Chapter 9. Emetics and antiemetics, cough remedies, respiratory stimulants
At the end of this chapter, the reader should be able to:
• understand what is meant by the vomiting centre and chemoreceptor trigger zone (CTZ)
• describe how they are stimulated
• give an account of the emetics and the classes of antiemetic drugs
• understand the uses and limitations of cough suppressants
• describe inhalations and mucolytic agents
• explain the term respiratory failure
Emetics
Mechanism of vomiting
Vomiting is a complex series of actions involving the stomach, oesophagus and pharynx with the voluntary muscles of the chest and abdomen, and results in the ejection of the stomach contents. A vomiting centre in the medulla of the brain coordinates these actions. This centre can be stimulated:
• Directly from the labyrinth of the ear in conditions such as seasickness or vertigo.
• By gastric irritation or distension.
• By mental activity (e.g. being sick with fright; imagining something extremely unpleasant).
• By stimulation of the 5-hydroxytryptamine (5-HT; serotonin) receptors of the CTZ. Circulating cytotoxic drugs (particularly cisplatin; see p. 350) release 5-HT from nerve endings, and this activates the CTZ receptors. From the CTZ, impulses travel to the vomiting centre and activate it by acting on muscarinic acetylcholine (ACh) receptors.
The stimulation of vomiting outlined above is summarized in Figure 9.1.
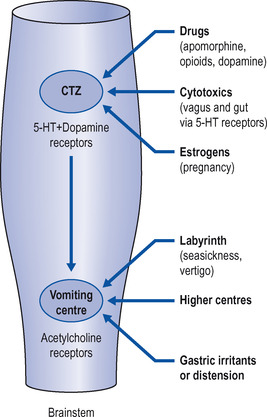 |
| Figure 9.1 Drugs and other factors stimulating the CTZ and vomiting centre. |
Before the act of vomiting occurs, stimulation of the vomiting centre produces a sensation known as nausea, which is often associated with increased secretion by the salivary and bronchial glands. Drugs that provoke vomiting are called emetics.
Emetics are rarely used in medical practice except in cases of poisoning. They may be divided into two types:
• reflex emetics, e.g. ipecacuanha
• central emetics, e.g. apomorphine.
Reflex emetics
This group of drugs produces vomiting by irritating the stomach. The only one in common use is ipecacuanha, a plant extract, which is dispensed as ipecacuanha emetic mixture, and vomiting should occur in 15–30 minutes. It may be used as a first-aid treatment for overdose provided that:
• the patient is fully conscious
• overdose is not of corrosive substances or petroleum products, when inhalation of vomit could be fatal.
Ipecacuanha can be used up to 1 hour after ingestion of poison and longer for some substances, such as tricyclic antidepressants and salicylates, when gastric emptying is delayed. It is not as effective as a stomach washout, but is particularly useful in children, when the upset caused by the process of lavage should be avoided if possible, and in removing such objects as berries, which cannot be washed out of the stomach. In general, the use of emetics in poisoning is decreasing because there is little evidence that, even if used soon after ingestion of poison, they usefully reduce absorption.
Central emetics (Those acting on the brain)
Apomorphine stimulates dopamine receptors in the CTZ. It is closely related to morphine but has none of its analgesic effects. It has, however, a very powerful emetic action and also produces some cerebral depression. It was formerly used as an emetic but because of its depressant action it should not be used in treating patients who have taken an overdose. At present its use is confined to patients with resistant Parkinson’s disease (see p. 260).
Antiemetics
Antiemetics should not be taken if the cause of the vomiting is unknown, as they may hinder diagnosis. Vomiting may be the result of, for example, drug overdose or diabetic ketoacidosis, which should be diagnosed and treated appropriately.
It is believed that acetylcholine, histamine, dopamine and 5-HT act as intermediate transmitters in the CTZ and vomiting centre. By blocking the action of these substances on their receptors, it is possible to prevent or diminish vomiting (Table 9.1).
| Types of vomiting | Effective drug | Comment |
|---|---|---|
| Vomiting of pregnancy | Promethazine, sometimes combined with pyridoxine | Dietary management if possible. Keep drugs to a minimum in early pregnancy, owing to risk of fetal deformity. Promethazine appears to be safe |
| Motion sickness | Hyoscine | Dry mouth. Blurred vision. Some sedation. Short journey |
| Cinnarizine | Preferred for longer journey | |
| Vertigo | Prochlorperazine | |
| Cinnarizine | ||
| Betahistine | ||
| Opioids | Prochlorperazine | |
| Metoclopramide | ||
| Chlorpromazine | ||
| Haloperidol | Less sedating. Long-acting | |
| Cytotoxic drugs | Prochlorperazine | Sedative |
| Domperidone | Not sedative | |
| Metoclopramide | High doses required | |
| Ondansetron | ||
| Cannabinoids | ||
| Benzodiazepines | Particularly if anxiety is a factor | |
| Dexamethasone | ||
| Migraine | Metoclopramide | |
| Post-anaesthetic (often opioid) | Prochlorperazine | |
| Haloperidol |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


