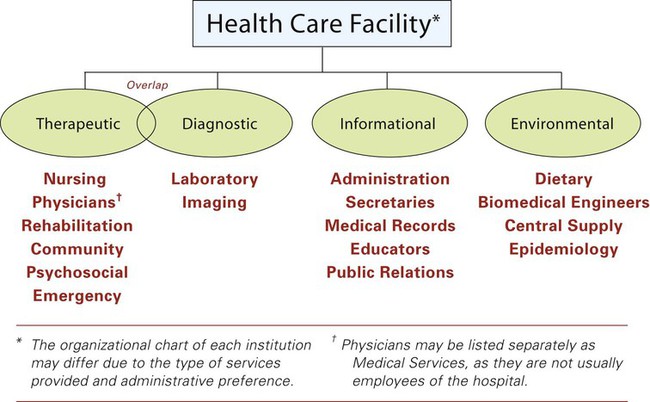
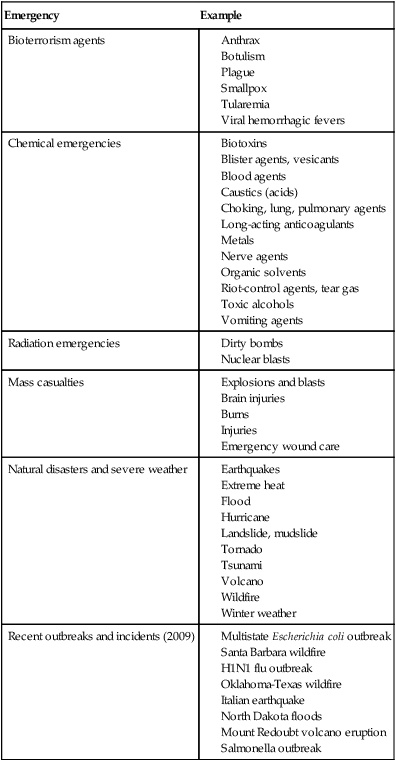
Chapter 1 In the earliest civilizations health needs were met by a specific person or group. Ancient treatments were harmful in some cases and helpful in others. Some of the most helpful were the use of herbs and plants for medication. The World Health Organization (WHO) estimates that 80% of the world’s population use plants or herbal treatments as part of their primary care. According to the American Association for the Advancement of Science (AAAS), about 118 of the 150 prescription drugs sold in the United States originate from plants, fungus, bacteria, and extractions from animals. Some of these remedies, such as quinine for malaria and digitalis for heart conditions, are still in use today (Box 1-1; also see Medical Milestones on pp. 21-22). Hippocrates (460-377 b.c.) is considered the father of modern medicine. He initiated the oath of practice that, in adapted form, most physicians still adopt (Box 1-2). In early times plagues or epidemics caused millions of deaths. Many of these diseases are now preventable through vaccination and improved methods of cleanliness and sanitation (Fig. 1-1). Although communicable diseases still cause many deaths in less-developed countries, new technological advances are being used to provide better health care throughout the world. Society has traditionally accorded respect to health care providers. The ancient Egyptians, Greeks, and Chinese who practiced the art of surgery or were witch doctors or neighborly herbalists all enjoyed stature in their communities. The arts of the past have become the professions of today (Box 1-3). These health care professions have many educational and training requirements. In the United States the focus of health care has shifted from the prevention of contagious diseases to those such as cancer, drug abuse, and heart disease, that are the result of lifestyles. Additionally, concerns relating to emergency response and preparedness services have become of primary concern to the health care industry (Table 1-1). Some communicable diseases are still a focus, including acquired immunodeficiency syndrome (AIDS), tuberculosis (TB), and flu. The WHO reported 33 million people living with AIDS worldwide in 2007. At the end of 2006, the Centers for Disease Control and Prevention (CDC) estimated that 1.1 million people were living with human immunodeficiency virus (HIV) or AIDS in the United States. It also reported a total of 12,898 cases of TB in 2008, which shows a decline of 2.9% from 2007 and 54% from 1980. According to WHO, nine Asian countries reported outbreaks of the H5N1 avian flu in birds by February 2006, six of which reported cases affecting humans. More than half of the confirmed cases were fatal. An outbreak of H1N1 swine flu was detected in April 2009. By July 2009 the CDC reported 43,771 cases; 302 of these patients died. The government has allocated money and the CDC has established preparation guidelines for a possible flu pandemic. Table 1-2 provides an overview of the pandemics and pandemic scares. TABLE 1-1 CDC Categories of Emergency Preparedness and Response From Centers for Disease Control and Prevention (CDC), retrieved September 2009, from http://www.bt.cdc.gov, Centers for Disease Control. TABLE 1-2 Institutional health care is provided by general hospitals, convalescent care centers, health maintenance organizations, home health agencies, and public health agencies (Table 1-3). Voluntary organizations provide education and support to individuals with specific concerns. The organizational structure of the facility defines the role of the health care worker (Fig. 1-2). TABLE 1-3 The federal agency that oversees the nation’s health care is the Public Health Services, which is part of the Department of Health and Human Services. It was established in 1798 to provide care for the American merchant seamen but has expanded to cover many other facets of health care (Box 1-4). The Department of Labor also regulates some health concerns through the Occupational Safety and Health Administration. The traditional model of insurance (fee-for-service) may also include cost-containment measures similar to those of managed care. The insured person may choose a plan that provides a percentage of the cost or a specified amount (Table 1-4). TABLE 1-4 Sample Insurance Cost Comparison
Health Care of the Past, Present, and Future
 Define at least 10 words relating to health care of the past, present, and future.
Define at least 10 words relating to health care of the past, present, and future.
 Identify three socioeconomic factors that influence the health care industry.
Identify three socioeconomic factors that influence the health care industry.
 Describe at least three advantages to following a career in the health care field.
Describe at least three advantages to following a career in the health care field.
 Describe a career ladder for at least one health care occupation.
Describe a career ladder for at least one health care occupation.
 List at least three factors to be considered when choosing an occupation.
List at least three factors to be considered when choosing an occupation.
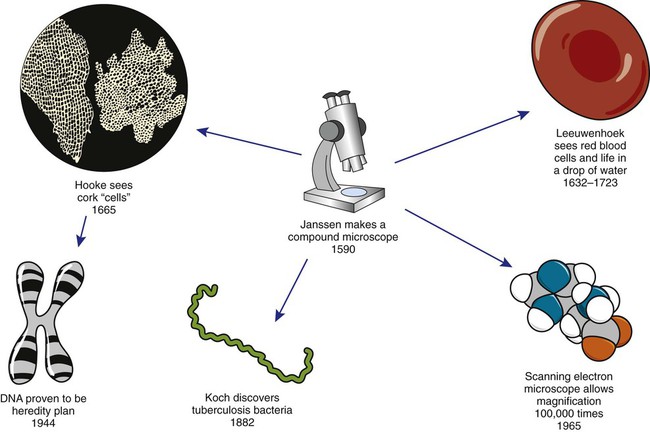
 Identify at least five milestones in the advancement of health care.
Identify at least five milestones in the advancement of health care.
 Describe at least two factors that have contributed to the rising cost of health care.
Describe at least two factors that have contributed to the rising cost of health care.
 Describe at least two methods being used to reduce health care costs.
Describe at least two methods being used to reduce health care costs.
Health Care of the Past
Health Care of the Present
Emergency
Example
Bioterrorism agents
Chemical emergencies
Radiation emergencies
Mass casualties
Natural disasters and severe weather
Recent outbreaks and incidents (2009)
Year
Name
Description
1918
Spanish flu
20%-40% of world population became ill; more than 20 million people died worldwide
1957
Asian flu
Appeared in two waves; 69,800 died in the United States
1968
Hong Kong flu
33,800 died in the United States
1976
Swine flu scare
Identified and stayed in Fort Dix, NJ, region; mass vaccination program enacted
1977
Russian flu scare
Appeared primarily in children
1997
Avian flu scare
Moved quickly from chicken to people; 18 died of the few hundred affected
Agency
Service
General hospital
Provides short-term care, acute care, and diagnostic and rehabilitation services; may be for profit or nonprofit, teaching or nonteaching
Specialty hospital
Provides treatment for a specific condition such as tuberculosis, mental health disorders, or rehabilitation services
Practitioner office
Provides diagnosis, simple testing, treatments, and counseling services; may be independent or group practice
Long-term care center
Provides personal care for elderly and extended convalescent care
Outpatient care facility
Provides surgical, diagnostic, and ambulatory care
Clinic
Provides combination of practices, which may or may not be supported by public health care funding
Health maintenance
Provides health services at group rates
Home health care
Provides care in the home of the patient; may be publicly or privately owned
Hospice care
Provides medical and psychological care for the terminally ill, either in the home or at a hospice facility; may be private or part of another facility
Assisted living facility
Provides residents a way to live alone or with someone in an apartment; provides services as needed, including meals and health care
Day care
Provides care for the elderly or children and may include care for illness
Public health care
Provides care through federal, state, and local agencies for those who cannot afford to pay for health care and provides preventive services for the entire population
Voluntary organization
Provides research, education, and support for specific concerns; funded by donations and grants
Indemnity (Fee-for-Service)
Managed Health Care (HMO, PPO, POS)
Payment of a monthly fee
Payment of a monthly premium
Yearly deductible for individual and family
Co-payment for office visit
80%-20% split of care after deductible is met
Coinsurance (70%/30% or 80%/20%)
Generally includes preventive care
Yearly deductible for individual and family ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access