G
Gamma-glutamyltransferase
Basics the nurse needs to know
In the range of reference values, there are differences related to gender, age, and ethnicity. The values for adult males are 25% higher than adult females. People of African ancestry have normal values that are double the values of those who are white, for all age groups.
REFERENCE VALUES
Premature newborn: 56-233 U/L or SI: 56-233 U/L at 37° C
Newborn-3 weeks: 10-103 U/L or SI: 10-103 U/L at 37° C
3 weeks-3 months: 4-111U/L or SI: 4-111 U/L at 37° C
1-5 years: 2-23 U/L or SI: 2-23 U/L at 37° C
6-15 years: 2-23 U/L or SI: 2-23 U/L at 37° C
16 years-Adult: 2-35 U/L or SI: 2-35 U/L at 37° C
Gastrin
Purpose of the test
Serum gastrin is a test used to help diagnose Zollinger-Ellison syndrome and gastrinoma.
Interfering factors
NURSING CARE
Nursing actions are similar to those used in other venipuncture procedures (see Chapter 2), with the following additional measures.
Pretest
Gated blood pool studies
Basics the nurse needs to know
A gated blood pool study is a noninvasive method of assessing myocardial function, particularly wall motion of the left ventricle. It also permits evaluation of left ventricular ejection fraction without invasive catheterization. Gated blood pool studies are being replaced by echocardiography (see pp. 270) and gated-SPECT myocardial perfusion imaging. GSPECT (gated single proton emission computed tomography) provides the evaluation of LV function and myocardial perfusion in one study. See pp. 488 for discussion of myocardial perfusion studies.
How the test is done
The procedure for the gated blood pool study is similar to that for myocardial imaging. The red blood cells are tagged with technetium 99m pyrophosphate, a gamma-emitting radionuclide. Because the bound technetium cannot diffuse through cell membranes, it remains in the blood. Its emissions are more concentrated in body cavities with large blood volumes, including the heart chambers.
Interfering factors
NURSING CARE
Pretest
During the test
Genetic sonogram
Includes: Nuchal translucency (NT)
Basics the nurse needs to know
Genetic sonogram
Nuchal translucency imaging is best when done in between the 11th and 14th week of gestation, as one of the recommended combined first trimester screening tests. The combined first trimester screening tests consist of nuchal translucency ultrasound imaging, human chorionic gonadotrophin (p. 193), and pregnancy-associated plasma protein A (p. 514).
For interpretation, the test results are considered as a combined result rather than as single entities. When nuchal translucency, the most sensitive of the triple markers is included, the combined first trimester screening tests have a 90% detection rate of Down syndrome and a 5% false-positive rate (Sonek & Nicolaides, 2010). The second trimester quadruple marker screening tests also assesses for indicators of Down syndrome and neural tube defects. The included tests are serum alpha-fetoprotein (p. 62), human chorionic gonadotrophin (p. 193), unconjugated estriol (p. 306), and inhibin A. The more complete genetic sonogram, including nuchal translucency, may be done late in the first trimester, or in the early part of the second trimester, in the follow-up of abnormal results of the combined first trimester screen or second trimester quadruple marker screening tests.
Nuchal translucency
The nuchal tissue is located in the back of the fetal neck. Nuchal fold translucency is measurable by ultrasound in the 11th to 14th week of gestation; the tissue appears translucent because of fluid or edema. On the sonogram image, the thickness of the translucent tissue of the nuchal fold is measured from the outer surface of the occipital bone to the exterior of the fetal scalp (Figure 52). When the measurement is greater than the reference value, it is an indicator of risk for Down syndrome, cardiac anomalies, and other fetal defects (Sonek and Nicolaides, 2010).
Likelihood ratio
The results are presented as a mathematical score called the Likelihood Ratio (LR). When the likelihood ratio is a large number, the data is considered very convincing. If the likelihood ratio is less than 1 or near zero, the data is considered not very convincing and the abnormal condition is not very likely (McGee, 2007). In the evaluation of the genetic sonogram, the calculation of the likelihood ratio includes the modifiers of maternal age, gestational age of the fetus, test sensitivity, and false-positive percentage. The presence of multiple abnormal images and additional structural defects in the fetus will increase the likelihood ratio score. Abnormal results are greater than 1. Scores of 2 to 5, 5 to 10, or greater than 10 in the likelihood ratio are considered as a small, moderate, or high probability of Down syndrome, respectively.
Interfering factors
NURSING CARE
Pretest
Posttest
Genetic testing for cystic fibrosis
Also called: Cystic Fibrosis; DNA Detection
Basics the nurse needs to know
Cystic fibrosis is an inherited autosomal-recessive genetic disorder. In the heterozygous (carrier) form, the individual has one mutated gene for cystic fibrosis, but does not have the disease or symptoms of the disease. In the homozygous form, the individual inherits two mutated cystic fibrosis genes, one from each carrier parent. This individual inherits cystic fibrosis disease. When both reproductive partners have the heterozygous form of the genetic mutation, each pregnancy has a one in four chance (25% risk) of conceiving a child with cystic fibrosis disease (Figure 53). Cystic fibrosis most commonly affects Caucasian people and the subgroup of Ashkenazi Jewish people. Cystic fibrosis also affects people who are African American, Asian, or Hispanic, but occurs less frequently.
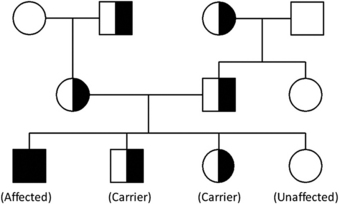
Figure 53. Autosomal recessive inheritance pattern of cystic fibrosis.
(From Goetzinger KR, Cahill AG: An update on cystic fibrosis screening, Clin Lab Med 30 (3):534, 2010.)
The genetic mutation occurs on chromosome 7 and alters the gene called CF transmembrane conductance regulator (CFTR). If the paired CTFR genes are absent or have a mutation, the child with cystic fibrosis will have multiple alterations for fluid and electrolyte transport to cells including dehydrated secretions, thick mucus in the lungs, poor secretion of pancreatic enzymes, altered intestinal function, and increased sodium chloride in sweat (Goetzinger & Cahill, 2010). There are over 1000 identified CFTR mutations in cystic fibrosis. The standard screening panel consists of testing for 23 of the most common mutations.
The genetic testing for cystic fibrosis is not 100% sensitive. One hundred percent sensitivity would mean that the cystic fibrosis mutation will be detected in every tested person who has the mutation. In the current state of genetic testing for cystic fibrosis, there are some false-negative results. False negative means that some people who have a negative test result actually are positive for the CFTR mutation and the mutations have not been identified. The sensitivity in genetic testing for cystic fibrosis varies among different racial and ethnic groups. The sensitivity or true positive detection rates are: Caucasians 80% to 88%, African American 65% to 69%, Ashkenazi Jewish 94% to 97%, Hispanic 57% to 72%, and Asian 30% to 49% (Goetzinger & Cahill, 2010).
Carrier screening for cystic fibrosis
To identify the carriers of this genetic mutation, genetic screening is offered to the female before conception or at the time of the first prenatal visit to her doctor. Because in the United States it is increasingly difficult to identify a single race or ethnic background, the current recommendation is to offer CF testing to all women, regardless of ethnic or racial status (Goetzinger & Cahill, 2010).
Interfering factors
NURSING CARE
Nursing actions are similar to those used in other venipuncture procedures (see Chapter 2), with the following additional measures.
Pretest
Glomerular filtration rate
Basics the nurse needs to know
GFC cannot be measured directly, but is estimated by evaluating marker clearance through the kidneys. Creatinine or insulin may be used as markers.




