life-threatening problems. If conditions are identified that present an immediate threat to life, you are required to stop and take corrective action prior to moving on to the next steps.
Call for help.
Ensure the area is safe for you to enter, with no live electric current, hazardous materials, dangerous persons or other threats.
Remove the patient from potential source of danger, such as live electric current, water, or fire. If hazardous materials are present, consult a MSDS book for decontamination procedures.
Determine whether patient is conscious.
Assess for adequate airway, breathing, and circulation in systematic manner. If any of these are absent, or inadequate, begin basic life support.
Assess pupillary reaction and level of responsiveness to voice or touch, as indicated.
If the patient is unconscious or has sustained a significant head injury, assume there is a spinal cord injury and maintain C-spine stabilization.
Undress the patient to assess for wounds and skin lesions as indicated. Control any hemorrhage, as needed.
When help arrives, assist with further assessment and transport, as needed.
A—Airway: Does the patient have an open airway? Is the patient able to speak, swallow, or cry? Check for airway obstructions such as loose teeth, foreign objects, bleeding, vomitus, or other secretions. Immediately treat anything that compromises the airway. Never do a blind finger sweep of an airway.
B—Breathing: Is the patient breathing adequately? Assess for equal rise and fall of the chest (check for bilateral breath sounds), respiratory rate and pattern, skin color, use of accessory muscles, adventitious breath sounds, integrity of the chest wall, and position of the trachea. All major trauma patients require supplemental oxygen via a nonrebreather mask at 12 to 15L/min. Dress any penetrating chest injuries with occlusive dressings.
C—Circulation: Is circulation in immediate jeopardy? Can you palpate a central pulse? What is the quality (strong, weak, slow, rapid)? Is the skin warm and dry? Is the skin color normal? Obtain a blood pressure (BP; in both arms if chest trauma or dissecting aortic aneurysm is suspected). Is there any major bleeding?
D—Disability: Assess level of consciousness and pupils (a more thorough neurologic survey will be completed in the secondary survey). Assess level of consciousness using the AVPU scale:
A—Is the patient alert? Are they looking at you and responding?
V—Does the patient respond to voice? Do they open their eyes or respond when you call them?
P—Does the patient respond to painful stimulus? Do they respond to sternal rub or nailbed pressure?
U—The patient is unresponsive even to painful stimulus.
Expose/environmental control: It is necessary to remove all of the patient’s clothing in order to identify all injuries. You must then prevent heat loss by using warm blankets, overhead warmers, and warmed intravenous (IV) fluids unless induced hypothermia is indicated. If your facility has a dedicated Trauma/Resuscitation room, keeping the temperature turned up aids in preventing heat loss.
Full set of vital signs:
Obtain a full set of vital signs including BP, heart rate, respiratory rate, temperature, and oxygen saturation.
As stated previously, obtain BP in both arms if chest trauma or dissecting aortic aneurysm is suspected.
Institute continuous cardiac monitoring.
Assess Glasgow Coma Scale (GCS) (see page 483) and pain scores.
Five interventions:
Vascular access with two large-bore IV catheters, if possible.
Pulse oximetry to measure the oxygen saturation; consider capnography to measure end-tidal carbon dioxide (EtCO2); noninvasive ultrasonic cardiac output monitor; and 12-lead electrocardiogram (ECG).
Indwelling urinary catheter (do not insert if you note blood at the meatus, blood in the scrotum, or if you suspect a pelvic fracture).
Gastric tube (if there is evidence of facial fractures, insert the tube orally rather than nasally).
Laboratory studies frequently include type and cross matching, complete blood count (CBC), urine drug screen, blood alcohol, electrolytes, prothrombin time and partial thromboplastin time, arterial blood gas (ABG), and pregnancy test, if applicable.
Facilitate family presence: Family presence is important during unexpected, potentially life-threatening events. They often have information that is critical in formulating the correct treatment plan. It is important to assess and respect the family’s needs and wishes. If any member of the family wishes to be present during the resuscitation, it is imperative to assign a staff member to that person to explain what is being
done and offer support. Resuscitation rooms are often loud and appear chaotic. Assigning a staff member to any family wishing to be present can do much to alleviate their anxiety and assure them that everything is being done to help their loved one. If a family member does not wish to be present, providing them with a quiet area to wait and assigning a staff member as a contact person or liaison can be helpful.
Give comfort measures: These include verbal reassurances as well as pain management as appropriate. Do not forget to give comfort measures to the family as well as the patient during the resuscitation process.
Obtain prehospital information from emergency personnel, patient, family, or bystanders using the mnemonic MIVT.
M—Mechanism of injury: It is helpful to understand the mechanism of injury to anticipate probable injuries. It is particularly helpful in motor vehicle accidents to know such information as external and internal damage to the car (or at least if the car was drivable after the accident), if the patient was ejected, if they were wearing a seat belt, if airbags were deployed, and the period of time elapsed before the patient received medical attention.
I—Injuries sustained or suspected: Ask prehospital personnel to list any injuries that they have identified. Most prehospital providers will have completed a rapid trauma survey, including looking for DCAP/BTLS (deformities, contusions, abrasions, punctures/burns, tenderness, lacerations, and swelling)
V—Vital signs: What were the prehospital vital signs?
T—Treatment: What treatment did the patient receive before arriving at the hospital and what was the patient’s response to those interventions?
If the patient is conscious, it is essential to ask him what happened. How did the accident occur? Why did it happen? A fall, for example, may not be a simple fall—perhaps the patient blacked out and then fell. If the patient is conscious and time permits, explore the chief complaint through the OPQRST mnemonic.
O—Onset: When did they first notice symptoms? Was today the first time? Has it been ongoing? Is it getting progressively worse?
P—Provokes, Palliates, Precipitates: What makes the symptoms better or worse?
Q—Quality: How would they describe the discomfort? Burning, throbbing, aching, and like an electric shock are all commonly used to describe the quality of pain.
R—Region, Radiates: Can the patient point to the pain with one finger? Does it move or shoot anywhere?
S—Severity, associated Symptoms: How do they rate their symptom? Is it accompanied by anything else such as numbness, tingling, or nausea?
T—Timing: Have the symptoms been constant or do they come and go? How often?
Obtain past medical history from the patient or a family member or friend; it may be helpful to utilize the mnemonic SAMPLE to assist in organizing history information:
S—Signs and symptoms, including chief complaint and OPQRST.
A—Allergies to foods and medications.
M—Medications, including herbal supplements and over-the-counters.
P—Past medical and surgical history.
L—Last oral intake.
E—Events leading up to the incident.
Plus any history of alcohol or illicit drug use.
 NURSING ALERT
NURSING ALERT
Head and face.
Inspect for any lacerations, abrasions, contusions, avulsions, puncture wounds, impaled objects, ecchymosis, or edema. Hair can hide injuries, so take time to do a complete inspection. Scalp lacerations also tend to bleed profusely, further obscuring the area from quick inspections.
Gently palpate for crepitus, crackling, or bony deformities.
Inspect ears and nares for any bleeding or drainage, if present, check for Halo sign.
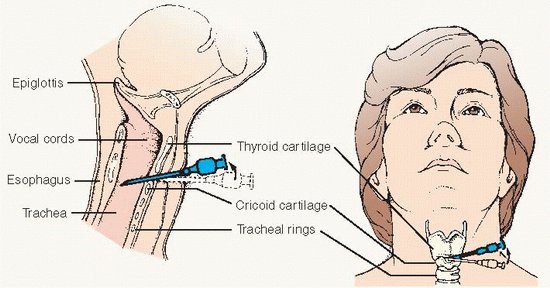
Neck (ensure proper C-spine stabilization is maintained).
Inspect for any punctures, lacerations, contusions, swelling, tracheal deviation, JVD, or subcutaneous emphysema.
Check for stomas or Medic Alert tags.
Gently palpate for midline cervical tenderness.
Chest.
Inspect for breathing effectiveness, paradoxical (uneven) chest wall movement, disruptions in chest wall integrity (lacerations, punctures, subcutaneous emphysema).
Auscultate for bilateral breath sounds and adventitious breath sounds.
Auscultate heart tones (muffled).
Gently palpate for bony crepitus or deformities.
Abdomen/flanks.
Inspect for lacerations, abrasions, contusions, avulsions, puncture wounds, impaled objects, ecchymosis, edema, scars, eviscerations, or distention.
Auscultate for the presence of bowel sounds.
Gently palpate for rigidity, guarding, masses, or areas of tenderness.
Pelvis/perineum.
Inspect for lacerations, abrasions, contusions, avulsions, puncture wounds, impaled objects, ecchymosis, edema, or scars. Look for blood at the urinary meatus and vagina in
females. Look for priapism in males (which could indicate spinal cord injury).
Gently palpate for pelvic instability or tenderness (do not rock the pelvis).
Neurologic/spinal (maintaining proper stabilization).
Reassess mental status.
Gently palpate for midline bony spinal tenderness.
Check for paresthesias and determine sensory level.
Check motor function and sphincter tone.
Extremities.
Inspect skin color and temperature. Look for signs of injury and bleeding. Does the patient have movement in all four extremities? Touch the patient on a distal extremity and ask them to identify the part you are touching.
Gently palpate peripheral pulses, any bony crepitus, or areas of tenderness.
Check capillary refill.
Gently palpate extremities for compartment firmness or signs of compartment syndrome.
 NURSING ALERT
NURSING ALERT NURSING ALERT
NURSING ALERT
Conditions requiring immediate clinician assessment. Any delay in treatment is potentially life- or limb-threatening. These are the patients that are in active danger of dying if there is no immediate intervention and will require admission.
Includes conditions such as:
Airway or severe respiratory compromise.
Cardiac arrest.
Severe shock.
Symptomatic cervical spine injury.
Multisystem trauma.
Altered level of consciousness (LOC) (GCS < 10).
Eclampsia.
Acute mental status changes or unresponsiveness.
These are conditions that are not in immediate danger, but have the potential to deteriorate rapidly if not treated.
Conditions include:
Head injuries.
Trauma.
Conscious overdose.
Severe allergic reaction without airway compromise.
Chemical exposure to the eyes.
Chest pain without hemodynamic instability.
Back pain.
GI bleed with unstable vital signs.
Stroke with deficit.
Severe asthma without airway compromise.
Abdominal pain in patients older than age 50.
Vomiting and diarrhea with dehydration.
Fever in infants younger than age 3 months.
Acute psychotic episode.
Severe headache.
Any pain greater than 7 on a scale of 1 to 10.
Any sexual assault.
Any neonate age 7 days or younger.
Conditions requiring urgent care-level activities with stable vital signs, but have the potential to deteriorate and utilize multiple resources.
Conditions include:
Stable conditions that use few resources.
Conditions include:
Alert head injury without vomiting.
Minor trauma.
Vomiting and diarrhea in patient older than age 2 without evidence of dehydration.
Earache.
Minor allergic reaction.
Corneal foreign body.
Chronic back pain.
Stable conditions that utilize little to no resources.
Conditions include:
Minor trauma, not acute.
Sore throat.
Minor symptoms.
Chronic abdominal pain.
 NURSING ALERT
NURSING ALERT
Understand and accept the basic anxieties of the acutely ill or traumatized patient. Be aware of the patient’s fear of death, disablement, and isolation.
Personalize the situation as much as possible. Speak, react, and respond in a warm manner, reassure, but remain realistic and do not patronize the patient.
Give explanations on a level that the patient can grasp. An informed patient can cope with psychological/physiologic stress in a more positive manner.
Accept the rights of the patient and family to have and display their own feelings.
Maintain a calm and reassuring manner—helps the emotionally distressed patient or family to mobilize their psychological resources.
Include the patient’s family or significant others if the patient wishes.
Encourage the patient or family to reach out to their support system. Often friends, other family members, or clergy can be of great comfort.
Understand and support the patient’s feelings concerning loss of control (emotional, physical, and intellectual). If possible, giving the patient options and choices can help alleviate some of their feelings of helplessness.
Treat the unconscious patient as if conscious. Touch, call by name, and explain every procedure that is done. Avoid making negative comments about the patient’s condition.
Orient the patient to person, time, and place as soon as he or she is conscious; reinforce by repeating this information.
Bring the patient back to reality in a calm and reassuring way.
Encourage the family, when possible, to touch the patient and aid in orienting the patient to reality.
Be prepared to handle all aspects of acute illness and trauma; know what to expect and what to do. When in doubt, stop, take a deep breath, and refocus. This alleviates the nurse’s anxieties and increases the patient’s confidence.
Inform the family where the patient is and give as much information as possible about the treatment he or she is receiving.
Consider allowing a family member to be present during the resuscitation. Assign a staff person to the family member to explain procedures and offer comfort.
Recognize the anxiety of the family and allow them to talk about their feelings. Acknowledge expressions of remorse, anger, guilt, and criticism.
Allow the family to relive the events, actions, and feelings preceding admission to the ED.
Deal with reality as gently and quickly as possible; avoid encouraging and supporting denial.
Assist the family to cope with sudden and unexpected death. Some helpful measures include the following:
Take the family to a private place.
Talk to all of the family together so they can mourn together.
Assure the family that everything possible was done; inform them of the treatment rendered.
Avoid using euphemisms such as “passed on.” Show the family that you care by touching, offering coffee.
Allow family to talk about the deceased—permits ventilation of feelings of loss. Encourage family to talk about events preceding admission to the ED.
Encourage family to support each other and to express emotions freely—grief, loss, anger, helplessness, tears, disbelief.
Avoid volunteering unnecessary information (eg, patient was drinking).
Avoid giving sedation to family members—may mask or delay the grieving process, which is necessary to achieve emotional equilibrium and prevent prolonged depression.
Be cognizant of cultural and religious beliefs and needs.
Encourage family members to view the body if they wish— to do so helps to integrate the loss (cover mutilated areas).
Prepare the family for visual images and explain any legal requirements.
Go with family to see the body.
Show acceptance of the body by touching to give family permission to touch and talk to the body.
Spend a few minutes with the family, listening to them.
Allow the family some private time with the body, if appropriate.
Encourage the ED staff to discuss among themselves their reaction to the event to share intense feelings for review and for group support. Organize a formal debriefing session for staff if warranted by circumstances of the event.
ABCD.
Evaluate pain using the OPQRST mnemonic.
Assess pain score using a pain rating tool, such as the numeric rating scale, visual analogue scale, Wong-Baker FACES pain scale (see page 1447), FLACC (faces, legs, activity, cry, and consolability) behavioral scale, verbal rating scale, or Abbey pain scale.
Pain is always subjective. Never doubt that a patient has pain based on how they look.
Establish a supportive relationship with the patient.
Respect the patient’s response to pain and its management.
Educate the patient regarding methods of pain relief, preventive measures, and expectations.
Establish a baseline pain level, as well as a pain level the patient would consider tolerable.
Administer pharmaceutical and nonpharmaceutical pain control.
Monitor the patient’s response to and effectiveness of treatment.
If initial interventions do not bring pain down to the tolerable level, explore other options.
Always reassure your patient and let them know you take their pain seriously.
 NURSING ALERT
NURSING ALERT Evidence Base
Evidence Base
Cardiac arrest.
Ventricular fibrillation.
Ventricular tachycardia.
Asystole.
Pulseless electrical activity.
Respiratory arrest.
Drowning.
Stroke.
Foreign-body airway obstruction.
Smoke inhalation.
Drug overdose.
Electrocution/injury by lightning.
Suffocation.
Accident/injury.
Coma.
Epiglottitis.
Backboard
Oral airway
Bag-valve-mask (BVM) device
Oxygen
IV setup
Defibrillator
Emergency cardiac drugs Cardiac monitor
Electrocardiograph machine
Intubation equipment
Suction
PROCEDURE | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 NURSING ALERT
NURSING ALERT Evidence Base
Evidence Base
Immediate loss of consciousness.
Absence of palpable carotid or femoral pulse; pulselessness in large arteries.
Absence of breath sounds or air movement through nose or mouth.
Postresuscitation distress syndrome (secondary derangements in multiple organs).
Neurologic impairment, brain damage.
 NURSING ALERT
NURSING ALERT
Persistent coma in the adult patient following cardiac arrest.
Return of spontaneous circulation.
 NURSING ALERT
NURSING ALERT
Institute continuous cardiac monitoring. Monitor for bradycardia caused by cooling or other dysrhythmias.
Institute continuous temperature monitoring, preferably core temperature.
Frequently monitor blood pressure to avoid hypotension, particularly during rewarming.
Monitor CBC for signs of infection, since temperature will not be an accurate sign. Monitor electrolyte panel for hypokalemia caused by hypothermia. ABGs should be analyzed at patient’s actual body temperature.
Assess skin every 2 hours for pressure and cold injury.
Shivering—patient may require sedation and neuromuscular blockade to relieve shivering, which will interfere with hypothermia.
Seizures—continuous neuromuscular blockade may mask post-cardiac arrest seizure activity.
A number of commercially available cooling devices are currently available, including cooling blankets, cooling gel pads applied to the skin, and centrally inserted heat-exchange catheters.
Cooling blankets are placed under and over the patient and cool utilizing circulated chilled water. They are easy to apply; however, they can have poor surface contact, making it difficult to maintain a targeted temperature.
Devices utilizing adhesive gel pads are also easy to apply and provide improved surface contact to facilitate rate and maintenance of cooling. Contoured cooling garments are also available.
With any surface cooling method, ice packs are often used to assist in initial cooling and then removed. Maintenance is controlled by the commercial device.
Centrally inserted heat-exchange catheters use chilled saline passed through a coiled section of catheter.
These coils provide a large surface area for blood to pass over and heat exchange to occur.
Normally placed in the femoral vein, these catheters allow for rapid cooling and extremely tight control without promoting shivering.
3-6 L bag of refrigerated 39° F (4° C) lactated Ringer’s solution
Small plastic bags
Ample supply of ice cubes
PRE PROCEDURE | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 NURSING ALERT
NURSING ALERT Evidence Base
Evidence Base
Weak, ineffective cough.
High-pitched noises on inspiration.
Respiratory distress.
Inability to speak or breathe.
Cyanosis.
Hands at throat.
PROCEDURE GUIDELINES 35-3 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Compromised airway and inability to intubate or perform tracheostomy:
Complete foreign-body airway obstruction.
Trauma to head and neck.
Allergic reaction causing laryngeal edema.
Laryngeal fracture.
Tracheal rupture.
Tracheal transection with distal tracheal retraction into the mediastinum.
Chlorhexidine or povidone iodine for site cleansing
Cricothyrotomy catheter (if available)
IV catheters (if commercial cricothyrotomy catheter is not available): 16G or larger IV catheters (adult) 16G or 18G IV catheters (children)
3.0 endotracheal tube connecter (bag-valve-mask connecter)
10 mL Luer-loc syringe with 5 mL of saline
PROCEDURE | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Evidence Base
Evidence Base NURSING ALERT
NURSING ALERT
Airway: assess for vomitus, bleeding, and foreign objects. Ensure cervical spine immobilization.
Breathing: assess for abnormally slow or shallow respirations. An elevated carbon dioxide partial pressure can worsen cerebral edema.
Circulation: assess pulse and bleeding.
Disability: assess the patient’s neurologic status.
Open the airway using the jaw-thrust technique without head tilt. Oral suction equipment (to handle heavy vomitus) should be at hand. Make sure that you do not stimulate the gag reflex as this can cause increases in ICP.
Administer high-flow oxygen.
Assist inadequate respirations with a bag-valve-mask, as necessary. Prophylactic hyperventilation is not indicated.
Control bleeding—do not apply pressure to the injury site. Apply a bulky, loose dressing. Do not attempt to stop the flow of blood or cerebrospinal fluid (CSF) from the nose or ears; apply a loose dressing, if needed.
Initiate two IV lines. The rate of flow should be determined by the patient’s hemodynamic status.
History.
Mechanism of injury.
Presence and duration of loss of consciousness.
Amnesia of the event.
Position found.
LOC.
Change in mental status is the most sensitive indicator of a change in the patient’s condition.
GCS (see page 483).
Vital signs.
Hypertension and bradycardia are late signs of increasing ICP.
Patients with a head injury may have associated cardiac dysrhythmias, noted by an irregular or rapid pulse.
Changing patterns of respiration or apnea may indicate a head injury.
Elevated temperature—high temperatures may be associated with head injury.
Unequal or unresponsive pupils.
Confusion or personality changes.
Impaired vision.
One or both eyes appear sunken.
Seizure activity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree