Outline care plan, including interventions and recommendations.
Allow electronic access by CC, PCP, and/or other specialists.
Provide printable format for care conferences and appointments.
Facilitate patient understanding (at appropriate health literacy level).
Include lists of diagnoses, medications, reminders for upcoming appointments, and preventative care recommendations.
Track admission and discharge dates.
Supply structured protocol for post-hospitalization and post-ED follow-up.
Structured overview of patient health information
The system should provide access to fundamental patient information, such as demographics, diagnoses, medications, assessment, and lab results. Gathering all of this data into one system in a structured, logical interface is critical to efficient access by the care coordinator and medical team. This feature should also include a recorded care plan for the patient’s ongoing interventions and assessments, including recommendations, goals set by the patient and provider, and upcoming appointments or other tests.
Patient summary sheet
A printable, patient-friendly version of the clinical summary at the appropriate health literacy level gives the care team a tool for discussing health issues with the patient. A Patient Summary Sheet outlines when a patient should receive appropriate treatment or monitoring, required lab work, and medications; it contains a problem list, structured medications list, and patient-specific goals and assessments. This record may be given to the patient and family as a printed clinical summary or sent electronically, or both. It provides a valuable self-management tool for the patient to reference for reminders of health promotion activities and preventative care actions such as immunizations, mammograms, prostate exams, nutrition, diet, or exercise classes.
Figure 7.1 A Patient Summary Sheet
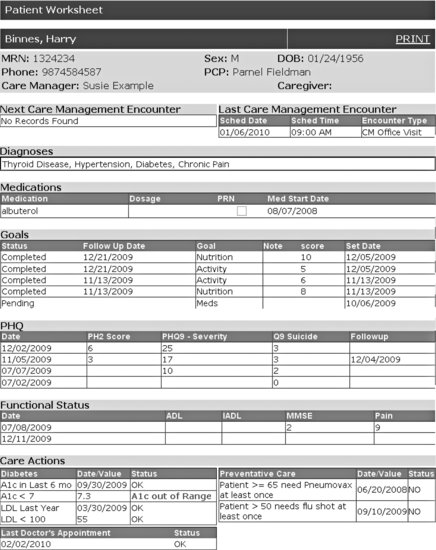
The patient summary sheet provides a solid foundation for behavioral modification, disease- or medication-specific education, and motivational health coaching with the patient, as well as a starting point for effective pre-visit planning in team-based care. Since the amount of information to be reviewed with patients with complex conditions can often be extensive, a patient summary sheet can facilitate discussion of quality metrics, preventive needs, and care planning. In one study, voluntary use of this summary sheet by clinical teams improved process and outcome quality measures by 17% to 30% (Wilcox et al. 2005). HIT self-management tools support health improvement goals when embedded in models of patient-centered care that motivate and facilitate their use (Dorr et al. 2006b; Dorr et al. 2007a); without such models, there is little evidence that clinics can achieve improved outcomes.
Care setting transitions
Clinical summaries are valuable for patient care transitions to another provider or an ED or hospital setting. An electronic or printed summary should be sent with the patient to provide the other setting with the proper background to properly treat the patient and contact information to report results or outcomes back to the primary care coordination team.
In some situations, electronic referrals for specialist consultation may be adequate to answer a patient’s or primary care provider’s questions. A specialist can sometimes make a recommendation or diagnosis based on descriptions, diagnostic images, and lab results provided via the HIT system. This process improves the efficiency and timeliness of care for all involved (O’Malley et al. 2009). Technical specifications, such as the Continuity of Care Record standard, facilitate electronic sharing of information, which supports the reconciliation and continuation of care plans and adherence to patient preferences.
Structured, flexible assessments & processes
A number of medical, psychosocial, and functional assessments provide the foundation for patient-centered care coordination. Protocols should provide structured but flexible guidance for clinical care (Dorr et al. 2006a).
Table 7.2 Overview of Features for Assessment and Protocol Process Support in an HIT System
| Areas of Implementation | IT Functions |
| Structured Encounter Form | Provide feedback about next steps and recommendations. Organize and prioritize information. Document communications and visits between any members of care team. Fulfill documentation criteria for records and billing. Serve as guideline for protocols. Track future appointments. |
| Medication Management | Support medication reconciliation at every encounter. Track encounters between CC and pharmacist. Provide printable comprehensive medication list. Identify and track barriers to medication adherence. Track prescription fills. |
| Assessments for Health, Psychosocial, and Functional Status | Support adherence to evidence-based guidelines. Furnish easy-to-fill forms with structured data entry. Update easily to document changes in patient status. Allow electronic access by CC, PCP, and/or other specialists. Provide printable format for flexible use. |
Structured encounter form
Given the vast variety of information that must be communicated to and from the patient and recorded during each interaction, a structured encounter form – available during face-to-face and phone encounters – is a core component of an IT system that supports care coordination. The advanced encounter form may function as a checklist for encounters by organizing and prioritizing communication that must be relayed and gathered during interactions between the patient and members of the care coordination team. Important components, such as primary language, preferences, or health literacy, may be tracked in such a way to allow future users to be immediately reminded of them in the next encounter. Advanced functions on the form might include the availability of reminders and feedback about next steps in the care plan, interface for scheduling the next encounter, or health promotion protocols. The form should also provide immediate decision support about the completeness of documentation, to aid in the workflow and ensure that documentation requirements are fulfilled for each encounter. High value activities, such as motivational interviewing, education, goal-setting, self-management support, and care conferences, should be tracked individually to see their contribution to the care and health of the person.
The HIT system should also facilitate tracking communication activities with other providers as necessary, either using a flexible encounter form or some other feature. Care conferences and other communication activities between the care coordinator and the primary care provider will be necessary to relay information regarding patient status, goals, and any modifications to protocols or care plans. The care coordinator should also track communications with other care team members, such as pharmacists, mental health providers, community resources, and patient’s family members or caregivers.
Medication management
Medication reconciliation and prescribing accuracy are critical to care safety. Having protocols to ensure that clinicians update medication lists with patients and caregivers, document medication discrepancies, and reconcile all relevant records helps reduce the likelihood of adverse events (Lesselroth et al. 2009). HIT systems can improve the process dramatically, from querying the patient about current adherence and starting reconciliation to gathering data about medication on-hand from prescription fill records.
Patients with five or more chronic conditions fill nearly 50 prescriptions per year on average (Anderson & Horvath 2002). The HIT system must have the functionality to create and print a comprehensive medication list to ensure that the medication list is accurate and updated regularly. The printable feature allows the medication list to be given to the patient to ensure accurate communication of medication purpose, dosage, and frequency. This medication list should be available to the care coordinator, primary care physician, specialists, hospitals, the patient, and the patient’s caregiver or family members (with patient’s permission). Transitions between different care settings can be greatly facilitated by ensuring that all parties are provided an accurate medication list. This list is also a tool for the care coordinator to help identify barriers to prescription refills and medication adherence. An advanced system should have the capability of tracking prescription refill dates and coordinate refill dates of all prescriptions to decrease multiple pickup dates and increase adherence. To this end, the system should also be able to track communication between the care coordinator and the pharmacist, whether in the medication information interface of in the encounter form. The advanced system will also be able to track medication reconciliation steps taken and adjustments made.
Assessments for health, psychosocial, and functional status
The HIT system should include built-in forms for assessment of patients’ medical, psychosocial, and other needs. Such assessments might include the Patient Health Questionnaire Depression Scale (PHQ9; a nine-item screen used to identify and rate depression severity), mini-mental status examination, or other cognitive evaluations, self-management and medical literacy evaluations, functional assessments such as activities of daily living or instrumental activities of daily living, and forms to record family pattern profile, caregiver contacts, and other social-support information. While data entry of responses should be structured, assessments should also provide a flexible field for extra patient-specific notes. These assessment results should be able to be tracked over time and accessible to all members of the care team. Where applicable, they should also include clinical decision support alerts to ensure that notable results are not overlooked.
Self-management support with follow-up
Care coordinators work with patients to increase their abilities to self-manage their conditions, resulting in healthier behaviors, better medical outcomes, and enhanced quality of life. Self-management skills empower patients to take more ownership of their care and set goals to keep them engaged in health maintenance activities. The benefits of improved self-management may persist beyond the time that the team is involved, accounting for better outcomes even years later.
Table 7.3 Examples of IT Functions to Support Self-Management Training and Follow-Up Activities
| Areas of Implementation | IT Functions |
| Goal-Setting | Facilitate interactive updates and modifications. Allow electronic access by CC, PCP, and/or other specialists. List recommended self-management activities. Track long-term and short-term goals. |
| Electronic Patient Access | Allow electronic access to clinical summary and goals. Facilitate updates and questions to and from patients. Remind patients about follow-up appointments, laboratory and other tests, and pending tasks. |
| Social and Educational Resources | Supply printable educational resources and other materials that can be shared with patients. Access availability and requirements of community and social support programs. Remind about available health promotion activities. |
Goal-setting support
Goal-setting is critical to motivation for health self-maintenance among older patients with multiple challenging illnesses. The IT system must be able to create and track in a structured way both short- and long-term goals. These goals could be related to patient self-management activities, behavior changes, or lifestyle adjustments. The system should provide an interactive goal-setting form that can be modified and updated as the patient’s priorities and needs change. The goal record should be accessible by all members of the care team, including the care coordinator, primary care physician, specialists, and pharmacists, social workers, or others, as needed. Ideally, the patient would have electronic access to this goal information, but at minimum, the goal list should be printable to promote patient self-management and enable sharing with caregivers and family members. The ability to share this goal-setting form promotes stronger communication among all members of the care team, enhancing the patient’s support system to help achieve these goals.
Electronic patient access
Enabling electronic patient access to the clinical summary will aid in self-management by facilitating reminders and updates to and from the patient. Such access may come in the form of a personal electronic health record populated through the clinic’s EHR. The patient interface should allow the patient to view diagnoses, medications, and reminders or updates about recommendation and future encounters. Electronic access to the static patient summary sheet or care plan is a solid starting point. Ideally, the access interface should be more interactive and dynamic, allowing for two-way messaging between the patient and care team members. For instance, it could permit patients to upload test results (such as glucose readings for diabetics) or update goal progress for ongoing clinical monitoring. The system could support a simple workflow for review and integration of patient-supplied data into the primary medical record.
Social and educational resources
The HIT system should provide reminders of and access to information regarding electronic or community-based patient social support and educational resources. This may include links to printable diagnosis fact sheets, contact information for local support groups, or other resources to support the patient’s self-management efforts. For example, integrating information about the availability and eligibility requirements of social support programs – such as discounted access to exercise facilities, support groups, or meals-on-wheels programs – into the system would help clinicians offer such services to appropriate patients. To enable such information access, the system must provide a flexible interface for recording local opportunities for easy reference by the care team. The system should record referrals and materials provided to the patient in the care plan, and provide reminders to the care coordinator to follow-up with the patient regarding their efficacy or helpfulness. Some self-management programs are now exclusively online and based on evidence of effectiveness from previous studies (Gremeaux & Coudeyre 2010). Integration of the monitoring and evaluation components of such programs would be an advanced addition to a system.
Prioritization
HIT tools enable providers to break the cycle of fragmented care by regularly identifying and high priority and neglected health care issues. Prioritization of care coordination services must take place on three scales: the clinic level, the panel level, and the individual patient level.
Table 7.4 Overview of Features to Support Prioritization Activities in an HIT System
| Areas of Implementation | IT Functions |
| Risk Stratification List | Support algorithm for selecting high-risk patients. Provide a consistent methods to identify and refer patients. Generate lists of patients by risk stratification measures, enrollment status, and diagnoses. |
| Patient-Focused Prioritization | Outline systematic process for working with patients to determine priorities. Document priorities, preferences, and goals. Furnish adjustable care plans that accommodate patient needs and preferences. |
Quality measure selection and improvement cycles
At the broadest level, the clinical team must first delineate priorities for the focus of the care coordination program. The clinic’s priorities are embodied in the selection of quality measures, a set of criteria that aide in quantifying improvement of clinical foci through the care coordination program. These choices, along with updated clinical processes and outcomes measures, can be documented and tracked in the HIT system to evaluate longitudinal improvement. Interactive quality measure reports, a population management tool discussed in more detail below, support and reinforce this continuous quality improvement process. Clinical team members should be involved early on in the prioritization of quality improvement areas and measures, as their engagement in and commitment to the quality improvement process is requisite for success. Over time, clinical teams may undertake Plan-Do-Study-Act quality improvement cycles to better their performance on these metrics (Institute for Healthcare Improvement 2010).
Risk stratification list
At the patient population level, prioritization is manifest in risk stratification lists that are based on the quality measures chosen at the clinic level. Assessments of risk level can be done organically in provider meetings with patients or more systematically using a risk stratification algorithm – or, ideally, using a combination of both approaches to address a variety of clinic and patient needs. Using patient records and billing data, HIT systems can use predictive algorithms to establish and maintain a list of patients with great potential to benefit from the care coordination program. Such risk determination can be developed from one or a combination of patient factors, including but not limited to: number and severity of chronic conditions, past hospitalizations, past emergency department utilization, concerning assessment or lab results, family history of certain conditions, or total cost of the patient to the health care system. Based on quality improvement goals, risk stratification helps to select patients to receive focused interventions in the care coordination program and patients to call in first for proactive care improvement. HIT systems should be able to track all assignment methods and planned next steps. The system should also have the capacity to track enrollment status in the care coordination program and the date and source of referrals.
Patient-focused prioritization
Depending on the nature of the program implemented, a care coordinator may provide care for anywhere from 50 to 350 patients. Not only must the care coordinator determine which patients to focus on for interventions, but the coordinator must also determine which issues to focus on first for each patient. The care coordinator must spend time working with the patient (and the patient’s family, or caregivers, when applicable) to design and implement a prioritized care plan that focuses on improvement in clinical quality measures and in areas most important to the patient. Developing a care plan involves basic prioritization of health issues, ongoing concerns, and goals, as well as preventative care recommendations and lifestyle changes. This process and resulting care actions can help improve underlying conditions, solidify self-management skills, and enhance overall quality of life for the patient. HIT features to facilitate this process include focused patient protocols, which provide guidance for diagnosis-specific care priorities, and structured forms for establishing and tracking patient goals and preferences. The ability to track the responses to questions such as What is your biggest concern about your health? or What is your most important goal for your health? is a crucial function of these systems.
Population management
Health Information Technology tools empower the care team to better monitor the statuses and needs of an entire patient population. With so many patients to manage, the ability to identify, categorize, and track tasks and recommended interventions is critical to the care coordinator’s daily work flow. Thorough documentation in care plans ensures that all members of the clinical team are current on the patient’s status and ensures the accuracy of quality measure reports.
Table 7.5 HIT Functions That Support Population Management Activities
| Areas of Implementation | IT Functions |
| Quality Reports | Track quality measures from evidence-based guidelines. Produce specific reports by patient population, provider, care team, and clinic. |
| Care Coordinator Task Tracking | Identify gaps in completion of tasks. Document frequency, duration, mode and outcome of contacts. |
| Generic Care Plans and Protocols | List specific activities, tasks, goals, and progress on each. Generate templates for different diagnoses. Remind about pre-planned frequency of encounters. Be electronically accessible to CC, PCP, and/or other specialists. |
Registries and quality reports
Quality reports are a primary output of advanced HIT systems. As implemented, few EHRs provide quality reports without additional modules and technical support. The creation of population registries is one technique that enables quality reporting from an ambulatory-based HIT. Registries extract data from EHRs and other HIT systems for use in quality reports. A registry reorganizes the data, abstracts it to the correct granularity, and creates a population snapshot that can be used to understand the current performance on a variety of quality measures. Common examples include aggregating all the billing diagnoses for diabetes to create a single list of patients with diabetes, capturing the most recent date and value for all patients with a particular lab test, or creating a list of each primary care provider’s patients.
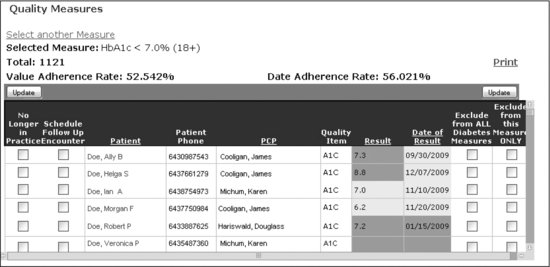
However, registries with static reports may not be adequate for ongoing care improvement initiatives. Interactive quality reports (Figure 7.2) allow members of the care team to easily and quickly generate outreach tasks for high-risk patients. The reports also aid clinicians in continuous and accurate evaluation of clinical quality improvement by allowing exclusions from a particular measure to respect patient preferences and acknowledge unique situations. This built-in flexibility supports the integrity of the quality measure reports for use in quality improvement cycles.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree