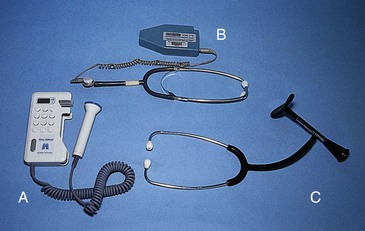
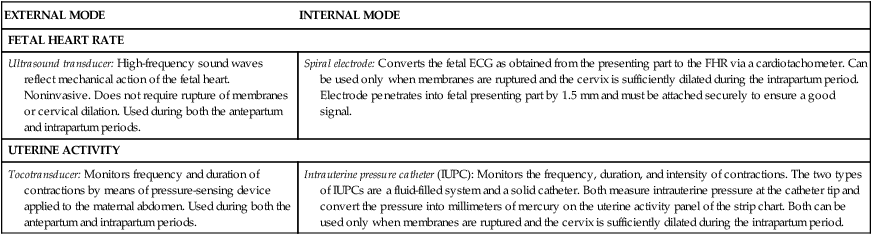
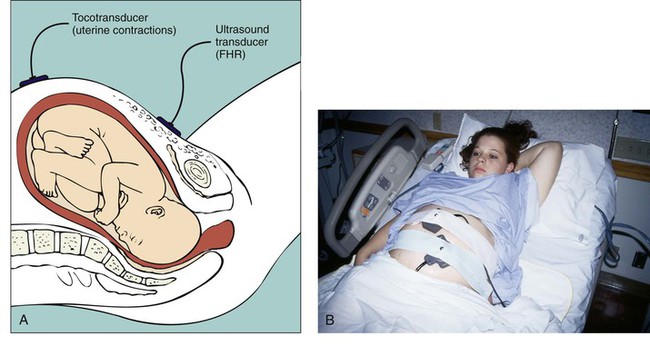
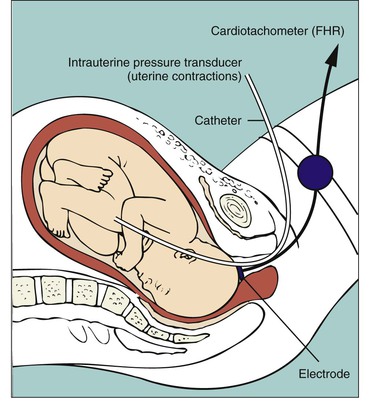
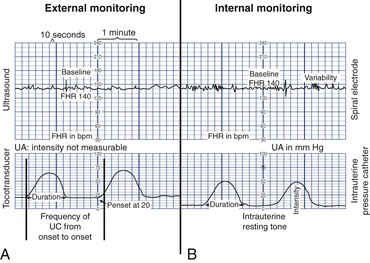
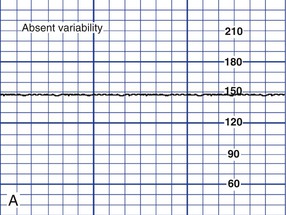
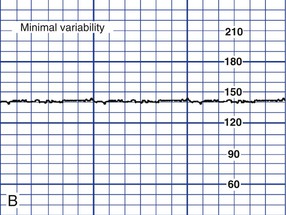
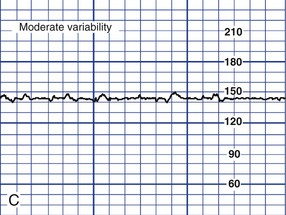
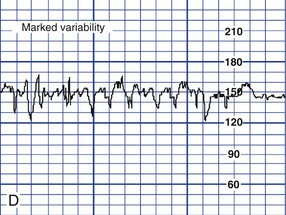
• Identify typical signs of normal (reassuring) and abnormal (nonreassuring) fetal heart rate (FHR) patterns. • Compare FHR monitoring performed by intermittent auscultation with external and internal electronic methods. • Explain the baseline FHR and evaluate periodic changes. • Describe nursing measures that can be used to maintain FHR patterns within normal limits. • Differentiate among the nursing interventions used for managing specific FHR patterns, including tachycardia and bradycardia, absent or minimal variability, and late and variable decelerations. • Review the documentation of the monitoring process necessary during labor. Additional related content can be found on the companion website at http://evolve.elsevier.com/Lowdermilk/Maternity/ • Critical Thinking Exercise: Fetal Monitoring • Nursing Care Plan: Electronic Fetal Monitoring during Labor T he ability to assess the fetus by auscultation of the fetal heart was initially described more than 300 years ago. With the advent of the fetoscope and stethoscope after the turn of the twentieth century the listener could hear clearly enough to count the fetal heart rate (FHR). When electronic FHR monitoring made its debut for clinical use in the early 1970s, the anticipation was that its use would result in fewer cases of cerebral palsy and be more sensitive than stethoscopic auscultation in predicting and preventing fetal compromise (Garite, 2007). Consequently, the use of electronic fetal monitoring rapidly expanded. However, the rate of cerebral palsy has risen slightly since that time and is not likely to improve (Gilbert, 2007). Moreover, in 2006 the cesarean birth rate in the United States reached an all-time high of 31.1% (Collard, Diallo, Habinsky, Hentschell, & Vezeau, 2008/2009). Still, electronic fetal monitoring (EFM) is a useful tool for visualizing FHR patterns on a monitor screen or printed tracing and continues to be the primary mode of intrapartum fetal assessment. Currently in the United States, approximately 85% of women giving birth have continuous EFM during labor, making it the most commonly performed obstetric procedure (American College of Obstetricians and Gynecologists [ACOG], 2009; Tucker, Miller, & Miller, 2009). Pregnant women should be informed about the equipment and procedures used and the risks, benefits, and limitations of intermittent auscultation (IA) and EFM. This chapter discusses the basis for intrapartum fetal monitoring, the types of monitoring, and nursing assessment and management of abnormal fetal status. • Reduction of blood flow through the maternal vessels as a result of maternal hypertension (chronic hypertension, preeclampsia, or gestational hypertension), hypotension (caused by supine maternal position, hemorrhage, or epidural analgesia or anesthesia), or hypovolemia (caused by hemorrhage) • Reduction of the oxygen content in the maternal blood as a result of hemorrhage or severe anemia • Alterations in fetal circulation, occurring with compression of the umbilical cord (transient, during uterine contractions [UCs], or prolonged, resulting from cord prolapse), placental separation or complete abruption, or head compression (head compression causes increased intracranial pressure and vagal nerve stimulation with an accompanying decrease in the FHR) • Reduction in blood flow to the intervillous space in the placenta secondary to uterine hypertonus (generally caused by excessive exogenous oxytocin) or secondary to deterioration of the placental vasculature associated with maternal disorders such as hypertension or diabetes mellitus Fetal well-being during labor can be measured by the response of the FHR to UCs. A group of fetal monitoring experts have recently recommended that FHR tracings that demonstrate the following characteristics be described as normal (Macones, Hankins, Spong, Hauth, & Moore, 2008): • A baseline FHR rate of 110 to 160 beats/min • Moderate baseline FHR variability • Late or variable decelerations absent • Early decelerations present or absent Table 11-1 describes normal uterine activity (UA) during labor. TABLE 11-1 Normal Uterine Activity during Labor Source: Tucker, S. M., Miller, L. A, & Miller, D. A. (2009). Mosby’s pocket guide to fetal monitoring: A multidisciplinary approach (6th ed.). St. Louis: Mosby. The goals of intrapartum FHR monitoring are to identify and differentiate the normal (reassuring) patterns from the abnormal (nonreassuring) patterns, which can be indicative of fetal compromise. Although the 2008 National Institute of Child Health and Human Development workshop (Macones et al., 2008) and a recent ACOG Practice Bulletin (2009) both recommend use of the terms normal and abnormal to describe FHR tracings, the terms reassuring and nonreassuring are still frequently used clinically. Abnormal FHR patterns are those associated with fetal hypoxemia, which is a deficiency of oxygen in the arterial blood. If uncorrected, hypoxemia can deteriorate to severe fetal hypoxia, which is an inadequate supply of oxygen at the cellular level. Examples of abnormal FHR patterns include the following (Macones et al., 2008). Absent baseline FHR variability and any of the following: The ideal method of fetal assessment during labor continues to be debated. When performed at prescribed intervals, especially during and immediately after contractions, IA has been shown to be as valuable as EFM at predicting fetal outcomes (Gilbert, 2007). Intermittent auscultation (IA) involves listening to fetal heart sounds at periodic intervals to assess the FHR. IA of the fetal heart can be performed with a Pinard stethoscope, a Doppler ultrasound device (Fig.11-1, A) an ultrasound stethoscope (Fig. 11-1, B) or a DeLee-Hillis fetoscope (Fig. 11-1, C). The fetoscope is applied to the listener’s forehead because bone conduction amplifies the fetal heart sounds for counting. The Doppler ultrasound device and ultrasound stethoscope transmit ultrahigh-frequency sound waves reflecting movement of the fetal heart and convert these sounds into an electronic signal that can be counted. Box 11-1 describes how to perform IA. IA is easy to use, inexpensive, and less invasive than EFM. It is often more comfortable for the woman and gives her more freedom of movement. Other care measures, such as ambulation and the use of baths or showers, are easier to carry out when IA is used. On the other hand, IA may be difficult to perform in women who are obese. Because IA is intermittent, significant events may occur during a time when the FHR is not auscultated. Also, IA does not provide a permanent documented visual record of the FHR and cannot be used to assess visual patterns of the FHR variability or periodic changes (Albers, 2007; Tucker et al., 2009). By using IA the nurse can assess the baseline FHR, rhythm, and increases and decreases from baseline. The recommended optimal frequency for IA in low risk women during labor has not been determined (Nageotte & Gilstrap, 2009). The purpose of electronic FHR monitoring is the ongoing assessment of fetal oxygenation. The goal is to detect fetal hypoxia and metabolic acidosis during labor so that interventions to resolve the problem can be implemented in a timely manner before permanent damage or death occur (Garite, 2007). The two modes of EFM include the external mode, which uses external transducers placed on the maternal abdomen to assess FHR and UA, and the internal mode, which uses a spiral electrode applied to the fetal presenting part to assess the FHR and an intrauterine pressure catheter (IUPC) to assess UA and pressure. The differences between the external and internal modes of EFM are summarized in Table 11-2. TABLE 11-2 External and Internal Modes of Monitoring Separate transducers are used to monitor the FHR and UCs (Fig. 11-2). The ultrasound transducer works by reflecting high-frequency sound waves off a moving interface: in this case the fetal heart and valves. Reproducing a continuous and precise record of the FHR is sometimes difficult because of artifacts introduced by fetal and maternal movement. The FHR is printed on specially formatted monitor paper. The standard paper speed used in the United States is 3 cm/min. Once the area of maximal intensity of the FHR has been located, conductive gel is applied to the surface of the ultrasound transducer, and the transducer is then positioned over this area and held securely in place using an elastic belt. The tocotransducer (tocodynamometer) measures UA transabdominally. The device is placed over the uterine fundus and held securely in place using an elastic belt (see Fig. 11-2). UCs or fetal movements depress a pressure-sensitive surface on the side next to the abdomen. The tocotransducer can measure and record the frequency and approximate duration of UCs but not their intensity. This method is especially valuable for measuring UA during the first stage of labor in women with intact membranes or for antepartum testing. Because the tocotransducer of most electronic fetal monitors is designed for assessing UA in the term pregnancy, it may not be sensitive enough to detect preterm UA. When monitoring the woman in preterm labor, remember that the fundus may be located below the level of the umbilicus. The nurse may need to rely on the woman to indicate when UA is occurring and to use palpation as an additional way of assessing contraction frequency and validating the monitor tracing. The external transducer is easily applied by the nurse, but it must be repositioned as the woman or fetus changes position (see Fig. 11-2, B). The woman is asked to assume a semi-sitting or a lateral position. Use of an external transducer confines the woman to bed. Portable telemetry monitors allow observation of the FHR and UC patterns by means of centrally located electronic display stations. These portable units permit the woman to walk around during electronic monitoring. The technique of continuous internal FHR or UA monitoring allows a more accurate appraisal of fetal well-being during labor than external monitoring because it is not interrupted by fetal or maternal movement or affected by maternal size (Fig. 11-3). For this type of monitoring the membranes must be ruptured and the cervix sufficiently dilated (at least 2-3 cm) to allow placement of the spiral electrode or IUPC or both. Internal and external modes of monitoring may be combined (i.e., internal FHR with external UA or external FHR with internal UA) without difficulty. The FHR and UA are displayed on the monitor paper, with the FHR in the upper section and UA in the lower section. Fig. 11-4 contrasts the internal and external modes of electronic monitoring. Note that each small square on the monitor paper or screen represents 10 seconds; each larger box of six squares equals 1 minute (when paper is moving through the monitor at the rate of 3 cm/min). Characteristic FHR patterns are associated with fetal and maternal physiologic processes and have been identified for many years. Because EFM was introduced into clinical practice before consensus was reached in regard to standardized terminology, however, variations in the description and interpretation of common fetal heart rate patterns were often great. In 1997 the National Institute of Child Health and Human Development (NICHD) published a proposed nomenclature system for EFM interpretation with standardized definitions for FHR monitoring. The NICHD recommendations were not widely incorporated into clinical practice, however, until they were endorsed by the American College of Obstetricians and Gynecologists (ACOG) in 2005. Shortly thereafter, use of the NICHD standard terminology was also endorsed by the Association of Women’s Health, Obstetric, and Neonatal Nurses (AWHONN), and the American College of Nurse-Midwives (ACNM) (Tucker et al., 2009). All three organizations cited concerns regarding patient safety and the need for improved communication among caregivers as reasons for using standard EFM definitions in clinical practice. In April 2008 the NICHD, ACOG, and the Society for Maternal-Fetal Medicine partnered to sponsor another workshop to revisit the FHR definitions recommended by the NICHD in 1997. The 1997 FHR definitions were reaffirmed at this workshop. In addition, new definitions related to UA were recommended, as well as a three-tier system of FHR pattern interpretation and categorization (Macones et al., 2008). ACOG (2009) has recently published a practice bulletin which supports use of the 2008 NICHD workshop recommendations. The baseline fetal heart rate is the average rate during a 10-minute segment that excludes periodic or episodic changes, periods of marked variability, and segments of the baseline that differ by more than 25 beats/min (Macones et al., 2008). The normal range at term is 110 to 160 beats/min. The baseline rate is documented as a single number, rather than a range (Tucker et al., 2009). Variability of the FHR can be described as irregular waves or fluctuations in the baseline FHR of two cycles per minute or greater (Macones, et al., 2008). It is a characteristic of the baseline FHR and does not include accelerations or decelerations of the FHR. Variability is quantified in beats per minute and is measured from the peak to the trough of a single cycle. Four possible categories of variability have been identified: absent, minimal, moderate, and marked (Fig. 11-5). In the past, variability was described as either long term or short term (beat to beat). The NICHD definitions do not distinguish between long- and short-term variability, however, because in actual practice, they are visually determined as a unit (NICHD, 1997).
Fetal Assessment during Labor
Web Resources
![]()
Basis for Monitoring

Fetal Response
Uterine Activity
CHARACTERISTIC
DESCRIPTION
Frequency
Contraction frequency overall generally ranges from two to five per 10 minutes during labor, with lower frequencies seen in the first stage of labor and higher frequencies (up to five contractions in 10 minutes) seen during the second stage of labor.
Duration
Contraction duration remains fairly stable throughout the first and second stages, ranging from 45-80 seconds, not generally exceeding 90 seconds.
Intensity (peak less resting tone)
Intensity of uterine contractions generally range from 25-50 mm Hg in the first stage of labor and may rise to over 80 mm Hg in second stage. Contractions palpated as “mild” would likely peak at less than 50 mm Hg if measured internally, whereas contractions palpated as “moderate” or greater would likely peak at 50 mm Hg or greater if measured internally.
Resting tone
Average resting tone during labor is 10 mm Hg; if using palpation, should palpate as “soft” (i.e., easily indented, no palpable resistance).
Montevideo units (MVUs)
Ranges from 100-250 MVUs in the first stage, may rise to 300-400 in the second stage. Contraction intensities of 40 mm Hg or more and MVUs of 80-120 are generally sufficient to initiate spontaneous labor.
Fetal Compromise
Monitoring Techniques

Intermittent Auscultation
Electronic Fetal Monitoring
EXTERNAL MODE
INTERNAL MODE
FETAL HEART RATE
Ultrasound transducer: High-frequency sound waves reflect mechanical action of the fetal heart. Noninvasive. Does not require rupture of membranes or cervical dilation. Used during both the antepartum and intrapartum periods.
Spiral electrode: Converts the fetal ECG as obtained from the presenting part to the FHR via a cardiotachometer. Can be used only when membranes are ruptured and the cervix is sufficiently dilated during the intrapartum period. Electrode penetrates into fetal presenting part by 1.5 mm and must be attached securely to ensure a good signal.
UTERINE ACTIVITY
Tocotransducer: Monitors frequency and duration of contractions by means of pressure-sensing device applied to the maternal abdomen. Used during both the antepartum and intrapartum periods.
Intrauterine pressure catheter (IUPC): Monitors the frequency, duration, and intensity of contractions. The two types of IUPCs are a fluid-filled system and a solid catheter. Both measure intrauterine pressure at the catheter tip and convert the pressure into millimeters of mercury on the uterine activity panel of the strip chart. Both can be used only when membranes are ruptured and the cervix is sufficiently dilated during the intrapartum period.
External monitoring
Internal monitoring
Fetal Heart Rate Patterns

Baseline Fetal Heart Rate
Variability
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Fetal Assessment during Labor
Get Clinical Tree app for offline access
