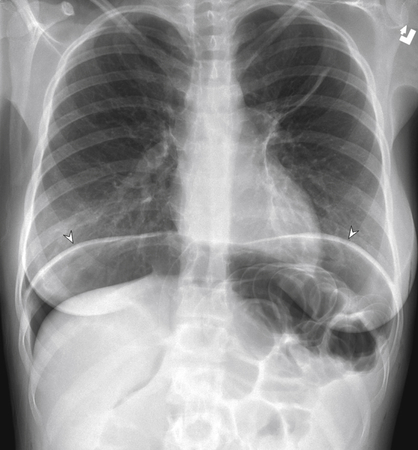
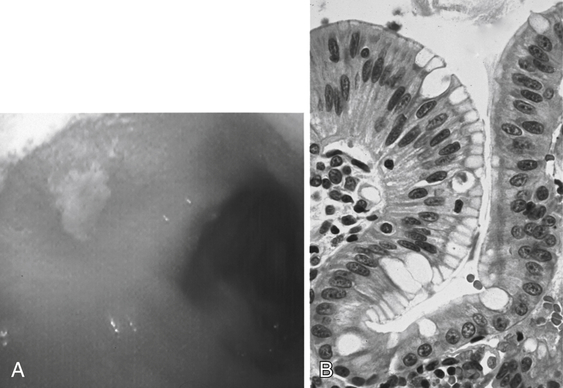
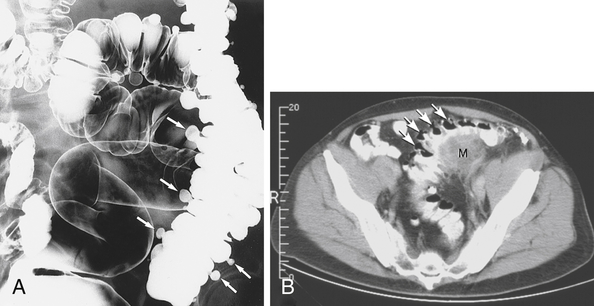
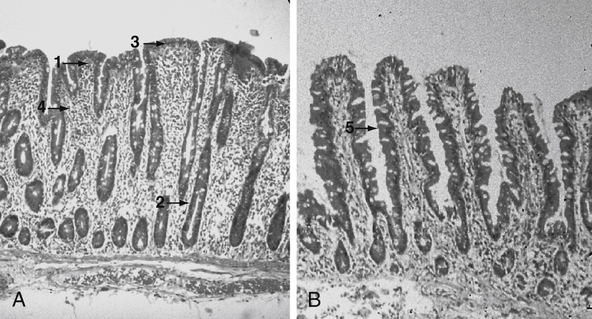
Chapter 12 Sequelae of GERD include esophagitis, esophageal stricture (which may mimic esophageal cancer), esophageal ulcer, hemorrhage, Barrett esophagus, and esophageal adenocarcinoma (Fig. 12-1). The most feared complication of PUD is perforation. Look for peritoneal signs, history of PUD, and free air on an abdominal radiograph (Fig. 12-2). Treat with antibiotics (e.g., ceftriaxone, metronidazole) and laparotomy with repair of the perforation. If ulcers are severe, atypical (e.g., located in the jejunum), or nonhealing, think about stomach cancer or Zollinger-Ellison syndrome (gastrinoma; check gastrin level). PUD is also a cause of GI bleeding, which can be severe in some cases. Signs and symptoms of diverticulitis include left lower quadrant pain or tenderness, fever, diarrhea or constipation, and increased white blood cell count. The pathophysiology is thought to be similar to appendicitis. Stool or other debris impacts within the diverticulum and causes obstruction, leading to bacterial overgrowth and inflammation. The diagnosis can be confirmed with a computed tomography (CT) scan (Fig. 12-4), if needed, which can also help rule out complications such as perforation or abscess. In the absence of complications, the treatment is antibiotics that cover bowel flora (e.g., a fluoroquinolone plus metronidazole) and bowel rest (i.e., no oral intake). Surgery is needed for perforation or abscess. Celiac disease (look for dermatitis herpetiformis, and avoid gluten in the diet; Fig. 12-5; Plate 21), Crohn disease, and postgastroenteritis (because of depletion of brush-border enzymes). Malabsorptive diarrhea improves when the patient stops eating.
Gastroenterology
3 What are the sequelae of GERD?
6 Explain the classic differences between duodenal and gastric ulcers.
DUODENAL
GASTRIC
% of cases
75
25
Acid secretion
Normal to high
Normal to low
Main cause
Helicobacter pylori
Use of nonsteroidal antiinflammatory drugs (NSAIDs), including aspirin
Peak age
40s
50s
Blood type
O
A
Eating food
Pain gets better, then worse 2-3 hours later
Pain not relieved or made worse
8 What is the most feared complication of PUD? What should you suspect if an ulcer does not respond to treatment?
12 What are the classic differences between upper and lower GI bleeds?
UPPER GI BLEED
LOWER GI BLEED
Location
Proximal to ligament of Treitz
Distal to ligament of Treitz
Common causes
Gastritis, ulcers, varices, esophagitis
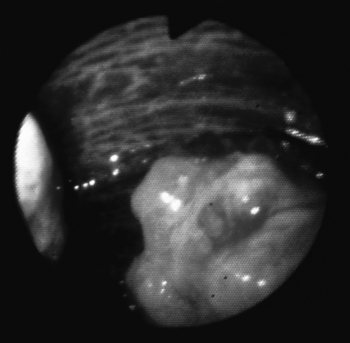
Vascular ectasia, diverticulosis, colon cancer (Fig. 12-3; Plate 20), colitis, inflammatory bowel disease, hemorrhoids
Stool
Tarry, black stool (melena)
Bright red blood seen in stool (hematochezia)
NGT aspirate
Positive for blood
Negative for blood
16 How do you diagnose and treat diverticulitis? What test should a patient have after a treated episode of diverticulitis?
20 What are the common causes of malabsorptive diarrhea?
27 Specify the classic differences between Crohn disease and ulcerative colitis.
CROHN DISEASE
ULCERATIVE COLITIS
Place of origin
Distal ileum, proximal colon
Rectum
Thickness of pathology
Transmural
Mucosa/submucosa only
Progression
Irregular (skip lesions)
Proximal, continuous from rectum; no skipped areas
Location
From mouth to anus
Involves only colon, rarely extends to ileum
Bowel habit changes
Obstruction, abdominal pain
Bloody diarrhea
Classic lesions
Fistulas/abscesses, cobblestoning, string sign on barium x-ray (Fig. 12-6)
Pseudopolyps, lead-pipe colon on barium x-ray (Fig. 12-7), toxic megacolon
Colon cancer risk
Slightly increased
Markedly increased
Surgery
No (may make worse)
Yes (proctocolectomy with ileoanal anastomosis) ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access