Facilitation of skills related to childbearing
Cusco speculum use
Learning outcomes
Having read this chapter, the reader should be able to:
A Cusco speculum is a medical instrument that is inserted into the vagina for access to the top of the vagina and cervix. For the woman this may be an uncomfortable and embarrassing procedure; thus it is important that the midwife undertakes this sensitively and correctly.
Indications
The midwife may need to use a Cusco speculum:
Cusco speculum
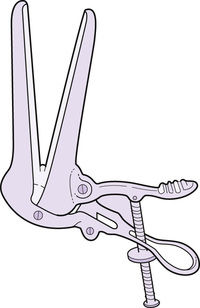
The Cusco speculum is made of metal (reusable) or plastic (single use, disposable) and usually comes in three sizes – small, medium, and large. It has two short hinged blades that are curved across their width to give a duckbill shape (Fig. 28.1). The blades are close together when the speculum is closed, but when open they separate and press against the vaginal walls. At one end there is a circular opening through which the vagina and cervix can be visualized and swabs inserted when required. Attached to this are the handles that open and close the speculum using a screw mechanism. When the handles are apart the blades are closer together and as the handles are brought closer together the blades open. It is worth practising the opening and closing of the blades a few times before inserting it to ensure familiarity with how it works.
Insertion of the speculum
The insertion of a speculum, whilst usually not painful, can be uncomfortable, particularly if there is a vaginal infection or lacerations, and using a cold speculum can make this discomfort worse. It can also be an embarrassing procedure for some women, which can be a source of anxiety. In their study with non-pregnant women, Wright et al (2005) found both discomfort and anxiety were reduced when women were offered the opportunity for self-insertion of the speculum. There do not appear to have been any studies looking at the effects of self-insertion of speculums during pregnancy.
When inserting the speculum, it is advisable to apply a thin coating of lubricating gel over the outer aspects of the blades to reduce friction between the blades and the vaginal wall. Hill and Lamvu (2012) found the use of 0.3 mL lubricating gel, compared with water for lubrication, reduced the degree of pain experienced during insertion. Use of aqueous gel for lubrication does not appear to affect the detection of infection from any swabs taken (Harmanli & Jones 2010). The blades should be inserted either obliquely or in the anteroposterior diameter while gently applying a 45° downward pressure. The speculum is rotated during insertion so that the handles are facing the clitoris or anus.
The speculum should be inserted far enough to facilitate visualization of the cervix and, if required, swab taking (Hardy 2007). If the cervix is not visualized, it is possible the speculum is not inserted far enough, in which case the blades should be closed slightly and the speculum inserted deeper or a larger speculum with longer blades be used. The tip of the speculum may have slipped into the anterior fornix which is more likely to occur if a downward pressure is not used during insertion. If this has occurred, the speculum should be withdrawn slightly and the hand holding the end of the speculum raised slightly to depress the speculum tip into the same axis as the cervix.
If the lateral walls of the vagina bulge inwards on opening the blades, visualization of the cervix will also be difficult. This is more likely to occur with obese women or where the woman has a vaginal prolapse. To overcome this, a condom with a small cut at the tip can be placed over the speculum prior to insertion or a larger speculum can be used (although the latter may increase the discomfort for the woman).
Once in position the blades are opened and the cervix and upper part of the vagina can be visualized. This is facilitated by using a good light source and many speculums use a light source that is clipped to the speculum. The light should be positioned so that the midwife is looking just over the top of it. When undertaking the procedure to assess for ruptured membranes, it is important that the woman has been lying down for at least 30 minutes to allow the amniotic fluid to pool in the vagina.
When removing the speculum, care should be taken to ensure the blades are not shut quickly while still in the vagina as they can pinch the walls of the vagina. It is better to close the blades completely once the speculum has been removed. The speculum can be rotated so that it is removed using the same position as it was inserted in.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree