarrhea in infants >6 mo; lessens amount and duration of watery stools
Gerber® Good Start Soy PLUS (Nestlé)
Milk–free and lactose free formula with DHA and AA
Protein Hydrolysate–Based and Amino Acid–Based Formulas
Similac Expert Care Alimentum (Abbott)
Liquid; hydrolyzed casein; hypoallergenic; lactose free; nutritionally complete; for infants with gastrointestinal malabsorption and colic
Nutramigen AA Lipil (Mead Johnson)
Powder; amino acid based for infants with severe protein allergy; lactose and sucrose free; nutritionally complete; contains AA and DHA
Nutramigen Lipil for Colic (Mead Johnson)
Extensively hydrolyzed; for colic
Enfamil Pregestimil Lipil (Mead Johnson)
Powder; hydrolyzed casein; lactose and sucrose free; easily digestible; for infants with postoperative bowel resection and malabsorption conditions
Neocate (Nutricia North America)
Powder; amino acid–based formula; for children sensitive to soy, cow’s milk protein, and hydrolyzed formula; nutritionally complete; high cost is a factor
EleCare (Abbott) Unflavored (for less than 1 year of age)
Powder; amino acid–based formula; hypoallergenic; nutritionally complete; iron fortified; for children sensitive to soy, cow’s milk protein, and hydrolyzed formula; high cost is a factor
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Health Promotion
Get Clinical Tree app for offline access