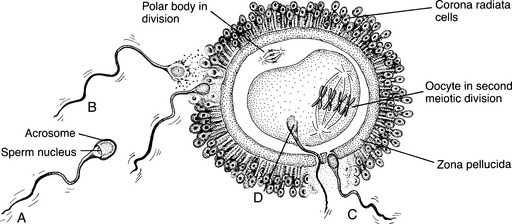
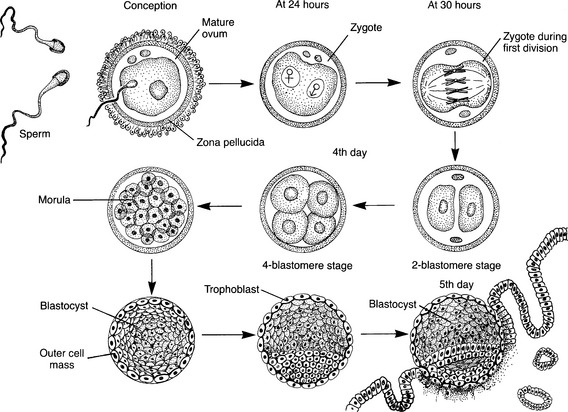
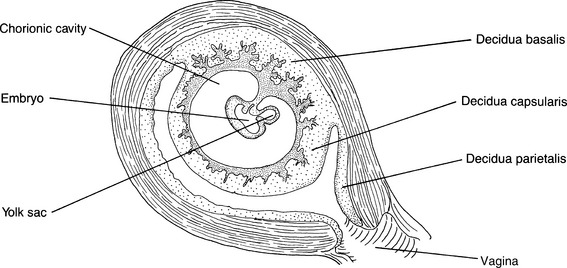
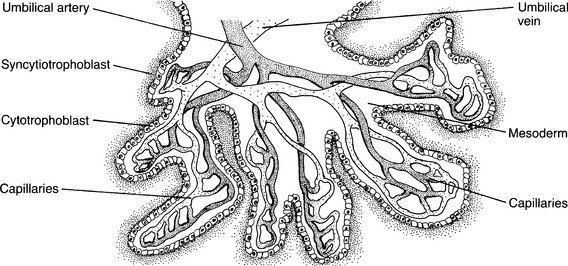
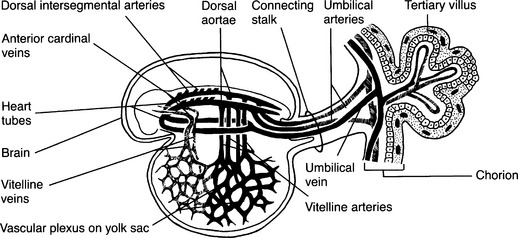
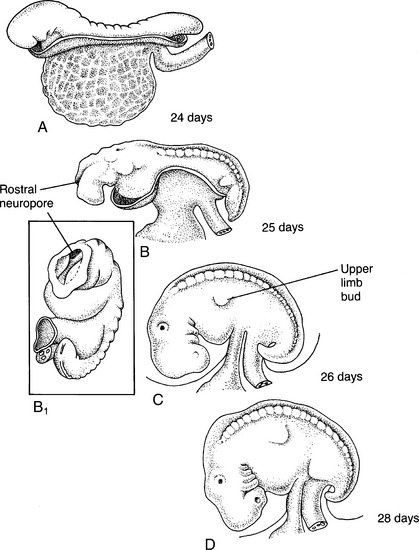
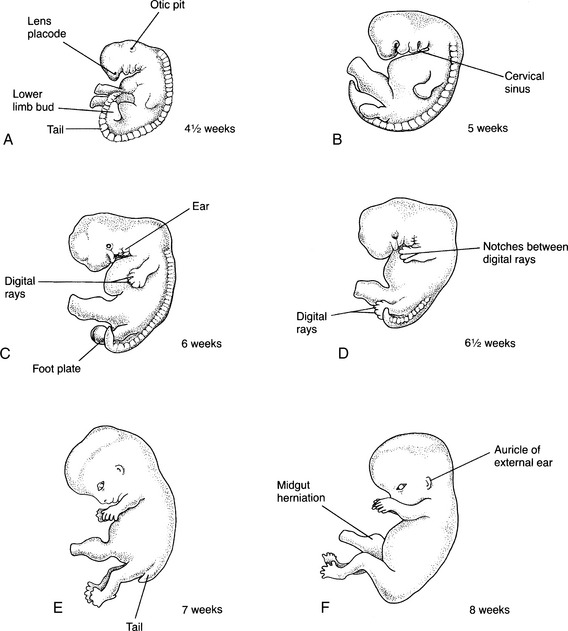
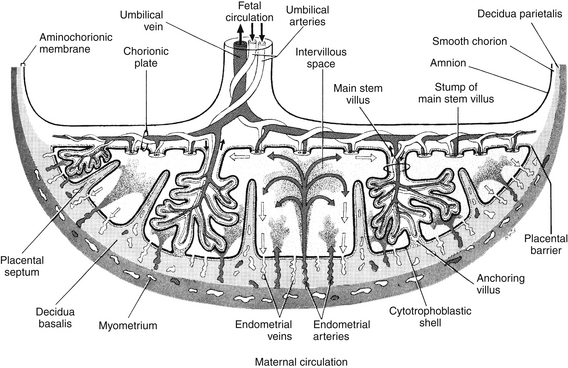
CHAPTER 3 1 Describe the process of fertilization. 2 Discuss the stages of placental development. 3 Describe the functions of the placenta. 4 Explain the implications of ineffective placental development on fetal development. 5 Describe the functions of the amniotic fluid. 6 Identify the important milestones for the development of fetal organs, such as the heart, lungs, kidney, and brain. 7 Identify the periods when the developing body systems of the fetus are most susceptible to teratogenic influences. 1. Encompasses the time after formation of the germ cells and before union of sperm and egg 2. Begins with differentiation and migration of primitive germ cells to the genital ridge and ends with the formation of the gametes (karyogamy) 3. Aneuploidies (abnormal numbers of chromosomes) might occur as a consequence of abnormal meiotic division of chromosomes during gamete formation. 1. Fertilization usually occurs in the ampulla of the fallopian tube. 2. Estrogen levels increase during ovulation, aiding fertilization and easing transit of the ovum down the fallopian tube. 3. The ovum membrane is surrounded by two layers of tissue. a. An inner layer called the zona pellucida b. An outer layer called the corona radiata (Figure 3-1) 4. In a single ejaculation, 400 million spermatozoa are deposited in the vagina, reaching the fallopian tubes within 5 minutes by frantic movement of their flagellar tails. a. A sperm undergoes two processes before it is able to penetrate the ovum. (1) Capacitation: structural changes occur once in the female genital tract. (2) Acrosomal reaction: the sperm releases enzymes (see Figure 3-1). b. Ova are considered fertile for approximately 24 hours after ovulation, whereas sperm, although viable for 72 hours, are believed to be fertile for only 24 hours. c. At the moment of penetration, the oocyte completes the second meiotic division (see Figure 3-1), whereas cellular changes prevent other sperm from entering the ovum (zona reaction). 5. With fertilization, the diploid number (46) of chromosomes is restored, and cell division begins. C Pre-embryonic stage: The first 2 weeks after fertilization; the blastogenetic period is the first 4 weeks of human development 1. This stage is characterized by rapid cell division, cell differentiation, and the development of embryonic membranes and germ layers. (1) Division of the zygote occurs within the first 30 hours. (2) The zygote continues to divide into a solid ball of cells (the morula). (3) The morula floats inside of the uterus for 2 or 3 days obtaining nourishment from the mucous lining of the uterus and the fluid in the uterine cavity. (4) Two distinct layers of cells develop as the morula hollows out. (a) The inner cell mass (blastocyst), which will form the embryo, the amnion, and the yolk sac membrane (b) The outer cell layer (trophoblast), which becomes the fetal side of the placenta and chorion (5) Zona pellucida disappears at about 5 days. (6) The attached portion of the trophoblast develops into two layers. (a) The internal cellular layer is called the cytotrophoblast. (b) The outer layer is called the syncytiotrophoblast, which invades the endometrial epithelium by the end of the 7th day. (c) Embedding is completed by the 11th day, with the site of attachment usually being the upper part of the posterior uterine wall. Attachment can occur anywhere, even extrauterine. (1) The inner cell mass differentiates into two cell layers: the endoderm (the inside of the embryo) and the ectoderm (the outside of the embryo). (a) The amniotic cavity appears as a space between the inner cell mass and the trophoblast. (b) When the embryo becomes a cylinder, the amnion surrounds it and forms the amniotic sac. (2) By the end of the second week, the embryonic cells and the amniotic and yolk sacs are attached to the chorionic sac by a slender band, which becomes the umbilical cord. (3) Malformations that occur during the pre-embryonic stage seldom result in a viable fetus. (1) Description: the placenta is a temporary disk-shaped organ that connects the fetus to the uterine wall and provides for fetal respiration as well as metabolic and nutrient exchanges between the maternal and fetal circulations. (2) Approximately 5 to 6 days after fertilization, the blastocyst adheres to the endometrium. (3) Blastocyst penetrates toward the maternal capillaries by eroding the uterine epithelium; this erosion process continues until the blastocyst is completely embedded in the uterine wall. d. Decidua: the portion of the endometrium enveloping the developing fertilized ovum (Figure 3-3) (1) On approximately the 14th day, the endometrium changes at the site of implantation and becomes the decidua. (2) Implantation causes the adjacent decidual cells to engorge with glycogen and lipids (decidual reaction). (3) The swollen decidual cells release their contents during the erosion process to provide nourishment to the embryo. (4) The decidua divides into three layers: (1) When the embryoblast is partially embedded in the decidua, two distinct layers of cells can be seen in the trophoblast. (a) Inner layer (cytotrophoblast) is made of mononuclear cells. (b) Outer layer (syncytiotrophoblast) consists of multinucleated cells and is responsible for the erosive ability of the trophoblast. (2) The cytotrophoblast and the syncytiotrophoblast separate the maternal and fetal circulations and are called the placental barrier. (3) On approximately the 9th day, spaces (vacuoles) appear in the syncytium; these fuse together to form lacunae (intervillous spaces), which develop into an interconnecting system. (4) On approximately the 11th day: (a) Invading syncytium encounters the congested capillaries of the decidua. (b) Syncytium enzymes break down the vessel walls, releasing blood into the lacunae. (c) Eventually the syncytium encounters the larger arteries and veins and establishes a directional flow of blood. (5) Chorionic villi develop between the 9th and 25th days (Figure 3-4). (a) The chorion (trophoblastic cells) is the first placental membrane to form, enclosing the embryo, amnion, and yolk sac and growing outward, forming finger-like projections called villi within which blood vessels develop. (b) Initially the chorion covers the whole chorionic surface, but with fetal growth the intraluminal villi become compressed and degenerate. (c) Villi located below the embryo continue to grow, forming a large surface for exchange with villi that contact the decidua basalis to become anchoring villi. [i] Decidual septa form between anchoring villi, which results in 15 to 20 lobes (cotyledons). [ii] Exchange of gases and nutrients occurs in this vascular system. (d) Other villi float free and conduct most of the exchange between mother and developing fetus. D Embryonic stage: Begins with the folding of the disk in week 2 of development (1) The embryonic disk converts into a trilaminar embryonic disk comprising three germ layers: ectoderm (to become the epidermis and the nervous system); mesoderm (to become the smooth muscle); and endoderm (to become the epithelial lining of the respiratory and digestive tracts). (2) The process is completed in the third week with the formation of intraembryonic mesoderm by the primitive streak. b. Proliferation and migration of cells from the primitive streak give rise to mesenchyme (1) Cells spread cranially and caudally. (2) Cells begin to form the embryonic endoderm, which gives rise to the lining of the digestive and respiratory tracts. (3) The cells that remain on the surface of the embryonic disk form the layer of cells called the embryonic ectoderm, which develop into the nervous system (i.e., the sensory epithelium of the eye, ear, and nose). c. The mesenchymal cells migrate cephalad under the embryonic ectoderm and form the notochordal process. (1) These cells grow until they reach the prochordal plate, the future site of the mouth. (2) Caudal to the primitive streak is a circular area called the cloacal membrane, which becomes the anus. (3) The primitive streak continues to form mesoderm until the end of the fourth week. (4) The notochord develops by transformation of the notochordal process by the end of the third week of gestation. d. Neurulation is the process of developing the neural plate, neural folds, and neural tube. (a) Embryonic ectoderm lying over the notochord thickens to form the neural plate. (b) It first appears near the primitive knot and enlarges to form a neural groove, which becomes bounded by the neural folds on each side. (a) By the third week the neural folds begin to fuse, forming the neural tube. (b) This occurs near the middle of the embryo and progresses toward the cranial and caudal ends. (a) Cells lying along the neural fold migrate ventrolaterally on each side of the neural tube forming an irregular mass called the neural crest. (b) These cells migrate throughout the embryo and give rise to the spinal ganglia. (c) The neural crest cells also form the meninges of the brain and spinal cord, the adrenal medulla, and several components of the skeletal and muscular parts of the head. (1) Some of the mesoderm forms columns that divide into paired cuboidal bodies (somites). (2) Mesenchymal cells from the somites will become the vertebral column, the ribs, the sternum, the skull, and associated muscles. (1) Cavities in the lateral mesoderm form a horseshoe-shaped cavity called the intraembryonic coelom. (2) The intraembryonic coelom divides the lateral mesoderm into two layers. (a) Somatic layer is continuous with the extraembryonic mesoderm covering the amnion. (b) Visceral layer is continuous with the extraembryonic mesoderm covering the yolk sac. (3) During the second month the intraembryonic coelom will become the pericardial, the pleural, and the peritoneal cavities. g. Primitive cardiovascular system (Figure 3-5) (1) Blood vessels start forming in the extraembryonic mesoderm of the yolk sac, connecting stalk and chorion at the end of the third week. (2) Mesenchymal cells (angioblasts) aggregate to form blood islands. (3) Mesenchymal cells arrange around cavities in the blood islands to form the endothelium of primitive blood vessels, which go on to develop into a series of vascular networks. (4) Primitive blood cells develop from the endothelial cells of the vessels in the walls of the yolk sac; blood formation does not begin in the embryo until the fifth week. (5) The primitive heart is a tubular structure formed from the mesenchymal cells in the cardiogenic area. (a) Paired endocardial heart tubes develop and fuse to form a primitive heart. (b) The heart tubes join blood vessels in the embryo, connective stalk, chorion, and yolk sac, forming a primitive cardiovascular system. (c) The primitive blood cells begin to circulate at the end of the third week as the tubular heart begins to beat. h. Malformations that might occur during this stage: (1) Anencephaly, as a result of a defect in the closure of the anterior neural tube, which results in the degeneration of the forebrain (2) Cyclopia, as a result of an alteration in the prechordal mesodermal development, and producing secondary defects of the midface and forebrain (3) Ectromelia (congenital absence of a limb) (4) Ectopia cordis (heart remains outside of the thoracic cavity) a. The neural tube is open at the rostral and caudal neuropores, and the embryo is almost straight (Figure 3-6, A and B). b. The first and second pairs of the branchial arches (future head and neck) are visible. c. The otic placodes (primordia of the internal ears) are developed. d. By the middle of the fourth week, the embryo is cylindric and curved because of the folding of the median and horizontal planes. (1) The rostral neuropore closes. (2) The upper limb buds appear as small swellings on the lateral wall (see Figure 3-6, C). (3) The heart is a distinct prominence on the surface of the embryo. e. By the end of the fourth week, the embryo is C-shaped. (1) The oral cavity begins while the esophagotracheal septum begins to divide into the esophagus and the trachea. (2) The stomach, the pancreas, and the liver begin to form. (3) Upper limb buds have a flipper shape (see Figure 3-6, D). (4) Lower limb buds appear as small swellings (Figure 3-7, A). (5) Four pairs of branchial arches and lens placodes (the lens of the eye) have developed. f. Malformations that might occur during this stage of development: (1) Myelomeningocele results from a defect in the closure of the posterior neural tube. (2) Esophageal atresia and tracheoesophageal fistulas can occur as a result of the lateral septation of the foregut. (3) Extravasation of the bladder occurs if the infraumbilical mesenchyme does not migrate effectively. 3. Fifth week (see Figure 3-7, B) a. The embryo is approximately 8 mm ( b. The head grows because of the rapid development and differentiation of the brain. c. The cranial nerves have developed. d. Atrial division in the heart begins. e. Upper limbs become paddle-shaped. f. Malformations can occur during this stage. 4. Sixth week (see Figure 3-7, C and D) a. The embryo is 12 mm (½ inch) long. b. The fissures of the brain are obvious. c. The heart begins to divide into chambers, and the liver begins to form red blood cells. d. The trachea and lung buds appear, and the oral and nasal cavities are formed. e. The upper and lower jaw begin to form; upper lip and palate development also occur. f. Embryonic sex glands appear. g. Skeletal and muscular systems (1) Ossification of the jaw and skull begins. (2) The wrist and elbow are identifiable. (3) Ridges called digital rays (future fingers and thumb) form on the paddle-shaped hands. h. The primordia of the external acoustic meatus and external ear are present; the external, middle, and inner ears continue to form. i. Malformations can occur during this period. (1) Rectal atresia with fistula occurs if there is a defect in the lateral septation of the cloaca into the rectum and urogenital sinuses. (2) Diaphragmatic hernia occurs when there is a defect in the closure of the pleuroperitoneal canal. (3) Ventricular septal defect results during the closure of the ventricular septum. 5. Seventh week (see Figure 3- 7, E) a. The embryo is approximately 18 mm (3⁄4 inch) long. b. Fetal heartbeat can be heard and fetal circulation begins. (1) The tongue separates, and the palate begins to fold inward. (2) The stomach assumes its final shape. (3) The diaphragm separates the abdominal and thoracic cavities. (1) The bladder and the urethra separate from the rectum. (2) The sex glands begin to differentiate into testes or ovaries. e. Skeletal and muscular systems f. The optic nerve forms, the eyelids appear, and the eye lenses begin to thicken. g. Malformations that can occur during this period: 6. Eighth week (see Figure 3-7, F) a. The embryo is 2.5 to 3 cm (1 inch) long and weighs 8 g (0.25 ounce). b. Sensory and motor neurons have functional connections, and the embryo is able to contract large muscles. c. Development of the heart is complete, and the circulatory system through the umbilical cord is formed. (1) Abdomen protrudes because the intestines are in the proximal part of the umbilical cord. (2) Anal membrane perforates, and rectal passage opens. e. External genitalia begin to differentiate. f. Skeletal and muscular systems (1) Distinct notches are present between the toes. (2) The fingers and toes are distinct and separated. (3) Differentiation of the cells occurs in the primitive skeleton. (4) Cartilaginous bones begin to ossify. (5) Muscle development begins in the trunk, limbs, and head. g. The eyes are open but fuse at the end of the eighth week, and the auricles of the external ear assume their final appearance. h. Malformations that can occur during this period: E Fetal stage: Every organ system and external structure is present, and the remainder of gestation is devoted to refining the function of the organs 1. Placental growth continues until the 20th week; beyond 20 weeks the placenta increases only in thickness. (1) Placenta is round and flat; approximately 15 to 20 cm (6 to 8 inches) in diameter and 2.5 cm (1 inch) thick. (2) Placenta weighs approximately one sixth of the weight of the infant. (3) Maternal surface (red and blue) (4) Fetal surface (smooth, white, and shiny in appearance):
Fetal and Placental Development and Functioning
INTRODUCTION
 inch) long.
inch) long.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree