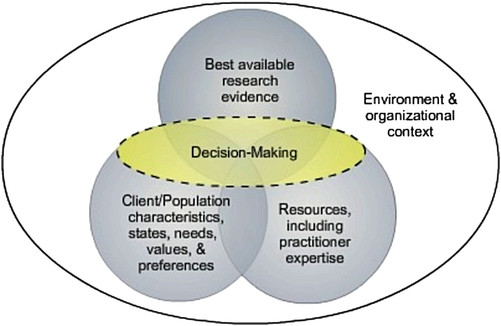
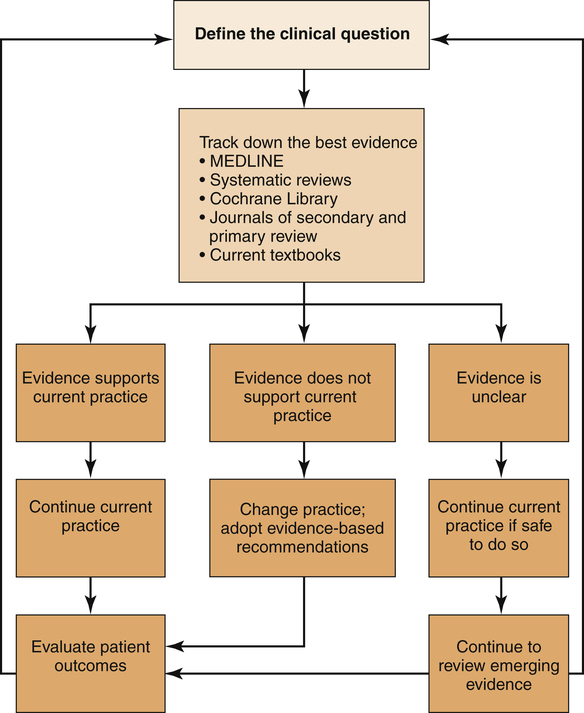
1. Define evidence-based practice. 2. Describe the activities necessary for providing evidence-based psychiatric nursing care. 3. Analyze practice guidelines and their contribution to clinical care. 4. Examine the importance of outcome measurement in psychiatric nursing practice. 5. Evaluate the evidence base for psychiatric nursing practice and an agenda for psychiatric nursing research. Despite existing evidence and agreement on some of the effective treatments for persons with mental illness, research shows that few patients with psychiatric disorders receive evidence-based care (Horvitz-Lennon et al, 2009; Resnick and Rosenheck, 2009). In addition, research is limited on the evidence base of the policies and politics of the mental health delivery system, including agencies, programs, and service effectiveness. • Medication treatment, evaluation and management • Illness management and recovery • Peer/consumer-operated services and support • Permanent supportive housing • Assertive community treatment • Substance abuse treatment integrated with mental health treatment • Crisis/hospital diversion programs • Treatment of depression in older adults • Specific interventions for children and adolescents, including therapeutic foster care, multisystemic therapy, positive behavior supports in schools, and parent-child interaction therapy The National Registry of Evidence-Based Programs and Practices (NREPP), developed by the U.S. Substance Abuse and Mental Health Services Administration (SAMHSA), is a source of information on a wide range of evidence-based interventions to prevent and treat mental and substance use disorders (www.nrepp.samhsa.gov) (Hennessy and Green-Hennessy, 2011). For psychiatric nurses the use of evidence-based practices raises three questions: 1. Do psychiatric nurses know the efficacy of their treatments and interventions? 2. Is the care they provide evidence-based? 3. Are they documenting the nature and outcomes of their nursing care? Accountability for patient care outcomes is a basic responsibility of professional nurses. Central to this accountability is the ability to examine nursing practice patterns, identify the best available research related to them, and demonstrate sound clinical decision making that incorporates environmental and organizational influences (Figure 4-1). It also takes into account the patients’ values, characteristics, preferences, and circumstances, as well as the skill and resources of the nurse (Fisher and Happell, 2009). Evidence-based practice is the conscientious, explicit, and judicious use of the best evidence gained from systematic research for the purpose of making informed decisions about the care of individual patients (Sackett, 2003). It blends a nurse’s clinical expertise with the best available research evidence. It also is a method of self-directed, career-long learning in which the nurse continuously seeks the best possible outcomes for patients and implements effective interventions based on the most current research evidence (Rice, 2008a; Melnyk and Fineout-Overholt, 2010). The evidence-based model is based on the following assumptions: • Information gathered only from one’s own clinical practice often involves unsystematic observations and subjective judgments. • All clinicians have biases that influence their clinical care. • Even theories from respected colleagues must be tested and must provide evidence of efficacy in order to be useful to clinical practice. • Knowing that conclusions were reached through scientific methodology permits a higher level of confidence in one’s nursing actions. • Replication of findings increases confidence in their validity. • Randomized controlled clinical trials are the gold standard of research methodologies. • Nurses who are able to critically review the research literature related to a specific clinical question will be able to provide better nursing care. There are four bases for nursing practice (Stetler et al, 1998): 1. The lowest level is the traditional basis for practice, which includes rituals, unverified rules, anecdotes, customs, opinions, and unit culture. 2. The second level is the regulatory basis for practice, which includes state practice acts and reimbursement and other regulatory requirements. 3. The third level is the philosophical or conceptual basis for practice, which includes the mission, values, and vision of the organization; professional practice models; untested conceptual frameworks; ethical frameworks; and professional codes. 4. The fourth and highest level is evidence-based practice, which includes research findings, performance data, and consensus recommendations of recognized experts. It is important to remember that not all clinical practice is based on quantitative research and randomized clinical trials. Qualitative studies that aim to understand the nature of the human experience are another valid type of evidence (Williamson, 2009). Also, some types of problems cannot be adequately tested empirically. Clinical experience is invaluable in these situations (Nolan, 2008). Evidence-based psychiatric nursing practice involves the following series of activities (Figure 4-2). Defining the clinical question is the first step in the process. Clear answers require clear questions. A good clinical question involves defining the patient’s problems, identifying the existing nursing intervention, and specifying the expected outcome (Rice, 2010). This process should be completed in partnership with the patient and family and in collaboration with other health care providers (Horsfall et al, 2011). Thus finding the evidence can be challenging. However, advances in information technology have made it easier to search the health care literature, and a number of sources can be used to find the evidence (Box 4-1). Access to electronic databases such as Medline is widespread and journals offer access through their websites, displaying tables of contents, abstracts, and full-text articles. Many of these articles are systematic reviews prepared by others. A systematic reviewer uses explicit methods of searching for and critically appraising the primary studies. If these are comparable, the reviewer may then perform a formal quantitative synthesis, called meta-analysis, of the results. A meta-analysis summarizes the findings from a number of studies in order to arrive at an objective and authoritative guide to treatment for a given condition (Mundy and Stein, 2008). In evaluating the evidence the nurse should consider the hierarchy of research evidence (Rice, 2008b). A commonly used hierarchy (with 1 indicating the best) for research designs is presented in Box 4-2. Systematic reviews or meta-analyses of randomized controlled trials (RCTs) are the most reliable study design for the evaluation of treatments. However, for many interventions, RCTs may not exist, and the nurse needs to use evidence from the next level of the hierarchy, with the idea that the nurse selects the intervention that is supported by the best available evidence.
Evidence-Based Psychiatric Nursing Practice
Evidence-Based Practice
Bases for Nursing Practice
Developing Evidence-Based Care
Evidence-Based Psychiatric Nursing Practice
Get Clinical Tree app for offline access