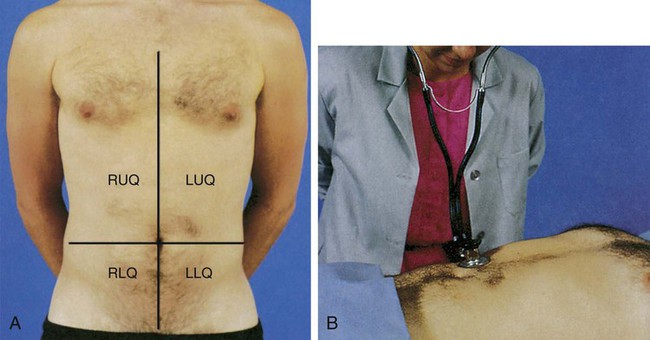
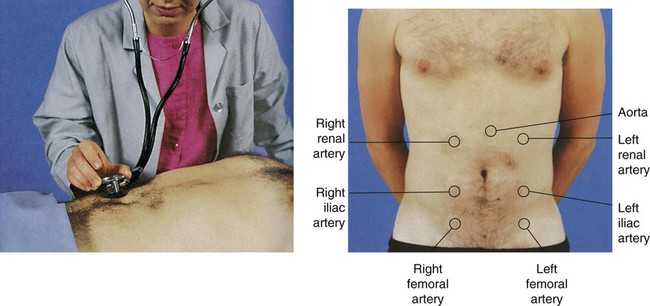
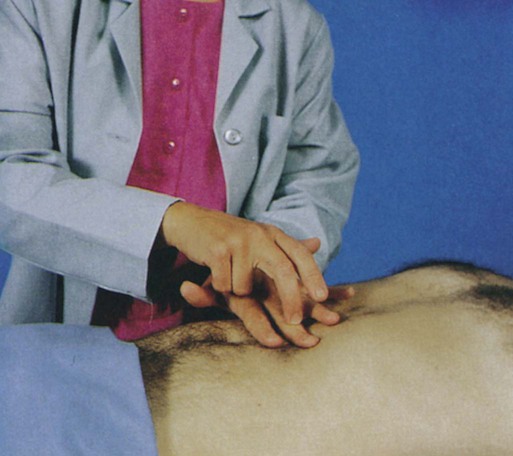
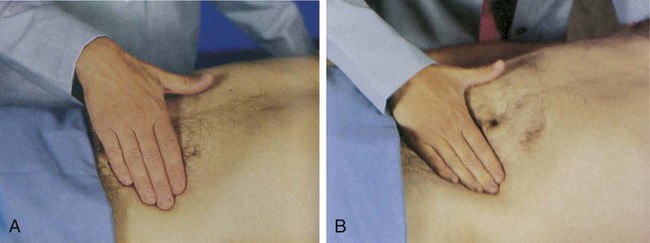
Chapter 29 A thorough clinical assessment of the patient with GI dysfunction is imperative for the early identification and treatment of GI disorders. The completed assessment serves as the foundation for developing the management plan for the patient. The assessment process can be brief or can involve a detailed history and examination, depending on the nature and immediacy of the patient’s situation.1,2 The initial presentation of the patient determines the rapidity and direction of the interview. For a patient in acute distress, the history should be curtailed to a few questions about the patient’s chief complaint and the precipitating events. For a patient in no obvious distress, the history should focus on current symptoms, the patient’s medical history, and the family’s history. Specific items regarding each of these areas are outlined in Box 29-1, Data Collection.3,4 The physical examination helps establish baseline data about the physical dimensions of the patient’s situation.3 The abdomen is divided into four quadrants (left upper, right upper, left lower, and right lower), with the umbilicus as the middle point, to specify the location of examination findings (Fig. 29-1 and Box 29-2). The assessment should proceed when the patient is as comfortable as possible and in the supine position; however, the position may need readjustment if it elicits pain. To prevent stimulation of GI activity, the order for the assessment should be changed to inspection, auscultation, percussion, and palpation.4 Observe the skin for pigmentation, lesions, striae, scars, petechiae, signs of dehydration, and venous pattern. Pigmentation may vary considerably and still be within normal limits because of race and ethnic background, although the abdomen usually is of a lighter color than other exposed areas of the skin. Abnormal findings include jaundice, skin lesions, and a tense and glistening appearance of the skin. Old striae (stretch marks) usually are silver, whereas pinkish purple striae may indicate Cushing syndrome.4 A bluish discoloration of the umbilicus (Cullen sign) and of the flank (Grey-Turner sign) indicates retroperitoneal bleeding.1 Observe the abdomen for contour, noting whether it is flat, slightly concave, or slightly round; observe for symmetry and for movement. Marked distention is an abnormal finding. In particular, ascites may cause generalized distention and bulging flanks. Asymmetric distention may indicate organ enlargement or a mass. Peristaltic waves should not be visible except in very thin patients. In the case of intestinal obstruction, hyperactive peristaltic waves may be observed. Pulsation in the epigastric area is often a normal finding, but increased pulsation may indicate an aortic aneurysm. Symmetric movement of the abdomen with respirations is usually seen in men.4,5 Auscultation of the abdomen provides clinical data regarding the status of the bowel’s motility. Initially, listen with the diaphragm of the stethoscope below and to the right of the umbilicus. The examination proceeds methodically through all four quadrants, lifting and then replacing the diaphragm of the stethoscope lightly against the abdomen (see Fig. 29-1). Normal bowel sounds include high-pitched, gurgling sounds that occur approximately every 5 to 15 seconds or at a rate of 5 to 34 times per minute. Colonic sounds are low pitched and have a rumbling quality. A venous hum may be audible sometimes.6 Table 29-1 provides a list of abnormal abdominal sounds. TABLE 29-1 LUQ, Left upper quadrant; RUQ, right upper quadrant. From Doughty DB, Jackson DB. Gastrointestinal Disorders. St. Louis: Mosby; 1993. Abnormal findings include the absence of bowel sounds throughout a 5-minute period, extremely soft and widely separated sounds, and increased sounds with a high-pitched, loud rushing sound (peristaltic rush). Absent bowel sounds may result from inflammation, ileus, electrolyte disturbances, and ischemia. Bowels sounds may be increased with diarrhea and early intestinal obstruction.6 The abdomen should be auscultated for the presence of bruits, using the bell of the stethoscope (Fig. 29-2). Bruits are created by turbulent flow over a partially obstructed artery and are always considered an abnormal finding. The aorta, the right and left renal arteries, and the iliac arteries should be auscultated.5,6 Percussion is used to elicit information about deep organs such as the liver, spleen, and pancreas (Fig. 29-3). Because the abdomen is a sensitive area, muscle tension may interfere with this part of the assessment. Percussion often helps relax tense muscles, and it is performed before palpation. Percussion in the absence of disease helps delineate the position and size of the liver and spleen, and it assists in the detection of fluid, gaseous distention, and masses in the abdomen.5 Percussion should proceed systematically and lightly in all four quadrants. Normal findings include tympany over the empty stomach, tympany or hyper-resonance over the intestine, and dullness over the liver and spleen. Abnormal areas of dullness may indicate an underlying mass. Solid masses, enlarged organs, and a distended bladder also produce areas of dullness. Dullness over both flanks may indicate ascites and necessitates further assessment.6 Palpation is the assessment technique most useful in detecting abdominal pathologic conditions. Light and deep palpation of each organ and quadrant should be completed. Light palpation, which has a palpation depth of approximately 1 cm, assesses to the depth of the skin and fascia (Fig. 29-4A). Deep palpation assesses the rectus abdominis muscle and is performed bimanually to a depth of 4 to 5 cm (see Fig. 29-4B). Deep palpation is most helpful in detecting abdominal masses. Areas in which the patient complains of tenderness should be palpated last.6 Normal findings include no areas of tenderness or pain, no masses, and no hardened areas. Persistent involuntary guarding may indicate peritoneal inflammation, particularly if it continues even after relaxation techniques are used. Rebound tenderness, in which pain increases with quick release of a palpated area, indicates an inflamed peritoneum.4 Table 29-2 presents a variety of common GI disorders and their associated assessment findings. TABLE 29-2 ASSESSMENT FINDINGS OF COMMON GASTROINTESTINAL DISORDERS
Gastrointestinal Clinical Assessment and Diagnostic Procedures
Clinical Assessment
History
Physical Examination
Inspection
Auscultation
SOUND
CAUSE
Hyperactive bowel sounds (borborygmi), loud and prolonged
Hunger, gastroenteritis, or early intestinal obstruction
High-pitched, tinkling sounds
Intestinal air and fluid under pressure; characteristic of early intestinal obstruction
Decreased (hypoactive) bowel sounds
Possible peritonitis or ileus
Infrequent and abnormally faint sounds
Absence of bowel sounds (confirmed only after auscultation of all four quadrants and continuous auscultation for 5 minutes)
Temporary loss of intestinal motility, as occurs with complete ileus
Friction rubs
Pathologic conditions such as tumors or infection that cause inflammation of organ’s peritoneal covering
High-pitched sounds heard over liver and spleen (RUQ and LUQ), synchronous with respiration
Bruits
Abnormality of blood flow (requires additional evaluation to determine specific disorder)
Audible swishing sounds that may be heard over aortic, iliac, renal, and femoral arteries
Venous hum
Increased collateral circulation between portal and systemic venous systems
Low-pitched, continuous sound
Percussion
Palpation
Assessment Findings for Common Disorders
CONDITION
HISTORY
SYMPTOMS
SIGNS
Right Lower Quadrant (RLQ) of the Abdomen
Appendicitis
Children (except infants) and young adults
Anorexia
Signs may be absent early
Nausea
Vomiting
Early vague epigastric, periumbilical, or generalized pain after 12-24 hours; RLQ at McBurney point
Localized RLQ guarding and tenderness after 12-24 hours
Rovsing sign: pain in RLQ with application of pressure, iliopsoas sign
Obturator sign
White blood cell count of 10,000/mm3 or shift to left
Low-grade fever
Cutaneous hyperesthesia in RLQ
Signs highly variable
Perforated duodenal ulcer
Prior history
Abrupt onset pain in epigastric area or RLQ
Tenderness in epigastric area or RLQ
Signs of peritoneal irritation
Heme-positive stool
Increased white blood cell count
Cecal volvulus
Seen most often in older adults
Abrupt severe abdominal pain
Distention
Localized tenderness
Tympany
Strangulated hernia
Any age
Severe localized pain
If bowel obstructed, distention
Women: femoral
If bowel obstructed, generalized pain
Men: inguinal
Right Upper Quadrant (RUQ) of the Abdomen
Liver hepatitis
Any age, often young blood product user
Fatigue
Hepatic tenderness
Malaise
Hepatomegaly
Drug addict
Anorexia
Bilirubin elevated
Pain in RUQ
Jaundice
Low-grade fever
Lymphocytosis in one third of cases
May have severe fulminating disease with liver failure
Liver enzymes elevated
Hepatitis A or B or antibodies to the viruses may be found
Acute hepatic congestion
Usually older adults with acute heart failure
Symptoms of acute heart failure
Hepatomegaly
Pericardial disease
Acute heart failure
Pulmonary embolism
Biliary stones, colic
“Fair, fat, forty” (90%) but can be 30 to 80 years old
Anorexia
Nausea
Tenderness in RUQ
Jaundice
Pain severe in RUQ or epigastric area
Episodes lasting 15 minutes to hours
Acute cholecystitis
“Fair, fat, forty” (90%) but may be 30 to 80 years old
Severe RUQ or epigastric pain
Vomiting
Episodes prolonged up to 6 hours
Tenderness in RUQ
Peritoneal irritation signs
Increased white blood cell count
Perforated peptic ulcer
Any age
Abrupt RUQ pain
Tenderness in epigastrium, right quadrant, or both
Peritoneal irritation signs
Free air in abdomen
Left Upper Quadrant (LUQ) of the Abdomen
Splenic trauma
Blunt trauma to LUQ of abdomen
Pain: LUQ pain of the abdomen often referred to the left shoulder (Kehr sign)
Hypotension
Syncope
Increased dyspnea
Radiographic studies show enlarged spleen
Pancreatitis
Alcohol abuse
Pain in LUQ or epigastric region radiating to the back or chest
Fever
Pancreatic duct obstruction
Rigidity
Rebound tenderness
Infection
Nausea
Cholecystitis
Vomiting
Jaundice
Cullen sign
Turner sign
Abdominal distention
Diminished bowel sounds
Pyloric obstruction
Duodenal ulcer
Weight loss
Increasing dullness in LUQ
Gastric upset
Visible peristaltic waves in epigastric region
Vomiting
Left Lower Quadrant (LLQ) of the Abdomen
Ulcerative colitis
Family history
Chronic, watery diarrhea with bloody mucus
Fever
Jewish ancestry
Cachexia
Anorexia
Anemia
Weight loss
Leukocytosis
Fatigue
Colonic diverticulitis
Older than 39 years
Pain that recurs in LUQ
Fever
Low-residue diet
Vomiting
Chills
Diarrhea
Tenderness over descending colon ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Gastrointestinal Clinical Assessment and Diagnostic Procedures
Get Clinical Tree app for offline access