Accommodation: Focusing apparatus of the eye that adjusts to objects at different distances by means of increasing the convexity of the lens (brought about by contraction of the ciliary muscles).
Ametropia: Abnormal vision.
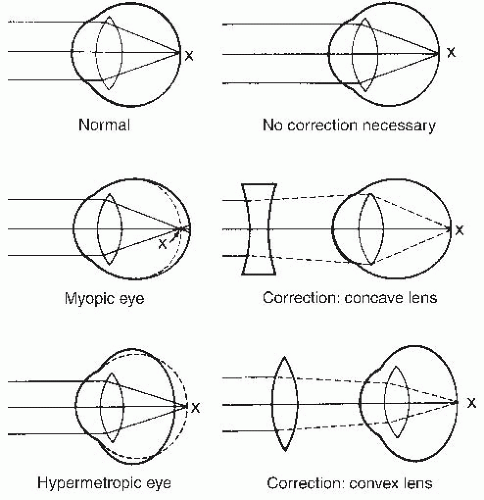
Myopia: Nearsightedness: rays of light coming from an object at a distance of 20 feet or more are brought to a focus in front of the retina.
Hyperopia: Farsightedness: rays of light coming from an object at a distance of 20 feet or more are brought to a focus in back of the retina.
Astigmatism: Uneven curvature of the cornea causing the patient to be unable to focus horizontal and vertical rays of light on the retina at the same time.
Emmetropia: Normal vision: rays of light coming from an object at a distance of 20 feet (6 m) or more are brought to focus on the retina by the lens (see Figure 16-1).
Presbyopia: The elasticity of the lens decreases with increasing age; an emmetropic person with presbyopia will read the paper at arm’s length and will require prescription lenses to correct the problem.
Strabismus: Deviation of the eye so that the visual axes are not physiologically coordinated.
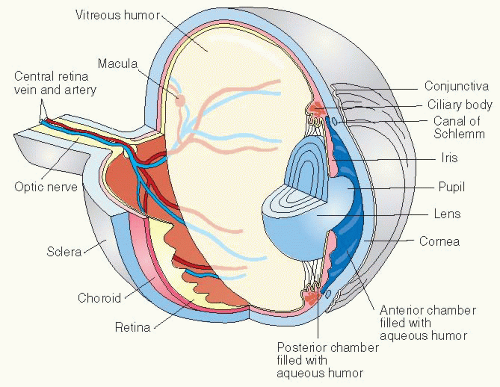
Vision: Passage of rays of light from an object through the cornea, aqueous humor, lens, and vitreous humor to the retina and its appreciation in the cerebral cortex.
Visual acuity: Measurement of a person’s ability to see at a distance or near (reading distance) and is measured against a standard of a normal person’s visual ability.
Ophthalmologist: Physician specializing in diagnosis, surgery, and treatment of the eye; may specialize in a specific part of the eye or disorder, such as a cornea specialist or glaucoma specialist.
Optometrist: Doctor of optometry who can examine, diagnose, and manage visual problems and diseases of the eye, but does not perform surgery.
Optician: Technician who fits, adjusts, and gives eyeglasses or other devices on the written prescription of an ophthalmologist or optometrist.
Ocularist: Technician who makes ophthalmic prostheses.
 Evidence Base
Evidence Base
Explore the chief complaint from patient by asking the following questions:
Is there pain, foreign body sensation (scratchy, something in the eye), photophobia, dryness, redness, itchiness, lacrimation, or drainage?
Is there blurred vision, double vision, loss of vision, or change in vision in a portion of the visual field?
Are there other visual symptoms such as glare, halos, floaters?
Is there difficulty in functioning, such as driving or reading, due to visual problem?
Review related systems.
Neurologic: Are there scintillations, scotomas, transient ischemic attacks, headache, sensory or motor dysfunction?
Ear, nose, and throat: Any nasal congestion, rhinitis, sinus pain, dry mouth?
Integumentary: Are there changes in skin and mucus membranes?
Endocrine: Any complaints of polyuria, polydipsia; signs of hyperthyroidism (see page 922)?
Musculoskeletal: Is there joint pain or swelling?
Review ocular history.
Have there been previous eye injuries, surgeries, and ocular procedures?
Is patient using glasses or contact lenses?
Was there childhood poor vision or patching of the eye?
Are there current visual problems such as glaucoma, cataracts, macular degeneration, or diabetic retinopathy?
Obtain medication history, including nonprescription, herbal, topical, and inhalant products.
Determine allergies to medications; note type of reaction.
Determine history of systemic conditions such as diabetes, cardiovascular disease, arthritis, Marfan’s syndrome, albinism, sickle cell anemia.
Obtain family history of ocular condtions such as glaucoma, cataracts, macular degeneration, color blindness, retinitis pigmentosa, retinoblastoma, nystagmus, keratocunus, choroideremia, corneal dystrophies, and other chronic diseases.
Perform functional assessment.
Depending on the patient’s circumstance, administer the National Eye Institute Visual Function Questionnaire (VFQ-25) available at www.rand.org/health/surveys_tools/vfq.html, or other valid visual functioning questionnaires such as the VF-14.
This helps determine the need for surgery based on the extent to which the eye disorder interferes with the patient’s ability to carry out a visually dependent activity of daily living such as driving and reading.
 GERONTOLOGIC ALERT
GERONTOLOGIC ALERT NURSING ALERT
NURSING ALERT
Letters and objects are of different sizes that can be seen by the normal eye at a distance of 20 feet (6 m) from the chart.
Letters appear in rows and are arranged so the normal eye can see them at distances of 30, 40, and 50 feet (9, 12, and 15 m), and so forth.
Each eye is tested separately, with and without correction (glasses or contact lenses) while the nontesting eye is completely occluded.
Test the right eye (OD) first and then the left eye (OS)
A person who can identify letters of the size 20 at 20 feet (6 at 6 m) is said to have 20/20 (6/6) vision.
If vision is less than 20/200 (6/60), additional tests may be recorded as:
Counting fingers (CF)—at feet (meters).
Hand motion (HM)—ability to detect hand movement at a certain distance.
Light perception and projection (LP).
Light perception only.
No light perception.
Letters and objects are of different sizes that can be seen by the normal eye at a reading distance of 14 inches from the chart.
Letters appear in rows and are arranged so the normal eye can read them at different levels on the Jaeger chart.
Each eye is tested separately, with and without correction (glasses or contact lenses) while the nontesting eye is completely occluded.
Test the right eye (OD) first and then the left eye (OS).
The vision is documented in Jaeger or Snellen notation where J1+ is equivalent to 20/20, J2 equivalent to 20/30 and so forth.
Equipment—light source and test objects. May be performed manually or as automated visual fields.
Peripheral field—useful in detecting decreased peripheral vision in one or both eyes.
Patient is seated 18 to 24 inches (45.5 to 61 cm) in front of the examiner.
The left eye is covered while the patient focuses with the right eye on a spot about 12 inches (30.5 cm) from the eye.
A test object is brought in from the side at 15-degree intervals, through a complete 360 degrees.
The patient signals when he or she sees the test object and again when the object disappears through the 360 degrees.
Equipment.
Polychromatic plates—dots of primary colors printed on a background of similar dots in a confusion of colors.
Individual colored disks—each disk is matched to its next closest color.
Procedure.
Various polychromatic plates are presented to the patient under specified illumination.
The patterns may be letters or numbers that the normal eye can perceive instantly, but that are confusing to the person with a perception defect.
Outcome.
Color blindness—person can’t perceive the figures.
Red-green blindness—8% of males, 0.4% of females.
Blue-yellow blindness—rare.
Refraction and internal examination may be accomplished by instilling a medication with cycloplegic and mydriatic properties into the conjunctiva of the eye. Tropicamide or cyclopentolate are two such medicines that cause ciliary muscle relaxation, pupil dilation (mydriasis), and lowered accommodative power (cycloplegia).
In older children and adults, refraction without the use of drugs is preferred.
Visual screening through a multiple pinhole card can help refractive causes of decreased vision versus decreased vision secondary to organic disease.
The refractive state of the eye can be determined in two ways:
Objectively—through retinoscopy or by automatic refraction (special instrument that measures, computes, and prints out refraction errors of each eye).
Subjectively—trial of lenses to arrive at the best visual image.
Direct ophthalmoscopy—uses a strong light reflected into the interior of the eye through an instrument called an ophthalmoscope.
Indirect ophthalmoscopy—allows the examiner to obtain a stereoscopic view of the retina. Light source is from a headmounted light. The examiner views the retina through a convex lens held in front of the eye and a viewing device on the head mount. The image appears inverted. This method of examination allows the examiner to use binocular vision with depth perception and a wider viewing field.
Clinical significance:
Detection of cataracts, vitreous opacities, corneal scars.
Close examination for the pathologic changes in retinal blood vessels that may occur with diabetes or hypertension.
Examination of the choroid for tumors or inflammation.
Examination of the retina for retinal detachment, scars, or exudates and hemorrhages.
Special equipment that magnifies the cornea, sclera, and anterior chamber and provides oblique views into the trabeculum for examination by the ophthalmologist.
Helps detect disorders of the anterior portion of the eye.
The room is generally darkened and the pupils are dilated.
The patient sits with chin and forehead resting against equipment supports.
Measures intraocular pressure, which depends on the amount of aqueous humor secreted into the eye and ease by which it leaves.
Tonometry is indicated as one of the measurements to screen for glaucoma, assess the development of glaucoma if suspected, evaluate glaucoma therapy, and diagnose phthisis and drug-induced intraocular pressure increase.
Normal tension is considered less than or equal to 20 mm Hg.
Tonometry techniques.
Goldmann applanation tonometry (see Figure 16-3).
This is the most effective measuring method for determining IOP; however, it requires a biomicroscope and a trained interpreter. May be part of the slit-lamp examination or done by handheld device.
After instillation of topical anesthesia, the cornea is flattened by a known amount (3.14 mm).
The pressure necessary to produce this flattening is equal to the IOP, counterbalancing the tonometer.
Schiotz tonometry (rarely used in ophthalmology).
Electronic tonometer that provides a digital reading of intraocular pressure, such as the Tono-Pen.
Pneumotonometer or air applanation tonometry— requires no topical anesthesia and measures tension by sensing deformation of the cornea in reaction to a puff of pressurized air.
Perkins hand-held tonometer.
Finger tension—pressure determined by use of digital pressure.
Provides information concerning vascular obstructions, microaneurysms, abnormal capillary permeability, and defects in retinal pigment permeability.
Introduction of sodium fluorescein IV administration over several minutes, usually through a brachial vein.
Indirect ophthalmoscopy using a blue filter may be done and photographs of the ocular fundus are obtained.
Advise the patient that a series of eye drops will be given to dilate the pupil for better visualization of the retina. The patient will be positioned in a special chair with head immobilized.
Dye will be injected into the arm over several minutes. Photographs will be taken during injection and up to 1 hour after injection.
Adverse effects include nausea due to dye injection, burning in eye from eye drop instillation, blurred vision and photophobia for 4 to 8 hours due to pupil dilation, and possible yellow skin and urine discoloration for up to 48 hours after dye injection.
 DRUG ALERT
DRUG ALERT
A-scan—uses stationary transducers to measure the distance between changes in acoustic density. This is used to differentiate between benign and malignant tumors and to measure the length of the eye to determine the power of an IOL.
B-scan—moves linearly across the eye; increases in acoustic density are shown as an intensification on the line of the scan that presents a picture of the eye and the orbit.
IOL Master technology—evaluates the length of the eye, surface curvature, and IOL power; has increased the accuracy of biometry by five-fold. It is also less technician-dependent for accuracy.
Advise the patient that topical anesthetic drops are applied to the eye before the procedure so the patient will not feel the transducer contacting the eye.
The procedure may take as little as 8 to 10 minutes or 30 minutes or longer, if a lesion is detected, to locate the lesion.
Warn patient not to rub eyes until the anesthetic has worn off to avoid trauma to the eye.
Advise the patient that the eyes are propped open and patient will be positioned lying or sitting down.
Topical anesthetic drops are instilled.
A cotton wick electrode saturated in saline is applied to the cornea.
Various intensities of light are produced and the electrical potential is measured.
Caution the patient not to rub eyes for up to 1 hour after procedure to avoid trauma while eyes are anesthetized.
To dilate or contract the pupil.
To relieve pain, discomfort, itching, and inflammation.
To act as an antiseptic in cleansing the eye.
To combat infection.
To irrigate chemicals or foreign bodies from the eyes.
To remove secretions from the conjunctival sac.
To treat infections.
To relieve itching.
To provide moisture on the surface of the eyes of an unconscious patient.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||
To keep an eye at rest, thereby promoting healing.
To prevent the patient from touching eye.
To absorb secretions.
To protect the eye.
To control or lessen edema.
Typically, removing a foreign body from the eye is an uncomplicated first-aid measure.
However, if the object appears to be embedded, medical intervention is required, that is, local anesthetic, antibiotic therapy, and clinical expertise in using other instruments.
The cornea should be evaluated for abrasion from the foreign body by use of fluorescein staining, even if a foreign body cannot be found.
Contact lenses should be removed in conjunction with a thorough eye exam. An optometrist or ophthalmologist may have to be notified.
Determine the type of lens from the patient or family.
Soft corneal lenses are widely used. The diameter covers the cornea plus a portion of the sclera of the eye. Extended- and daily-wear soft lenses are available.
Rigid or gas-permeable lenses are usually smaller than the cornea of the eye, although some are made to extend beyond the cornea onto the sclera of the eye. These lenses need to be removed promptly.
Do not remove lenses if the iris is not visible on opening the eyelids; await the arrival of an ophthalmologist. If patient is to be transported, note that contacts are in the eyes. (Write out the message and tape it to the patient or send with transporter.)
Collect subjective and objective data about patient’s general state of health.
Ascertain what symptoms the patient has been having (eye pain, visual loss, drainage, history of trauma) and how that has impacted usual activity.
Assess the patient’s mobility and self-care ability.
Assess visual and other sensory impairments.
Gather data regarding usual support systems used by patient. Is family near? Do friends visit regularly?
Review the patient’s daily schedule.
Record pertinent data in patient’s record.
Deficient Knowledge of postoperative expectations and continuing care.
Risk for Injury related to altered vision.
Impaired Environmental Interpretation Syndrome related to visual disturbance.
Fear of blindness related to invasive procedure to eye.
Bathing, Dressing, Feeding Self Care Deficit related to reduced or altered vision.
Table 16-1 Ophthalmic Pharmacologic Agents* | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||
| ||||||||||||||||||||||||||||||||||||||||
| |||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




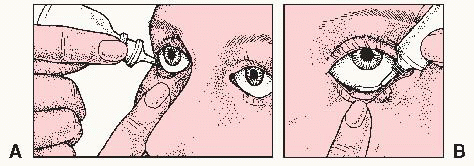
 NURSING ALERT Parietal occlusion (place finger over lacrimal duct for 1 minute) may be necessary after instilling drops if systemic absorption is to be avoided, prolonged corneal contact is desired, or taste or smell of medication is distressing.
NURSING ALERT Parietal occlusion (place finger over lacrimal duct for 1 minute) may be necessary after instilling drops if systemic absorption is to be avoided, prolonged corneal contact is desired, or taste or smell of medication is distressing. Evidence Base American Society of Ophthalmologic Registered Nurses. (2011). Ophthalmic procedures in the office and clinic (3rd ed.). Dubuque, IA: Kendall/Hunt.
Evidence Base American Society of Ophthalmologic Registered Nurses. (2011). Ophthalmic procedures in the office and clinic (3rd ed.). Dubuque, IA: Kendall/Hunt. DRUG ALERT Topical anesthetic drops may be instilled prior to irrigation according to policy or order. If used, do not allow patient to rub eye for 45 minutes to avoid injury.
DRUG ALERT Topical anesthetic drops may be instilled prior to irrigation according to policy or order. If used, do not allow patient to rub eye for 45 minutes to avoid injury. Evidence Base American Society of Ophthalmic Registered Nurses. (2011). Ophthalmic procedures for the office and clinic (3rd ed.). Dubuque, IA: Kendall/Hunt.
Evidence Base American Society of Ophthalmic Registered Nurses. (2011). Ophthalmic procedures for the office and clinic (3rd ed.). Dubuque, IA: Kendall/Hunt. Evidence Base American Ophthalmic Association of Registered Nurses. (2011). Ophthalmic procedures for the office or clinic (3rd ed.). Dubuque, IA: Kendall/Hunt.
Evidence Base American Ophthalmic Association of Registered Nurses. (2011). Ophthalmic procedures for the office or clinic (3rd ed.). Dubuque, IA: Kendall/Hunt.