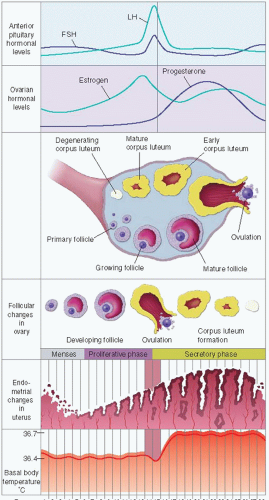
Menstrual or bleeding phase (or early follicular phase): starts day 1 of the cycle and lasts approximately 5 days; endometrial sloughing and discharge occur due to low levels of estrogen and progesterone.
Postmenstrual phase (or early follicular phase); approximately days 5 to 8—thin endometrium. Ovarian follicles grow.
Proliferative phase (or mid- to late follicular phase): approximately days 8 to 15; estrogen starts to increase the thickness of the endometrium. A selected ovarian follicle continues to grow. A surge in LH occurs. Transition from proliferative phase to secretory phase occurs with ovulation, the expulsion of a mature follicle (or ovum) from the ovary.
Secretory phase (or luteal phase, which lasts 14 days after LH surge in most women): approximately days 16 to 23; endometrium thickens because of increased progesterone; after ovulation, a corpus luteum forms and then regresses unless pregnancy occurs.
Premenstrual phase (or late luteal phase): days 24 to 28; levels of estrogen and progesterone begin to fall.
and comfortable setting for history-taking before the patient undresses. Reassure the patient about confidentiality and rationale for history-taking (see Chapter 5, page 46).
Table 22-1 Characteristics of Menstruation | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Menstrual history: date of start of last menstrual period (LMP) or age at last menses. Documented in this manner: age at menarche × cycle length × number of days of bleeding (eg, 13 × 28 × 4). Symptoms of dysmenorrhea? Symptoms of premenstrual syndrome? Intermenstrual spotting/bleeding, postcoital bleeding, or postmenopausal bleeding.
Obstetric history: gravida (number of pregnancies), para (number of term births, preterm births, miscarriages/abortions, living children) (eg, G2P1102). Difficulty conceiving or assisted reproduction? For each pregnancy, list date; gestational age at delivery; mode of delivery; maternal complications (gestational diabetes, hypertension); and fetal, delivery, or neonatal complications.
Cervical cytology/Papanicolaou (Pap) test history: date and result of most recent test? Diagnosis and follow-up of abnormal Pap tests? History of HPV vaccination (as age-appropriate)?
Sexual history: sexual concerns? Partner preference (men, women, or both)? Activity type? Satisfaction? Frequency? Number of partners in past year and during lifetime?
Methods of contraception and sexually transmitted disease (STD) prevention: desire for pregnancy testing or STD screening? Desire for other methods? Desire for preconceptual counseling?
Screening for intimate partner violence and previous emotional, physical, or sexual abuse.
Characteristics: date of LMP? Frequency, duration, and amount of flow for most recent several cycles? Previous menstrual pattern and change? What is the color and consistency of blood? What are the sizes of the clots? Significant change in quantity or quality of menstrual flow? Bleeding or spotting between periods, postcoital bleeding, or postmenopausal bleeding? Pain with bleeding? Age at menarche? Age at menopause?
Associated factors: pregnancy and childbirth history? Is patient sexually active? What method of contraception is used? Is patient taking hormone replacement or hormonal contraceptives? Any other medications? Is patient obese or underweight? Does patient have acne and hirsutism? History of amenorrhea? Coagulation disorders?
Significance: may indicate infection of the vagina or cervix; malignancy of the vulva, vagina, cervix, or uterus; benign tumor of the uterus; ovarian cyst; pregnancy; endometriosis; polycystic ovary syndrome; thyroid disorder; or perimenopausal phase.
Characteristics: color, amount, and duration of the discharge? Any odor, itching, burning, urinary symptoms, or pain? Fever? Dyspareunia (painful intercourse—vulvar, vaginal, or internal pain with intercourse)? Onset related to menses or to intercourse?
Associated factors: LMP? What is the sexual history, such as number of partners or new partner within the past 6 months, type of sexual activity, symptoms in partner? Is barrier method of contraception used? Is patient menopausal or postmenopausal? Environmental factor changes? Vaginal dryness? Does patient take estrogen replacement? Recent use of antibiotics? Recent douching? Recent over-the-counter product use or herbal/natural remedies? History of sexually transmitted diseases?
Significance: may indicate normal or pathologic discharge, bacterial vaginosis, candidal vaginitis, cervicitis, gonorrhea, chlamydia, trichomoniasis, pelvic inflammatory disease (PID), or genital malignancy.
Characteristics: frequency, duration, severity, and location of pain? Does the pain radiate? Was the onset sudden or gradual? What aggravates and what relieves it? Relationship to menstrual cycle, eating, physical exercise, bowel, or bladder function? Any dyspareunia? Does it feel like heaviness in the pelvis? Intensity and effect on daily activities?
Associated factors: LMP? Fever, nausea, vomiting, dizziness, abnormal bleeding? Urinary symptoms? Back pain? Recent significant weight loss or gain? Use of estrogen preparations? Difficulty conceiving? Did patient perform a home pregnancy test? Use of an intrauterine device (IUD)? Any change in bowel habits or diarrhea? History of sexual abuse? Use of pain medications and home remedies?
Significance: may indicate condition arising from relaxed pelvic muscles, PID, endometriosis, interstitial cystitis, urinary tract infection, irritable bowel syndrome, history of sexual abuse (posttraumatic stress disorder), ectopic pregnancy, miscarriage, uterine fibroids, cervical or uterine cancer.
Tell patient a blood test will be performed and the results will be ready in 1 to 3 days.
Not a specific or definitive screening test for ovarian cancer; rather, it is better used as a measure of response to treatment.
Level may be elevated in benign gynecologic disease, hepatic cirrhosis, and in healthy women.
Should not be used as an independent screening tool.
Specimen type—conventional smear (slide) versus liquid based.
Specimen adequacy.
Satisfactory for evaluation—result is given but presence of other factors, such as absence of transformation zone, is also listed.
Unsatisfactory for evaluation—result may not be given; lists reason, such as inadequate number of cells or obscured by blood or inflammation.
Interpretation of results—only a screening tool, not diagnostic.
Negative for intraepithelial lesion or malignancy: no cell abnormalities.
Presence of an organism (trichomonas, fungal elements, shift in flora) and cellular changes consistent with HSV may also be listed.
Other non-neoplastic findings (reactive reparative changes, glandular cells, atrophy) may be described.
Epithelial cell abnormalities—atypical squamous cells are common.
Atypical squamous cells of undetermined significance— management options based on population and can include HPV testing, repeat Pap test in 6-month intervals, and/or colposcopy.
Atypical squamous cells, cannot exclude high-grade intraepithelial lesion—potentially more serious; do immediate colposcopy and endocervical sampling for further evaluation.
Low-grade squamous intraepithelial lesion—management options based on population and can include repeat Pap test in 6-month intervals, HPV testing, and/or colposcopy.
High-grade squamous intraepithelial lesion—management options based on population and can include colposcopy with biopsy and endocervical curettage.
Squamous cell carcinoma—colposcopy and biopsy.
Glandular cell abnormalities—atypical, not otherwise specified (NOS) or atypical, favor neoplastic (require further evaluation); colposcopy, and HPV testing. Endometrial biopsy is performed if over 35 years of age and on younger women with risk factors for endometrial neoplasia such as unexplained uterine bleeding or chronic anovulation.
Endocervical adenocarcinoma in situ; colposcopy, cervical biopsy, conization and possible referral to oncologist.
Hysterectomy may be performed for women who do not desire to preserve fertility.
Adenocarcinoma—endocervical, endometrial, extrauterine, NOS—biopsy and conization; consider referral to gynecologic oncologist.
Perineal drape or other drape
Vaginal speculum of appropriate size (the smaller, the more comfortable; medium or large should be reserved for multiparous and/or obese women)
Warm water
Water-soluble lubricant
Gloves
Long swab sticks
Adequate lighting
Papanicolaou (Pap) smear equipment (spatula, cervical brush, cytology slide and fixative; or cervical broom and liquid-based preparation)
Microscope slide equipment (microscope, glass slides and covers, dropper bottles of normal saline and potassium hydroxide [KOH])
pH paper with range from 3.5 to 5.5 Specimen collection swabs and containers for gonorrhea, chlamydia, or other organisms.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Evidence Base
Evidence Base
Pap test should not be performed during menses, unless the liquid-based system is used.
Instruct patient not to use douche, medication, tampon, or cream in the vagina and to avoid sexual intercourse for 48 hours before the examination.
Recommend regular screening based on established guidelines set forth by the American Cancer Society, U.S. Preventive Services Task Force, and American College of Obstetricians and Gynecologists (ACOG). The same screening guidelines apply to all women whether vaccinated against HPV or not. More frequent testing is recommended if the woman has human immunodeficiency virus (HIV), is immunosuppressed, was exposed to diethylstilbestrol in utero, or has been treated for cervical intraepithelial neoplasia (CIN) 2, CIN 3, or cervical cancer.
Recommend starting Pap testing at age 21.
Recommend testing every 3 years from ages 21-65 for women without risk factors such as DES exposure.
For those aged 30-65 wanting to extend the screening interval, screen with a combination of HPV testing and cytology every 5 years.
Discontinue screening after age 65 if adequate negative prior screening and no history of CIN 2 or greater within the last 20 years.
Discontinue after total hysterectomy if no dysplasia or cancer.
Make sure that patient obtains results. If patient has an abnormal smear, explain that this is not always conclusive but requires further testing based on age, such as repeat Pap test, HPV testing, colposcopy, biopsy, or conization. Encourage patient to return for further testing.
Yearly examination for breast cancer screening, detection of other genital cancers, infections, reproductive problems, and contraception management may be indicated.
 Evidence Base
Evidence Base
Commonly known as deoxyribonucleic acid (DNA) probe or antigen detection tests, a single specimen can detect both STD-causing organisms. Will detect even subclinical infection; can be used as screening test.
Can also be done by culture method, but takes longer and requires separate specimens and special processing for each.
Screening for chlamydia and gonorrhea can also be done on urine specimen using amplified DNA technology. This method is more expensive, but saves time in specimen collection (especially for women) in screening centers.
Explain the procedure to patient before taking the specimen.
Specimens should be taken from the cervix without douching for 24 hours or from the male urethra before urinating.
Obtain specimen with cotton-tipped swab inserted and rotated in the cervical os for 10 seconds or urethral meatus in a male patient. Small-tipped swabs are available for the urethra. Send swab to laboratory in provided container with preservative.
For urine testing, ask the patient to provide the first 10 to 20 mL of voided urine in a specimen container (this represents a urethral specimen that is more likely to contain the organism, if present, without being diluted by a larger amount of urine from the bladder).
May also use ThinPrep as a testing vehicle.
This fluoroscopic x-ray study of the uterus and fallopian tubes is used to determine tubal patency, detect pathology in the uterine cavity, and identify peritoneal adhesions, and for treatment of unexplained fertility.
A bivalve speculum is introduced while patient is in the lithotomy position and contrast medium is injected into the uterine cavity; the medium will enter the peritoneum in 10 to 15 minutes if tubes are patent.
Determine date of last menstrual period; the test is done a few days after menses ends, before ovulation. Obtain pregnancy test if patient is within childbearing years, as indicated.
Verify that the patient does not have a history of allergy to contrast media or iodine.
Administer prescribed antibiotic and analgesic.
After procedure, apply perineal pad for drainage of excess contrast medium or blood and instruct patient to notify health care provider if bloody drainage continues after 3 days or if signs of infection are present.
Inform patient that pain medication may be necessary for shoulder discomfort because of dye irritation of the phrenic nerve.
 Evidence Base
Evidence Base
Inform patient that a full bladder may be necessary to make the uterus easier to visualize.
Instruct patient to drink 16 to 32 ounces of water (may differ among facilities) before the procedure and not to void. If transvaginal ultrasound will be performed, inform patient that a vaginal probe will be inserted to obtain more accurate measurements from internal organs. Have patient empty her bladder prior to insertion of probe. (Probe is not used if patient is virginal.)
After the procedure, help patient wipe off ultrasound gel from abdomen and allow her to empty her bladder.
Abnormalities are represented as different densities that differentiate solid from cystic masses and can help make a diagnosis; however, explain to patient that further testing may be necessary.
Procedure is preferably done when cervix is least vascular (usually 1 week after the end of the menstrual flow). Obtain pregnancy test if patient is within childbearing years, as indicated.
Explain that a vaginal speculum will be inserted and that a biopsy may be taken, causing only slight discomfort.
Help patient into lithotomy position, drape her appropriately, and provide emotional support throughout the procedure. Provide distraction techniques, such as music and posters (hung on the ceiling), as appropriate.
After the cervix and vagina are swabbed with acetic acid solution and inspected through the colposcope, biopsies may be taken. Biopsy tissue is preserved in 10% formalin, labeled, and sent to the laboratory. Saline may be used to rinse the area, and bleeding may be stopped with silver nitrate or ferric subsulfate (Monsel’s solution).
After procedure, assist patient to rise slowly and give the following discharge instructions:
Avoid heavy lifting for 24 hours.
There may be some bleeding and cramping; however, more than that of a normal period must be reported to health care provider.
Obtain health care provider’s instructions regarding douching and sexual intercourse.
Discuss procedure with patient before surgery—does she know why surgery is being done? Does she know which organs will be removed or altered? Does she understand the implications for childbearing, sexuality, menopause? Answer questions and contact surgeon, if necessary.
After the procedure, assess vital signs as frequently as indicated for signs of shock, infection, fluid overload, and atelectasis.
Assess incision for drainage and signs of infection (redness, oozing, warmth, increased pain).
Assess vaginal area for excessive bleeding or foul-smelling drainage.
Monitor intake and output.
If patient has an indwelling catheter, ensure that it is draining clear urine greater than 30 to 50 mL/hour.
After catheter has been removed, ensure that patient voids in adequate amounts and monitor for urinary retention or signs of infection.
Ensure adequate IV and then oral fluids, but monitor for edema and shortness of breath, signs of fluid overload.
Monitor level of pain and relief with analgesics but watch for oversedation, hypotension, and decreased bowel sounds as adverse effects of opioids.
Provide comfort measures, such as positioning, splinting incision during position changing, or coughing, applying ice pack to perineum.
Auscultate bowel sounds for return, signaling progression of diet. Report nausea, vomiting, and loss of or decrease in bowel sounds immediately; intervention for bowel obstruction may be needed.
Institute thromboembolism prevention, as ordered, and monitor for calf tenderness.
Encourage ambulation as early as possible but encourage gradual resumption of activities, according to surgeon instructions.
Notify surgeon of fever, shortness of breath, increased pain, excessive bleeding or drainage, foul odor, change in vital signs, urinary retention, decreased urine output, nausea and vomiting, or tender, swollen calf.
Explain to patient that this test can be a minor surgical procedure that requires local or general anesthesia. Obtain pregnancy test if patient is within childbearing years, as indicated.
After excision, bleeding is controlled by cauterization or suturing and packing.
Patient should be observed for several hours after the procedure for excessive bleeding.
Instruct patient to avoid tampons, douching, and intercourse as well as not to immerse herself in water (no swimming, hot tub, tub bath) for 2 weeks, or as directed by health care provider, to allow healing.
Obtain pregnancy test prior to the procedure if patient is within childbearing years, as indicated.
Administer prescribed sedative before the procedure and explain that a local anesthetic will also be injected into the cervix in the operating room.
Patient will be assisted into the lithotomy position and the perineum and vagina will be cleaned immediately before sterile draping.
Explain that instruments called sounds are inserted into the cervical canal for dilation before insertion of the hysteroscope. With the scope in place, normal saline or CO2 gas is slowly infused into the endometrial cavity to distend it and allow for viewing.
Observe patient for several hours and give discharge instructions.
Over-the-counter analgesics may be needed for minor discomfort if analgesic has not been prescribed.
Notify the health care provider of severe cramping or bleeding, fever, or unusual discharge.
Procedure is done with or without local anesthesia to obtain cells from the uterine lining to assist in the diagnosis of endometrial cancer, menstrual disorders, and infertility.
During speculum examination, a uterine sound is placed, followed by a curette or Pipelle suction device to withdraw specimen.
Obtain pregnancy test if patient is within childbearing years, as indicated.
Administer prostaglandin inhibitor to decrease postoperative uterine cramping.
Assist patient into the dorsal lithotomy position and explain procedure.
Label specimen, place in formalin, and send to laboratory.
Inform patient that she may experience light bleeding and occasional cramping for a few days.
Instruct patient to report fever, chills, and increased bleeding; no tampons, douching, or intercourse for 2 to 3 days.
Contraception is the prevention of fertility on a temporary basis.
Sterilization is the permanent prevention of fertility. Female and male sterilization procedures can be performed. Some procedures can be reversed but with possible complications and variable success rates.
Contraception effectiveness depends on motivation, which is a result of education, culture, religious beliefs, and personal situation. It is best to include both partners in any contraception decision.
Nurses should be familiar with contraceptive methods and educate patients without moral judgment.
Failure rate (pregnancy) is determined by experience of 100 women for 1 year and is expressed as pregnancies per 100 woman-years.
Table 22-2 Contraceptive Methods | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Approaches.
Abdominal is most frequently used: may be postpartum laparotomy, minilaparotomy, or laparoscopy. Laparoscopy with electrocoagulation is frequently performed. It is a safe and effective procedure.
Vaginal incision in posterior vagina (colpotomy) with the uterine tube pulled through it; rarely done due to higher rate of complications—infection.
Uterine approach utilizing hysteroscopy to visualize the tubal ostia and insert coils or plugs.
Techniques vary by surgeon preference.
Electrocoagulation: burn section of tube with or without excision; low reversal rate.
Pomeroy: the tube is tied in midsection and section removed; may be reversed.
Fimbriectomy: the fimbriated end removed and end tied; irreversible.
Cornual resection: removal of the section of tube nearest uterus and suture cornual opening closed.
Silastic bands: plastic or metal clips to occlude tube; may be reversed, although rare.
Coils or plugs inserted in the tubal ostia through hysteroscopy.
Failure to successfully block the tubes—pregnancy or tubal pregnancy.
Hemorrhage, infection, uterine perforation, damage to bowel, bladder, or aorta.
Assess motivation for sterilization and level of knowledge about the procedure. Informed consent is needed. The couple should be thoroughly counseled about the permanence of the procedure.
Teach patient there is no effect on hormones and menstruation will continue.
Teach patient there should not be any adverse effect on sexual response.
Birth control methods are discontinued immediately before the procedure.
Prepare patient to expect some abdominal soreness for several days; instruct her to report any bleeding, increasing pain, or fever.
Sexual intercourse and strenuous activity should be avoided for 2 weeks.
Prepare patient for the procedure—answer questions; request that she void; administer an enema, if ordered; and administer nonsteroidal anti-inflammatory drug (NSAID) or a sedative, as directed.
Immediately postoperatively, monitor vital signs at frequent intervals; potential for hemorrhage exists.
Monitor perineal pads and the bed for amount of bleeding; report excessive amounts.
Offer prescribed analgesics for lower back and pelvic pain; cramping may occur for 2 to 3 days because of dilation of the cervix.
Instruct patient to maintain decreased activity for remainder of day to decrease cramping and bleeding.
Instruct patient to use perineal pads at home and to report fever (more than 100.4°F), heavy bleeding (saturating a pad within 1 hour more than once), cramps lasting longer than 48 hours, increasing pain, prolonged or a foul-smelling vaginal discharge.
Instruct patient to avoid strenuous activity until bleeding stops.
Inform patient that the procedure does not affect sexual functioning, but that she should refrain from sexual intercourse, douching, and tampons for at least 2 weeks, according to preference of health care provider.
Obtain pregnancy test if patient is within childbearing years, as indicated.
Prepare patient by ensuring that she has taken nothing by mouth (NPO), answering questions about the procedure, and administering a sedative and enema, if ordered.
Inform patient that she may experience shoulder or abdominal discomfort after the procedure from the infusion of carbon dioxide given to separate the intestines from pelvic organs. Elevation of feet higher than shoulders after the procedure helps relieve this.
Patient will receive local, general, or regional anesthesia and will be placed in Trendelenburg’s position to displace the intestines for better visualization.
After procedure, monitor bleeding and vital signs and administer analgesics, as indicated.
Inform patient that passing gas and bowel movements may be difficult initially because of the manipulation of the intestines; ambulation and fluids will be helpful.
Advise patient not to have intercourse or to perform strenuous activity for 2 to 3 days and to report bleeding, cramping, or fever. For more complex procedures, return to normal activities, as directed by the health care provider.
Abdominal.
Subtotal/supracervical hysterectomy—corpus of uterus is removed, but cervical stump remains.
Total hysterectomy—entire uterus is removed, including cervix; tubes and ovaries remain.
Total hysterectomy with bilateral salpingo-oophorectomy— entire uterus, tubes, and ovaries are removed.
Vaginal—removal of uterus and cervix through vagina.
Laparoscopically assisted vaginal hysterectomy—allows for the removal of pelvic adhesions that would otherwise prevent vaginal hysterectomy.
Laparoscopic supracervical hysterectomy—laparoscopic removal of the uterus that spares the cervix.
Laparoscopic total hysterectomy—laparoscopic removal of the entire uterus and cervix.
Uterine fibroids, endometriosis and adenomyosis, dysfunctional uterine bleeding—most common.
Uterine prolapse, chronic pelvic pain.
Cancer of the vagina, cervix, uterus, ovaries, or fallopian tubes.
Obstetric complications—rare.
Procedure and reason for hysterectomy, what the procedure involves, and what to expect postoperatively are explained.
Patient must remain NPO from midnight the night before surgery and must void before surgery.
An enema may be administered before surgery to evacuate the bowel and prevent contamination and trauma during surgery.
Vaginal irrigation is performed before surgery and skin preparation is done, if ordered.
Implement the Universal Protocol for Preventing Wrong Site, Wrong Procedure, Wrong Person Surgery (see Chapter 7).
Preoperative medication is given to help the patient relax.
Postoperatively, the following assessments are made:
Wound appearance and drainage.
Vital signs, level of consciousness.
Level of pain and comfort to include nausea and vomiting.
Vaginal drainage (serous, bloody).
Intake and output.
Urge to void, bladder distention, residual urine (if appropriate).
Clarity, color, and sediment of urine.
Homans’ sign or impaired circulation.
Return of bowel sounds, passage of flatus, first bowel movement.
Exercise and ambulation are encouraged to prevent thromboembolus, facilitate voiding, and stimulate peristalsis.
Incisional/pelvic infection.
Hemorrhage.
Urinary tract injury.
Bowel obstruction.
Thrombophlebitis/venous thrombus emboli.
Acute Pain related to surgical procedure.
Impaired Urinary Elimination related to decreased sensation and stimulation.
Risk for Infection related to surgical procedure.
Disturbed Body Image related to alteration in female organs and hormones.
Sexual Dysfunction related to alteration in reproductive organs and function.
Assess pain location, level, and characteristics.
Administer prescribed pain medications. Ensure that patient knows how to use patient-controlled analgesia pump and is using it properly.
Encourage patient to splint incision when moving.
Encourage patient to ambulate as soon as possible to decrease flatus and abdominal distention.
Institute sitz baths or ice packs, as prescribed, to alleviate perineal discomfort.
Monitor level of sedation related to opioid administration— may interfere with ambulation and elimination.
Monitor intake and output, bladder distention, signs and symptoms of bladder infection.
Maintain patency of indwelling catheter if one is in place.
Catheterize patient intermittently if uncomfortable or if she has not voided in 8 hours.
Catheterize to check for residual urine after patient voids; should be less than 100 mL. Continue to check if more than 100 mL, or bladder infection may develop.
Encourage patient to empty bladder around the clock, not only when feeling the urge, because of loss of sensation of bladder fullness.
Encourage fluid intake to decrease risk of urinary infection.
Assess vaginal drainage amount, color, and odor, incision site, and temperature.
Administer antibiotics, as prescribed.
Assist use of incentive spirometer, coughing and deep breathing, and ambulation to decrease risk of pulmonary infection. Monitor respirations and breath sounds for compromise.
Allow patient to discuss her feelings about herself as a woman.
Reassure patient she is still feminine.
Encourage patient to discuss her feelings with her spouse or significant other.
Reassure patient that she will not go through premature menopause if her ovaries were not removed.
Discuss changes regarding sexual functioning, such as shortened vagina and possible dyspareunia because of dryness.
Offer suggestions to improve sexual functioning.
Use of water-soluble lubricants.
Change position—female-dominant position offers more control of depth of penetration.
Advise patient that a total hysterectomy with bilateral salpingo-oophorectomy produces a surgical menopause. Patient may experience hot flashes, vaginal dryness, and mood swings unless short-term hormonal replacement therapy is instituted.
Advise patient against sitting too long at one time, as in driving long distances, because of the possibility of blood pooling in the lower extremities, which increases the risk of thromboembolism.
Suggest that patient delay driving a car until the third postoperative week because even pressing the brake pedal puts stress on the lower abdomen. Avoid hazardous activities when taking opioid analgesics.
Tell patient to expect a tired feeling for the first few days at home and not to plan too many activities for the first week. She can perform most of her usual daily activities within 4 to 6 weeks or per provider instruction. Teach patient that the recovery period differs for each individual and is dependent on medical history and any complications that may have occurred. Inform her that it may be 2 to 3 months or even a year “to feel like herself again.”
Tell patient not to feel discouraged if, at times during convalescence, she experiences depression, feels like crying, and seems unusually nervous. This is common but will not last. Tell patient to call her provider if the feelings persist.
Remind patient to ask her surgeon about strenuous or lifting activities, which are usually restricted for 4 to 6 weeks.
Reinforce instructions given by the surgeon on intercourse, douching, and use of tampons, which are usually discouraged for 6 to 8 weeks. Sexual intercourse should be resumed cautiously to prevent injury and discomfort. Showers are permitted, but tub baths are deferred until healing is sufficient.
Instruct patient to report fever higher than 100°F (37.8°C), heavy vaginal bleeding, drainage, increased pain or cramping, foul odor of discharge, and bleeding or increased drainage from incision site.
Emphasize the importance of follow-up visits and routine physical and gynecologic examinations.
Verbalizes decreased pain.
Voids every 4 to 6 hours of sufficient quantity.
No fever or signs of infection.
Verbalizes positive statements about self and positive outlook on recovery.
Verbalizes understanding of possible changes in sexual functioning and what to do about it.
 Evidence Base
Evidence Base
No pelvic lesion; usually intrinsic to uterus.
Current research supports increased prostaglandin production by the endometrium as the chief cause.
May also be because of hormonal, obstructive, and psychological factors.
Caused by lesion, such as endometriosis, pelvic infection, congenital abnormality, uterine fibroids, or ovarian cyst or may be caused by passage of a clot through undilated cervix.
Pain may be caused by increased uterine contractility and uterine hypoxia.
Characteristics of pain—recurrent, crampy, colicky or dull, usually in lower midabdominal region; spasmodic or constant.
Nausea, vomiting, diarrhea, headache, chills, tiredness, nervousness, and lower backache may be experienced.
Usually self-limiting without complications.
Chlamydia and gonorrhea tests—may show infection.
Pelvic ultrasound—may detect tumor, endometriosis, cysts.
Serum or urine pregnancy test—to rule out ectopic pregnancy.
Possibly, hysteroscopy and laparoscopy—primarily to detect endometriosis.
Nonsteroidal anti-inflammatory agents, such as ibuprofen or naproxen sodium for their antiprostaglandin action. Most effective with loading dose 1 to 2 days before onset of menses and taken on a regular schedule for 2 to 3 days.
Local heat, such as heating pad, to increase blood flow and decrease spasms, for 20-minute intervals More effective in combination with other therapies.
Hormonal contraceptives to decrease contractility and menstrual flow. Evidence supports decreased dysmenorrhea symptoms with monthly oral contraceptives, extended-cycle oral contraceptives, intravaginal hormonal devices, and intrauterine hormonal systems.
Possibly—exercise to increase endorphin release, which decreases pain perception, and to suppress prostaglandin release. More evidence is needed to support this intervention.
Obtain menstrual and gynecologic history that could suggest underlying pathology.
Assess level of pain using scale of 1 to 10; assess patient’s emotional response to pain, coping mechanisms, and ability to carry out activities.
Obtain vital signs, including temperature, to rule out infection.
Perform abdominal and pelvic examination (if indicated) to obtain specimens.
Acute Pain related to uterine contractions.
Risk for Activity Intolerance related to pain severity and associated symptoms.
Readiness for Enhanced Coping related to chronic, recurrent condition.
Administer pharmacologic agents, as ordered, to control pain and menstrual flow.
Apply heating pad to lower back or abdomen, as indicated, for 20-minute intervals.
Assess patient’s response to pain-control measures.
Encourage verbalization of feelings and reassure patient through the evaluation process.
Encourage activity and exercise, as tolerated.
Explain to patient possible causes of dysmenorrhea.
Teach patient nonpharmacologic methods to reduce pain.
Apply heating pad to lower midabdomen or back or take warm tub baths for 20-minute intervals.
Exercise regularly (30 minutes, five or more times per week).
Healthy eating habits; see www.myplate.gov.
Smoking cessation.
Teach patient to use prescribed medications effectively by taking medication at beginning of discomfort and repeating as necessary, especially on first day of menses.
Teach patient adverse effects of medications.
Encourage patient to reduce stress through adequate sleep, good nutrition, exercise, smoking cessation, and coping with stressors.
Discuss patient’s feelings toward menstruation (hygienic issues, inconvenience, female identity).
Verbalizes reduced pain level.
Demonstrates participation in functional activities of daily living without intolerance.
Describes methods to reduce pain and to increase coping skills.
 Evidence Base
Evidence Base
Etiologic theories include hormonal imbalances, such as ovarian steroid interaction; dysfunction of neurotransmitters (such as serotonin), prostaglandins, or endorphins; psychological factors, such as attitudes and beliefs related to menstruation; and environmental factors, such as nutrition and pollution.
Most common in women in their 30s.
May occur in 20% to 32% of menstruating women. Up to 80% of women experience one or more of the symptoms during the luteal phase of their menstrual cycle.
Symptoms may begin 7 to 14 days before onset of menstrual flow; may diminish 1 to 2 days after menses begins.
Physical—edema of extremities, abdominal fullness, breast swelling and tenderness, headache, vertigo, palpitations, acne, backache, constipation, thirst, weight gain.
Psychological and behavioral—labile mood, irritability, fatigue, lethargy, depressed mood, anxiety, crying spells, changes in appetite, decreased concentration.
Diagnosis based on clinical manifestations; usually neither diagnostic laboratory nor radiological evaluation is necessary.
Usually self-limiting without complications.
First-line pharmacological therapy for severe PMS or PMDD includes selective serotonin reuptake inhibitors (SSRIs) such as citalopram, escitalopram, fluoxetine, and sertraline; and serotonin-norepinephrine reuptake inhibitors such as venlafaxine.
Drospirenone (a spironolactone derivative diuretic) combined with low-dose estrogen in oral contraceptives helps symptoms. Theoretically, longer cycles of oral contraceptives with shorter inactive phases would ameliorate symptoms by suppressing natural hormones.
Calcium supplementation of 1,200 mg elemental calcium per day has good evidence that supports decreased mood swings, irritability, depression, and anxiety.
Vitamin B6 supplements of 50 to 100 mg daily (should not exceed 100 mg/day).
Cognitive-behavioral therapy has some limited evidence supporting relief of symptoms.
Healthy lifestyle changes, such as restriction of sodium, caffeine, tobacco, alcohol, and refined sweets, and inclusion of aerobic exercise, while are often recommended, have insufficient evidence to support their efficacy in treatment of PMS symptoms.
High-dose daily vitamin D intake is supported by some evidence.
Prostaglandin inhibitors such as ibuprofen will decrease dysmenorrhea-related symptoms.
Spironolactone, a diuretic with androgenic effect, may decrease fluid retention and weight gain.
With great caution because of abuse potential, anxiolytic agents may be prescribed for use during the luteal phase for patients with anxiety symptoms.
Chasteberry, an herbal supplement, 20 mg daily was shown to be effective in one randomized controlled trial.
 DRUG ALERT
DRUG ALERT
Ask patient to describe symptoms, their onset, and means of relief.
Assess patient’s diet, activity, and rest habits.
Assess patient’s emotional response to symptoms and methods of coping.
Deficient knowledge related to self-care measures.
Anxiety related to symptoms and difficulty coping with condition.
Administer medications, as ordered; warn patient that diuretics will cause increased urination and anxiolytics may cause drowsiness or cognitive impairment.
Provide emotional support for patient and significant others.
Teach stress management and relaxation measures such as imagery and progressive muscle relaxation (see Chapter 3).
Suggest counseling, as indicated.
Encourage patient to keep a diary for several consecutive months, which includes dates, cycle days, stressors, symptoms, and their severity, to determine if therapy is effective.
Instruct patient in the use and adverse effects of prescribed medications.
Teach patient possible causes of syndrome and nonprescription methods to alleviate distress, such as calcium and vitamin B6 intake.
Refer for further resources and support to such groups as the National Association for Premenstrual Syndrome (UK) (http://pms.org.uk) or womenshealth.gov, a project of the U.S. Department of Health and Human Services Office on Women’s Health (www.womenshealth.gov).
Verbalizes increased knowledge and sense of control over condition.
Reduced signs and symptoms of anxiety.
Menarche does not occur by age 16 with pubertal development or by age 14 with absence of secondary sex characteristics.
May be caused by chromosomal disorders, such as Turner’s syndrome, agenesis of the uterus, or constitutional delay of growth and puberty.
Transverse vaginal septum or imperforate hymen.
Menstruation stops for 3 months in women with previously established regular menstrual cycles or 9 months in a woman with previously established oligomenorrhea (infrequent or longer menstrual cycles).
May be caused by pregnancy, lactation, menopause, or corpus luteal ovarian cysts.
Excessive exercise, inadequate nutrition with decreased body fat stores, and excessive weight loss may cause amenorrhea in young athletes (included in the female athlete triad: an eating disorder, amenorrhea, and osteoporosis).
Amenorrhea and anovulation secondary to polycystic ovary syndrome (PCOS) commonly occurs in obese women but may be seen in women with normal body mass index (BMI).
Ovarian, adrenal, or pituitary tumors and thyroid disorders are hormonal causes.
Some medications, such as antipsychotics (phenothiazines), antidepressants, antihypertensives, histamine H2 blockers, opiates, chemotherapy, and hormonal contraceptives, may also induce amenorrhea.
It may be a result of severe depression, severe psychological trauma, physical trauma, or radiation.
Pregnancy test.
Prolactin level (elevated) with pituitary tumor.
Thyroid-stimulating hormone (TSH)
Progesterone challenge test in secondary amenorrhea if both prolactin and TSH are normal.
Positive result—bleeding occurs; chronic anovulation is most likely.
Negative result—no bleeding occurs; may indicate ovarian failure; other tests are needed.
Hormonal levels—LH and FSH—to determine type of hypogonadism in primary amenorrhea or to detect ovarian failure in secondary amenorrhea.
Genetic karyotyping to detect chromosome abnormalities in primary amenorrhea.
Ultrasound to identify presence of uterus and/or outflow obstruction.
Discontinue causative medications if benefit of discontinuance outweighs risk.
Nutritional, exercise, or psychological counseling, as indicated.
Recommend decreased exercise in athletes to increase body fat stores and restore normal BMI.
Recommend weight reduction if obese.
Low-dose hormonal contraceptives to regulate cycle after underlying cause has been determined.
In polycystic ovarian syndrome, insulin-sensitizing agents decrease androgen levels, improve ovulation rate, and improve glucose tolerance. Clomiphene citrate is first-line for ovulation induction. Laser treatment plus eflornithine is indicated for hirsutism in PCOS.
Treatment of tumor or other underlying cause. Surgery, as indicated.
Amenorrhea increases risk for osteoporosis and endometrial hyperplasia, which may lead to atypia and cancer of the endometrium.
PCOS conveys risk of metabolic syndrome, type 2 diabetes, and cardiovascular disease. Improvement in ovulation rate increases the risk of pregnancy.
Assess for signs of chromosomal disorders, such as abnormal genitalia, masculinization, short stature, and characteristic facies.
Assess for signs of pituitary tumor, such as headache, vision disturbances, dizziness, and galactorrhea.
Assess weight and body build, BMI, change in weight, and nutritional and exercise habits that may indicate anorexia or loss of body fat because of exercise.
Assess for signs of PCOS: elevated blood pressure, elevated BMI, waist circumference, stigmata of insulin resistance, hirsutism.
Assess emotional status, areas of stress, and coping ability.
Imbalanced Nutrition: Less Than Body Requirements related to inadequate nutritional intake and/or rigorous exercise.
Imbalanced Nutrition, More Than Body Requirements related to obesity or PCOS.
Disturbed Body Image related to lack of menses, perception of inappropriate weight.
Explore knowledge of the food groups, behavior regarding meals, and exercise routine; point out misconceptions, dangerous behavior, and ideas for improvement.
Monitor weight and BMI and return of menstrual cycles.
Explore patient’s body image and coping strategies. Provide emotional support for patient and family.
Describe diagnostic tests and who will give results to patient.
Point out ineffective coping mechanisms and teach more positive coping mechanisms such as assertiveness. Instruct in relaxation techniques.
Teach patient the physiology of the normal menstrual cycle and possible causes in diagnostic workup for amenorrhea.
Teach proper use and adverse effects of prescribed medications.
Teach patient to chart menstrual periods on a calendar and maintain regular gynecologic and medical follow-up visits.
Teach patients with PCOS that they should be screened for type 2 diabetes and cardiovascular risk factors such as fasting lipid levels and body mass index.
Verbalizes adequate dietary intake and appropriate exercise regimen.
Achieves normal body mass index with restoration of menses.
Verbalizes understanding of diagnostic tests and improved body image.
 Evidence Base
Evidence Base
Common causes of anovulatory AUB include polycystic ovarian syndrome (PCOS), uncontrolled diabetes mellitus, thyroid disorders (hypo- and hyperthyroidism), hyperprolactinemia, or medications (such as antipsychotics and anti-epileptics).
In adolescents, AUB is frequently caused by immature hypothalamic-pituitary-ovarian axis.
Ovarian failure in perimenopausal women frequently causes DUB. Recurrent irregular menstrual cycles are considered abnormal if they occur 8 years before menopause.
Anovulation may be related to hypothalamic or pituitary dysfunction, impaired follicular formation or rupture, or corpus luteum dysfunction.
Temporary estrogen withdrawal at ovulation may cause mid-cycle ovulatory bleeding.
Excessive bleeding or duration may be related to hypothyroidism, late-stage liver disease, or bleeding disorders (such von Willebrand disease).
Structural abnormalities, such as submucosal fibroids or endometrial fibroids, may cause AUB.
Approximately one half of women with ovulatory AUB have no identifiable cause.
Amenorrhea—no bleeding for three cycles or more (see page 849).
Oligomenorrhea—significantly diminished menstrual flow; infrequent intervals (greater than 35 days) or irregular intervals.
Metrorrhagia—bleeding from uterus between regular menstrual periods; significant because it is usually a symptom of disease.
Menometrorrhagia—excessive bleeding at the usual time of menstruation and at other irregular intervals.
Menorrhagia—excessive bleeding during regular menstruation cycles; can be increased in duration or amount.
Polymenorrhea—frequent menstruation occurring at intervals of less than 21 days.
Menometrorrhagia—excessive bleeding at the usual time of menstruation and at other irregular intervals.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


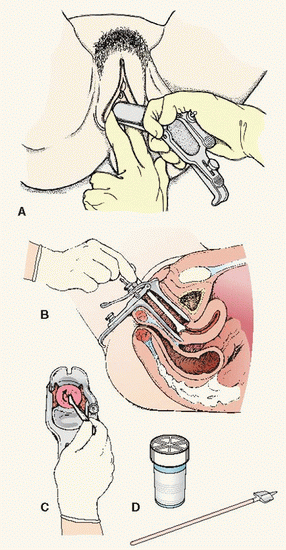 (A) Insertion of vaginal speculum during pelvic examination. (B) Cervical cytology specimen collection: either conventional or liquid-based preparations are acceptable for cervical cancer screening. A scraping of endocervical and exocervical cells is obtained using a spatula and cervical brush or using a cervical broom. (C) The spatula, which obtains exocervical cells (inserted with the longer end in the cervical os), and cervical brush, which obtains endocervical cells, are rotated in the os, smeared on a microscope slide, and finished with a fixative. (D) The cervical broom obtains samples from both the endocervix and the exocervix by rotation in the os. The handle is detached and the broom is sent in liquid medium for processing; or the brush is rinsed in the preservative with 15 strokes and the liquid then sent for processing.
(A) Insertion of vaginal speculum during pelvic examination. (B) Cervical cytology specimen collection: either conventional or liquid-based preparations are acceptable for cervical cancer screening. A scraping of endocervical and exocervical cells is obtained using a spatula and cervical brush or using a cervical broom. (C) The spatula, which obtains exocervical cells (inserted with the longer end in the cervical os), and cervical brush, which obtains endocervical cells, are rotated in the os, smeared on a microscope slide, and finished with a fixative. (D) The cervical broom obtains samples from both the endocervix and the exocervix by rotation in the os. The handle is detached and the broom is sent in liquid medium for processing; or the brush is rinsed in the preservative with 15 strokes and the liquid then sent for processing.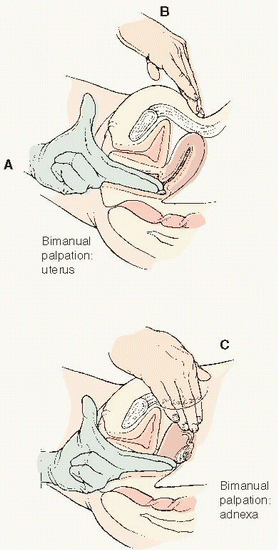 Bimanual examination of the pelvic organs. (A) Insert two fingers of dominant hand into vagina. (B) Place second hand over midline lower abdomen. Gently capture the uterus between your two hands to feel the contour and size and to elicit tenderness. (C) Move hands to either side of midline to palpate the adnexa, feeling for swelling, masses, or tenderness of the ovaries and fallopian tubes. Source: From Fuller J and Schaller-Ayers J. Health Assessment: A Nursing Approach, 2nd ed. Philadelphia: J.B. Lippincott Company, 1994.
Bimanual examination of the pelvic organs. (A) Insert two fingers of dominant hand into vagina. (B) Place second hand over midline lower abdomen. Gently capture the uterus between your two hands to feel the contour and size and to elicit tenderness. (C) Move hands to either side of midline to palpate the adnexa, feeling for swelling, masses, or tenderness of the ovaries and fallopian tubes. Source: From Fuller J and Schaller-Ayers J. Health Assessment: A Nursing Approach, 2nd ed. Philadelphia: J.B. Lippincott Company, 1994. Evidence Base Saslow, D., Solomon, D., Lawson, H. W., et al. (2012). American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA—Cancer Journal for Clinicians, 62, 147-172.
Evidence Base Saslow, D., Solomon, D., Lawson, H. W., et al. (2012). American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA—Cancer Journal for Clinicians, 62, 147-172. NURSING ALERT Warn patients who use condoms, diaphragms, and the cervical cap that latex sensitivity may be a problem—watch for itching, swelling, generalized reactions.
NURSING ALERT Warn patients who use condoms, diaphragms, and the cervical cap that latex sensitivity may be a problem—watch for itching, swelling, generalized reactions.