F
Fibrocystic breast changes
Description
Fibrocystic breast changes include the development of excess fibrous tissue, hyperplasia of the epithelial lining of the mammary ducts, proliferation of mammary ducts, and cyst formation. These benign changes are the most frequently occurring breast disorder. Fibrocystic changes occur most frequently in women between 35 and 50 years old, but often begin as early as 20 years old. They are not associated alone with increased breast cancer risk.
Fibrocystic changes most commonly occur in women with premenstrual abnormalities, nulliparous women, women with a history of spontaneous abortion, nonusers of oral contraceptives, and women with early menarche and late menopause.
Pathophysiology
Fibrocystic changes are thought to be heightened responsiveness of breast tissue to circulating estrogen and progesterone. These changes produce pain by nerve irritation from connective tissue edema and fibrosis from nerve pinching.
Clinical manifestations
Manifestations of fibrocystic breast changes include one or more palpable lumps that are usually round, well delineated, and freely movable within the breast. Discomfort ranging from tenderness to pain may also occur.
■ Nipple discharge associated with fibrocystic breasts is often milky, watery-milky, yellow, or green.
Mammography may be helpful in distinguishing fibrocystic changes from breast cancer. However, in some women the breast tissue is so dense that it is difficult to obtain a mammogram. In these situations, ultrasound may be more useful in differentiating a cystic mass from a solid mass.
Nursing and collaborative management
With the initial discovery of a discrete breast mass, aspiration or surgical biopsy may be indicated. If the nodularity is recurrent, a wait of 7 to 10 days may be planned to note any changes related to the menstrual cycle.
Many types of treatment have been suggested for a fibrocystic condition. Some relief may occur if the changes are cyclic with caffeine and coffee and dietary fat reduction; taking vitamins E, A, and B complex and gamma-linolenic acid (evening primrose oil); and the continual wearing of a support bra. Drugs might be recommended, including oral contraceptives and danazol (Danocrine).
Patient and caregiver teaching
Your role in the care of the patient with fibrocystic breast changes is primarily one of teaching.
Fibromyalgia
Description
Fibromyalgia is a chronic disorder characterized by widespread, nonarticular musculoskeletal pain and fatigue with multiple tender points. People with fibromyalgia may also experience nonrestorative sleep, morning stiffness, irritable bowel syndrome, and anxiety. Fibromyalgia is a commonly diagnosed musculoskeletal disorder and a major cause of disability. It affects an estimated 5 million Americans, 75% to 90% of them women.
Fibromyalgia and chronic fatigue syndrome (CFS) share many commonalities (see Table 25, p. 131).
Pathophysiology
There is general agreement that fibromyalgia is a disorder involving neuroendocrine/neurotransmitter dysregulation. The pain amplification experienced by the affected patient is caused by abnormal sensory processing in the central nervous system.
Multiple physiologic abnormalities have been found, including increased levels of substance P in the spinal fluid, low levels of blood flow to the thalamus, dysfunction of the hypothalamic-pituitary-adrenal (HPA) axis, low levels of serotonin and tryptophan, and abnormalities in cytokine function.
Clinical manifestations
The patient complains of a widespread burning pain that worsens and improves through the course of a day. It is often difficult for the patient to discriminate whether pain occurs in the muscles, joints, or soft tissues.
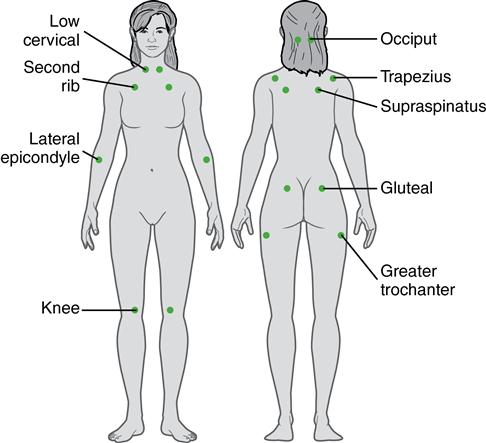
■ Head or facial pain often results from stiff or painful neck and shoulder muscles. This pain can accompany temporomandibular joint dysfunction. Physical examination characteristically reveals point tenderness at 11 or more of 18 identified sites (Fig. 5).
Diagnostic studies
A definitive diagnosis is often difficult to establish. Laboratory results may serve to rule out other suspected disorders.
■ Occasionally a low antinuclear antibody (ANA) titer is found, but it is not considered diagnostic.
■ Muscle biopsy may reveal a nonspecific moth-eaten appearance or fiber atrophy.
The American College of Rheumatology classifies an individual as having fibromyalgia if two criteria are met: (1) pain experienced in 11 of the 18 tender points on palpation and (2) a history of widespread pain for at least 3 months.
Collaborative care
Treatment is symptomatic and requires a high level of patient motivation. You have a key role in teaching the patient to be an active participant in the therapeutic regimen. Rest can help pain, aching, and tenderness.
Drug therapy for the chronic widespread pain associated with fibromyalgia includes pregabalin (Lyrica), duloxetine (Cymbalta), and milnacipran (Savella). Low-dose tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs), or benzodiazepines (e.g., diazepam ([Valium]) may also be prescribed. If the tricyclic antidepressant amitriptyline (Elavil) is not well tolerated, other similar drugs can be substituted, such as doxepin (Sinequan), imipramine (Tofranil), or trazodone (Desyrel).
Nursing and collaborative management
Because of the chronic nature of fibromyalgia and the need to maintain an ongoing rehabilitation program, the patient needs consistent support from you and the other health care team members. Massage is often combined with ultrasound or the application of alternating heat and cold packs to soothe tense, sore muscles and increase blood circulation.
Flail chest
Description
Flail chest results from the fracture of several consecutive ribs in two or more separate locations that cause an unstable segment.
Pathophysiology
The affected (flail) area moves in the opposite direction with respect to the intact portion of the chest. During inspiration, the affected portion is sucked in, and during expiration it bulges out. This paradoxic chest movement prevents adequate ventilation of the lung in the injured area and increases the work of breathing.
Clinical manifestations and diagnostic studies
A flail chest is usually apparent on visual examination of the unconscious patient.
Collaborative care
Initial therapy consists of airway management, adequate ventilation, supplemental oxygen therapy, careful administration of IV solutions, and pain control. Definitive therapy is to reexpand the lung and ensure adequate oxygenation. Although many patients can be managed without mechanical ventilation, intubation and ventilation may be necessary. Surgical fixation of the flail segment may be done. Lung parenchyma and fractured ribs will heal with time.
Fracture
Description
A fracture is a disruption or break in the continuity of the structure of bone. Traumatic injuries account for the majority of fractures, although some fractures are secondary to a disease process (pathologic fractures from cancer or osteoporosis).
Fractures can be classified as open (formerly called compound) or closed (formerly called simple) depending on communication or noncommunication with the external environment. In an open fracture, the skin is broken, exposing the bone and causing soft tissue injury. In a closed fracture, the skin has not been ruptured and remains intact.



