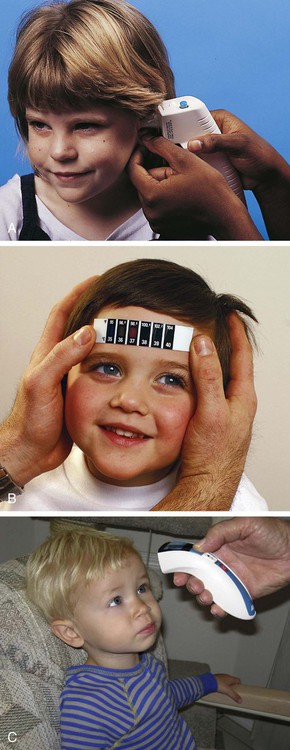
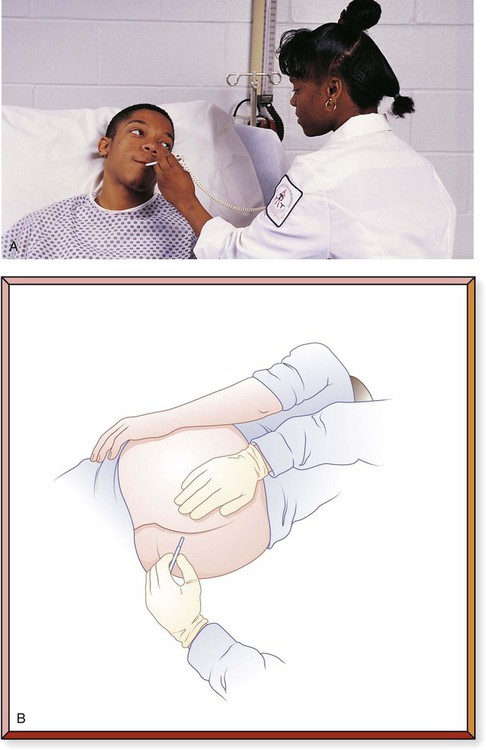
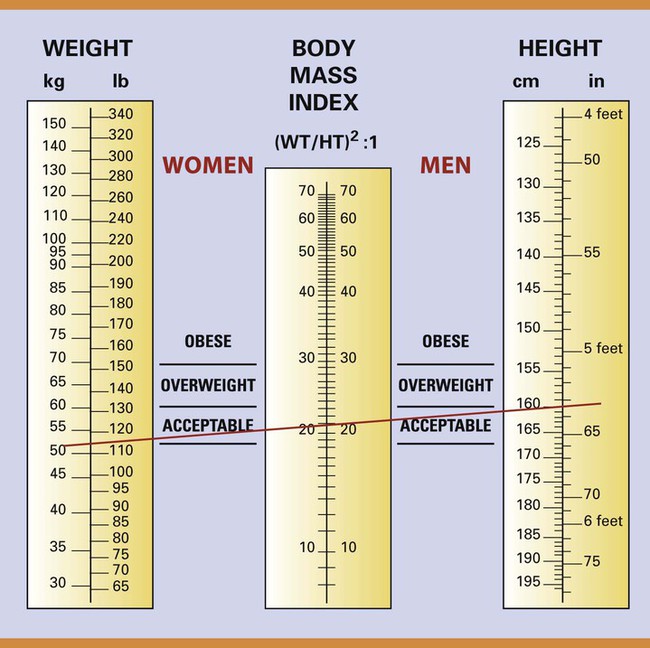
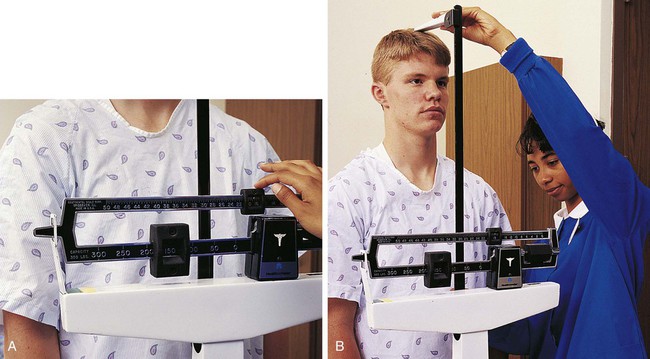
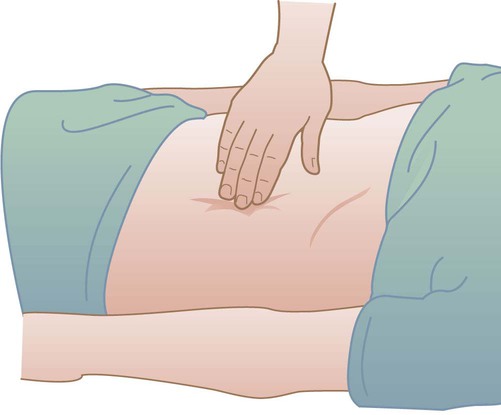
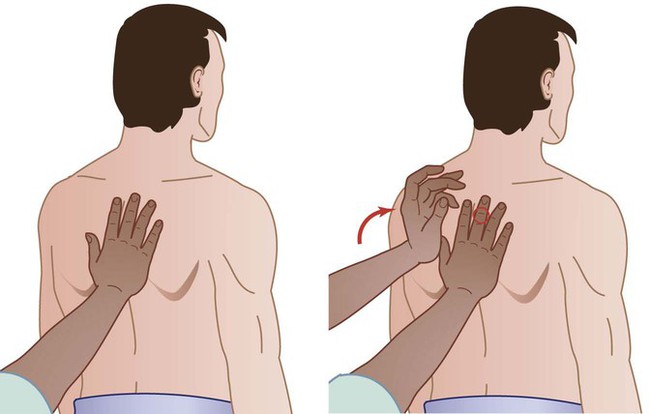
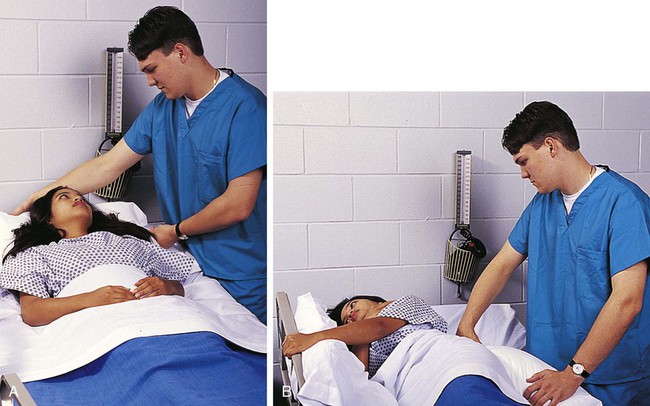
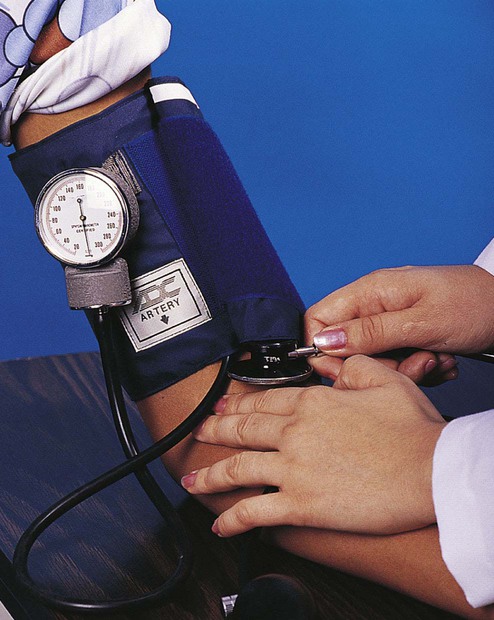
Chapter 7 The basic health assessment may include an interview and physical examination to determine functional, cultural, spiritual, and physical characteristics (Table 7-1). Basic health assessment may be the responsibility of many health care workers and is an ongoing process. The type and extent of assessment are determined by the role of the worker and the type of care being given. Some health care workers, such as the nurse assistant and licensed practical nurse, may collect data that will be analyzed and evaluated by another health care worker, such as the registered nurse. TABLE 7-1 The initial patient interview may include the health history, nature of the current complaint, and medication record. The medical or health history gathers subjective information about the patient’s health. The physical assessment uses techniques of inspection, auscultation, palpation, percussion, and smell (Table 7-2). Visual observations are used for inspection. Auscultation means listening to sounds, often with a stethoscope (Fig. 7-1). Palpation is using the hands to observe structures by touch (Fig. 7-2). Percussion is striking the body to assess the sound made (Fig. 7-3). The patient is positioned according to physician orders and for comfort during assessment (Fig. 7-4). Information that is gathered during the initial or admission health assessment is used to develop a nursing care plan (see Fig. II-3 in Appendix II on pp. 587−588). (See Skill List 7-1, Admitting, Transferring, and Discharging the Patient; and Skill List 7-2, Recording Observations, pp. 125−126). TABLE 7-2 *Odor may also be due to food eaten, medication, and hygiene practices. Blood pressure (BP) is a measurement of the force of the blood against the walls of the arteries as it circulates through the body. It reflects the effort the heart exerts to circulate the blood to the tissues. Two units or values for BP are measured: the maximum pressure at which the pulse can be heard (systolic) and the minimum pressure at which it is audible (diastolic). The systolic reading occurs while the ventricles of the heart are contracting. The diastolic reading occurs during relaxation of the ventricles. Instruments that are used to determine the blood pressure are the stethoscope and sphygmomanometer (Fig. 7-5). The stethoscope amplifies the sound. The sphygmomanometer is an inflatable cuff that uses air (aneroid) or a liquid to measure pressure. Automated cuffs may be used to measure BP using the radial artery of the wrist (Fig. 7-6). Mercury is no longer used in thermometers because of its environmental and safety risks, but sphygmomanometers containing mercury are still in use. Blood pressure varies greatly among people. It is affected by the diameter and flexibility (elasticity) of the blood vessels, force of the heart contraction, and amount of blood in the vessels. Pressure on the area of the brain that controls BP can also change its value. Limits of the usual blood pressure for most individuals have been set. “Normal” blood pressure is commonly said to be 120/80 (systolic/diastolic) (Box 7-1). The range of BP is acceptable with a systolic pressure less than 119 and a diastolic pressure less than 80. (See Skill List 7-3, Taking a Blood Pressure, pp. 126–127). Temperature is the measurement of the balance between the heat produced and lost by the body. Several methods are used to measure temperature. They include the mouth (oral), armpit (axillary), rectum (rectal), ear (temporal), and by infrared radiation (Fig. 7-7). Temperature may be measured with the Fahrenheit or Celsius (Centigrade) scale. The normal reading for temperature depends on the location used to assess it (Table 7-3). An elevation of temperature (fever) may indicate infection or inflammation in the body. TABLE 7-3 *Time required to take temperatures may vary with the electrical instruments and is usually signaled by a sound from the device. Several types of thermometers are available for measuring temperature. The most common type is made of glass with an expandable liquid filling. Glass thermometers are designed differently for oral or rectal use. The bulb of the rectal thermometer is rounded to prevent injury to the tissues of the rectum. The tip of the stem of the rectal thermometer is red, and that of the oral thermometer is blue or silver for easy identification (Fig. 7-8). Rectal thermometers should never be used in the mouth. Mercury thermometers are not commonly used because of environmental and health hazards resulting from the possibility of spilling mercury. Electronic and disposable chemical thermometers are used. (See Skill List 7-4, Taking an Oral Temperature; Skill List 7-5, Taking an Axillary Temperature; Skill List 7-6, Taking a Rectal Temperature; and Skill List 7-7, Taking an Infrared Temperature, pp. 127–130). Pulse is the heartbeat that can be felt (palpated) on surface arteries as the artery walls expand. The pulse rate is usually counted using the radial artery near the wrist, but it may be found in other locations (Fig. 7-9). The rate of the heartbeat must be adequate to supply blood and its nutrients to all parts of the body. The pulse of an infant is significantly faster than that of an adult (Table 7-4). The normal adult pulse rate can range between 60 and 100 beats per minute. In addition to the rate, it is important to assess the rhythm and character of the pulse. A regular rhythm is evenly paced. An irregular pulse may be fast or slow or may skip beats. Character, describing the force of the pulse, may be strong, weak, bounding, thready, feeble, or fleeting. (See Skill List 7-8, Taking a Radial Pulse and Measuring Respiration, p. 130). TABLE 7-4 The pulse can be counted by listening to the heart through a stethoscope placed on the chest. This pulse is called an apical pulse (Fig. 7-10). The apical pulse may differ from the radial pulse in some conditions that affect the peripheral blood flow. (See Skill List 7-8, Taking a Radial Pulse and Measuring Respiration, p. 130). One respiration includes the inspiration and expiration of a breath. The normal rate for respiration is more rapid in infants than adults (Box 7-2). The rhythm and character of respiration are important observations. The rhythm of respiration describes its regularity. Character describes the depth and quality of the sound. Respirations that are difficult to see may be assessed by feeling the rise (expansion) and fall (contraction) of the chest or by using the stethoscope to listen for the respiratory or breath sounds. Health professionals use charts that are developed by insurance companies to determine healthy weight (Fig. 7-11). The insurance companies determine at which weight for a specific height an individual is predicted to live the longest (Fig. 7-12). According to the National Heart, Lung, and Blood Institute, an ideal weight is having a body mass index between 18.7 and 24.9 (Box 7-3). More information about weight and nutrition may be found in Chapter 8. Addition and subtraction are methods for counting, resulting in a sum or difference between amounts. Multiplication and division perform addition and subtraction more quickly and result in a product or quotient. A fraction is a comparison of part of a whole to the entire unit. For example,
Foundation Skills
 Spell and define the key terms.
Spell and define the key terms.
 Describe the elements of basic health assessment.
Describe the elements of basic health assessment.
 Identify normal and abnormal vital sign values.
Identify normal and abnormal vital sign values.
 Describe the importance of the values for normal vital signs.
Describe the importance of the values for normal vital signs.
 Perform basic mathematical skills related to health care.
Perform basic mathematical skills related to health care.
 Use basic medical terminology and abbreviations.
Use basic medical terminology and abbreviations.
Health Assessment
Patient Interview and Examination
Assessment
Observations
Appearance
Physical, developmental, social development; general health; significant features; height, weight, posture; communication skills; grooming and hygiene
Hair
Color, texture, cleanliness, distribution
Nails
Color, texture, markings, shape, size
Skin
Color, temperature, turgor, lesions, mucous membranes, injury, edema
Neurological
Pupil reaction to light; motor and verbal responses; reflexes, gait, orientation
Musculoskeletal
Range of motion, gait, posture, injury
Cardiovascular
Heart rate and rhythm, peripheral pulses, temperature
Respiratory
Rate, rhythm, quality, breath sounds, sputum production or cough
Gastrointestinal
Abdominal contour, bowel sounds, nausea or vomiting, defecation frequency and consistency
Genitourinary
Urine color, amount, frequency, odor, clarity
Area
Smell
Possible Cause
Mouth
Alcohol
Drinking alcohol
Bad breath (halitosis)
Poor dental hygiene, gum disease
Fruity, sweet
Diabetes acidosis, medication
Feces
Intestinal obstruction
Acid breath
Peptic ulcer
Rotten eggs, garlic
Cirrhosis, medication
Ammonia
Kidney failure
Rectal area
Feces
Incontinence
Skin (under arms and breasts)
Foul, body odor
Poor hygiene, excessive sweating
Stale urine
Uremic acidosis
Skin (under cast)
Musty
Infection
Tracheostomy
Sweet, fetid
Bacterial infection (pseudomonas)
Urine
Ammonia
Urinary tract infection
Foul
Urinary tract infection
Vomit
Feces
Bowel obstruction
Wound site
Feces
Abscess
Sweet, heavy
Bacterial infection (pseudomonas)
Blood Pressure
Temperature
Method
Time
Normal
Oral
3 min*
97.6°-99.0° F
(98.6° F = 37.0° C)
Axillary
10 min*
96.6°-98.0° F
(97.6° F = 36.4° C)
Rectal
3-5 min*
98.6°-100.0° F
(99.6° F = 37.5° C)
Temporal
*
96.4°-100.4° F
(98.4° F = 36.9° C)
Infrared
*
97.6°-99.0° F
(98.6° F = 37.0° C)
Pulse and Respiration
Age Group
Normal Pulse Rates (Beats/Min)
Abnormal Pulse Rates (Beats/Min)
Newborn
70-170
Infant
80-130
School age
70-110
Adult
60-100
<60 (bradycardia)
>100 (tachycardia)

Height and Weight
Information Exchange
Basic Math
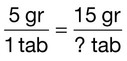
 indicates that the quantity being considered is 1 of 4 equal parts of the whole. Fractions may be “reduced” by dividing the top number (numerator) and bottom number (denominator) by the same number. For example,
indicates that the quantity being considered is 1 of 4 equal parts of the whole. Fractions may be “reduced” by dividing the top number (numerator) and bottom number (denominator) by the same number. For example,  is equal to
is equal to  . In health care, fractions or ratios often are used to calculate medications, determine temperature, or determine a schedule for the patient’s care (Box 7-4).
. In health care, fractions or ratios often are used to calculate medications, determine temperature, or determine a schedule for the patient’s care (Box 7-4).




 Normal value
Normal value Prehypertension
Prehypertension High
High