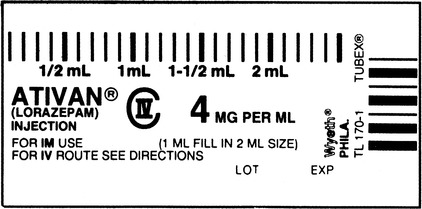
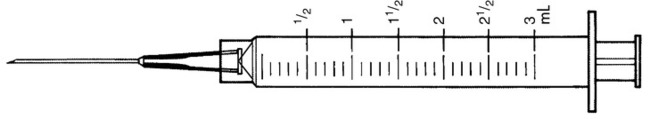
2. Describe the purpose of administering the combination of D50W, atropine, and naloxone (Narcan). 3. What treatment will Z.H. require in the ED? 4. Within 30 minutes of receiving the naloxone (Narcan), Z.H. is starting to respond. You need to continue to observe her closely because: (Select all that apply.) a. multiple doses of naloxone (Narcan) increase Z.H.’s risk of developing pulmonary edema. b. adverse effects of naloxone (Narcan) are atrial fibrillation and ventricular dysrhythmias. c. the opioid effect associated with the drug overdose might return after the naloxone (Narcan) is metabolized. d. reversing the effects of the drug overdose too quickly causes a rebound decline in the level of consciousness. 8. What is a chemically impaired nurse? 9. What is the profile of an impaired nurse? List five characteristics. 10. One of Z.H.’s colleagues calls on the phone to ask how she is. She tells you that she thought something was wrong with Z.H. because her behavior was so erratic, but “I had no idea it was drugs. I didn’t think Z.H. would ever do anything like that!” What are the visible signs of a chemically impaired nurse? 11. State four problems associated with impaired nurses who are practicing. 12. Z.H. asks what is going to happen to her career. What are the regulatory issues related to impaired nurses that will guide your response? 1. List five things you would do in order of priority. 2. Describe status epilepticus. 3. Given A.A.’s history, state at least two possible causes for his tonic-clonic seizure. The rapid response team is called, and the attending physician orders the following: 4. Indicate the expected outcome for A.A. associated with each medication. 5. List one thing you would be particularly alert for when giving lorazepam (Ativan) intravenously. 6. The lorazepam (Ativan) is supplied in a single-use vial. How many milliliters will A.A. receive? Shade in the dose on the syringe. 7. What is the significance of this time lapse? 8. The physician decides to administer propofol (Diprivan) and intubate A.A. to support his airway. What is propofol (Diprivan), and why is it being administered to A.A.? 9. The physician orders phenytoin (Dilantin) 15 mg/kg IV loading dose to be given at a rate of 50 mg/min. What is the rationale behind administering phenytoin (Dilantin)? 10. A.A. weighs 143 pounds. How much phenytoin (Dilantin) will you administer? 11. As you prepare to administer the phenytoin (Dilantin), you see that A.A. has D5W infusing at 75 mL per hour. Why does this concern you and what are your options? 12. A.A. is transported to the ICU, and his seizure activity ceases. What are the main complications of status epilepticus that the nurse will monitor for? 13. Identify nursing interventions that are appropriate for A.A. at this time. 1. What will your first action be? 2. What immediate care will you provide to R.J.? 3. Given R.J.’s admitting diagnosis, what differential diagnoses do you consider? 4. Suddenly, you remember R.J.’s wife, who is anxiously hovering over you in the room. What are you going to do? 5. What is Beck’s triad, and what causes it? 6. Explain the rationale for the surgeon performing a pericardiocentesis. 7. What is the significance of the surgeon aspirating unclotted blood? 8. The physician orders dopamine IV to “begin at 4 mcg/kg/min and titrate to maintain a systolic BP over 100 mm Hg.” What is the rationale for this order? 9. Describe how you will titrate the dopamine infusion. 10. Identify four assessment findings that would indicate that R.J. is responding to your immediate actions. R.J. is transferred to the thoracic intensive care unit (TICU) for observation. 11. As the team prepares R.J.’s transfer, you go to find R.J.’s wife to thank her for alerting you to the emergency so promptly and to tell her what has happened. Briefly, and in lay terms, how would you explain what happened to her husband? 12. As you both get up to leave, Mrs. J. suddenly turns pale and says she feels very dizzy. What are you going to do? K.L. reports that he is getting nauseated but not thirsty. VS are 92/58, 116, 32. 3. What additional interventions do you need to institute? 4. What assessment indicators would you monitor in K.L.? 5. While caring for K.L., which of these care activities can be safely delegated to the nursing assistive personnel (NAP)? (Select all that apply.) a. Initiating a pulse oximetry monitoring b. Measuring K.L.’s vital signs every 15 minutes c. Obtaining consent from K.L. for a possible blood transfusion d. Assessing K.L.’s peripheral circulation e. Emptying each Foley catheter collection bag each hour f. Monitoring K.L.’s hemoglobin and hematocrit levels 6. Interpret the preceding arterial blood gases (ABGs). What do they tell you? 10. Identify five immediate interventions you should initiate. 11. You are preparing to administer the first of 2 units of packed RBCs. Evaluate each of the following statements about the safe administration of blood. Enter “T” for true or “F” for false. Discuss why the false statements are incorrect. ___1. Prime the correct tubing and filter with normal saline. ___2. Verify K.L.’s identification with secretary in the endoscopy suite. ___3. Obtain baseline vital signs before starting the transfusion. ___4. Begin the transfusion at a rate of 125 mL per hour. ___5. Take K.L.’s vital signs 30 minutes after starting the transfusion. ___6. Complete the transfusion within 6 hours of receiving the unit.
Emergency Situations
Scenario
Case Study Progress
Case Study Progress
Scenario
Case Study Progress
Case Study Progress
Scenario
Case Study Progress
Case Study Progress
Scenario
Case Study Progress
Case Study Progress
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Emergency Situations
Get Clinical Tree app for offline access
