E
Echocardiogram
Also called: (ECHO); Heart Sonogram; Transthoracic Echocardiogram, Stress Echocardiogram
Basics the nurse needs to know
An echocardiogram is a noninvasive test that uses ultrasound techniques to detect enlargement of the cardiac chambers or variations in chamber size during the cardiac cycle. Even with the advent of CT angiography, the echocardiogram is the gold standard to evaluate heart valves. When echocardiography has been integrated into stress testing, it is called stress echocardiography or exercise echocardiography (see Stress Testing, Cardiac p. 558). It is frequently used for risk stratification and to assess therapeutic outcomes for patients with coronary artery disease. Stress echocardiography is similar to stress testing, but with an echocardiogram being done at baseline and at each progressive level of exertion. It is especially helpful as a screening tool for women and for persons with a left bundle-branch block. If the patient is unable to use the treadmill or bicycle, stress can be induced with dobutamine or dipyridamole. Sometimes atropine is needed to reach the desired heart rate. Dobutamine stress echocardiography (DSE) is frequently used to assess “stunned” or “hibernating” myocardium.
How the test is done
An echocardiogram may be carried out at the bedside, in a special laboratory, in a clinic, or in a doctor’s office. A transducer is placed over the third and fourth intercostal spaces to the left of the sternum. The transducer emits ultrasonic beams of high-frequency sound waves that are inaudible to the human ear. The transducer then picks up the echoes created by the deflection of the beams off the various heart structures. This creates a picture on the oscilloscope. The picture is created because the echo varies in intensity based on the differing densities of the structures.
Electrocardiogram
Also called: (ECG); (EKG); 12-lead ECG or EKG; 15-lead ECG or EKG; 18-lead ECG or EKG
Basics the nurse needs to know
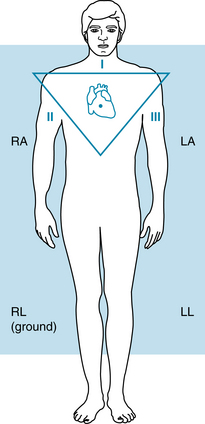
In a 12-lead ECG, leads I, II, and III are limb leads. In lead I, the negative electrode of the electrocardiograph is connected to the right arm, and the positive electrode is attached to the left arm. In lead II, the negative electrode is placed on the right arm, and the positive electrode is placed on the left leg. In lead III, the negative electrode is placed on the left arm, and the positive electrode is placed on the left leg. Leads I, II, and III form a triangle, which is called Einthoven’s triangle (Figure 42).
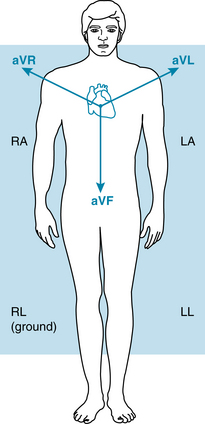
The second set of three leads recorded by the electrocardiograph machine is called the augmented limb leads. In these leads, two limbs are attached to negative electrodes, and a third limb is attached to a positive electrode. If the positive electrode is placed on the right arm, the lead is called aVR (augmented voltage right arm). If the positive electrode is on the left arm, it is called aVL (augmented voltage left arm). When the positive electrode is on the left foot, it is called aVF (augmented voltage foot) (Figure 43).
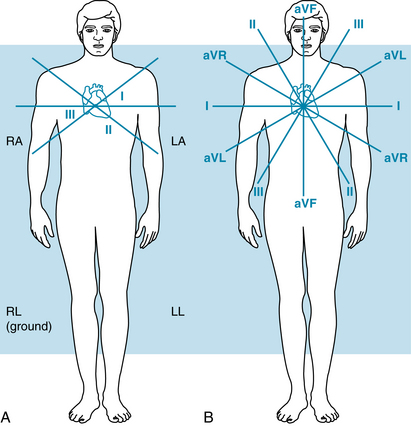
The limb leads and augmented leads are called the standard leads. If one takes the three sides of Einthoven’s triangle and moves them to the center, they form three intersecting lines of reference (Figure 44, A). If one superimposes the augmented limb leads, the lines of reference and the six limb leads form six intersecting lines (one every 30 degrees). Each limb and augmented lead records a different angle and, therefore, a different view of the same electric activity (Figure 44, B).
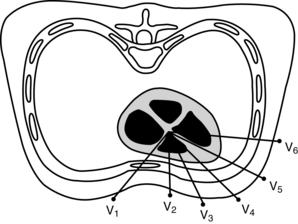
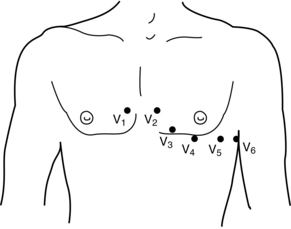
Usually, six chest leads are recorded. This is done by placing the positive electrodes at six different positions across the chest. The chest leads are identified as V1 through V6. The chest leads give various views of the horizontal plane of the left ventricle. The precordial leads can be visualized as spokes of a wheel, the center being the atrioventricular (AV) node (Figure 45).
How the test is done
For a 12-lead ECG, the technician, the physician, or the nurse places the patient in a supine position. Conduction jelly is placed on the electrodes (disposable electrodes already have jelly on the electrode), and the electrodes are applied. The electrocardiograph’s electrode wires are marked and color coded. It is essential that the chest leads be positioned correctly for accurate interpretation.
The chest leads are applied as follows (Figure 46):
With the 18-lead ECG, a 15-lead ECG is taken, and then three chest electrodes are placed on the line level with the fifth ICS at the posterior axillary line (V7). The next electrode is placed at the fifth ICS at the posterior midclavicular line (V8), and the last electrode is placed at the fifth ICS, left of the spinal column (V9).
Significance of test results
Myocardial infarction
Table 8 summarizes which leads reflect which walls of the left ventricle. Note that because leads usually are not placed over the posterior wall of the heart, posterior infarctions are diagnosed by reciprocal changes. Right ventricular infarctions are assessed by performing a right-sided ECG.
Table 8 Electrocardiographic Changes with Acute Myocardial Infarction
| Lead Changes | Reciprocal Changes | |
| Inferior wall | II, III, aVF | I, aVL |
| Lateral wall | I, aVL, V5, V6 | V1, V2, V3 |
| Anterior wall | V2, V3, V4 | II, III, aVF |
| Anteroseptal | V1, V2, V3, V4 | II, III, aVF |
| Posterior wall | V7, V8, V9 | V1, V2 |
| Right ventricular | V4R, V5R |
Electrocardiogram, signal-averaged
How the test is done
The procedure is similar to the 12-lead ECG, except that no limb electrodes are necessary and the six chest electrodes and ground lead are positioned differently on the chest.
Interfering factors
Electroencephalography
Also called: (EEG); Electroencephalogram
Basics the nurse needs to know
Normal EEG recordings are generally rhythmic and have waveforms of similar height and duration. The interpretation of the EEG considers the frequency of the predominant rhythm, the amplitude, any abnormal waves or wave groups, and the asymmetry between the right and left hemispheres.
Interfering factors
NURSING CARE
Pretest
During the test
Electrolytes, 24-hour urine
Includes: Sodium, Urine; Chloride, Urine; Potassium, Urine; Calcium, Urine; Magnesium, Urine
Purpose of the test
Urine electrolytes are used to help monitor renal function, fluid and electrolyte balance, and acid-base balance. The urinary calcium level is used to evaluate bone disease, parathyroid disorders, nephrolithiasis, calcium metabolism, and idiopathic hypercalciuria.
Basics the nurse needs to know
REFERENCE VALUES
Sodium
Male child (6-10 years): 41-115 mEq/24 hr or SI: 41-115 mmol/24 hr
Female child (6-10 years): 20-69 mEq/24 hr or SI: 20-69 mmol/24 hr
Male child (10-14 years): 63-117 mEq/24 hr or SI: 63-117 mmol/24 hr
Female child (10-14 years): 48-168 mEq/24 hr or SI: 48-168 mmol/24 hr
Chloride
Infant: 2-10 mEq/24 hr or SI: 2-10 mmol/24 hr
Male child (6-10 years): 36-110 mEq/24 hr or SI: 36-110 mmol/24 hr
Female child (6-10 years): 18-74 mEq/24 hr or SI: 18-74 mmol/24 hr
Male child (10-14 years): 64-176 mEq/24 hr or SI: 64-176 mmol/24 hr
Female child (10-14 years): 36-173 mEq/24 hr or SI: 36-173 mmol/24 hr
Adult (<60 years): 40-220 mEq/24 hr or SI: 40-220 mmol/24 hr
Potassium
Infant: 4.1-5.3 mEq/24 hr or SI: 4.1-5.3 mmol/24 hr
Male child (6-10 years): 17-54 mEq/24 hr or SI: 17-54 mmol/24 hr
Female child (6-10 years): 8-37 mEq/24 hr or SI: 8-37 mmol/24 hr
Male child (10-14 years): 22-57 mEq/24 hr or SI: 22-57 mmol/24 hr
Female child (10-14 years): 18-58 mEq/24 hr or SI: 18-58 mmol/24 hr
Calcium
Infant and child: 6 mg/kg/day or less or SI: 0.15 mmol/kg/day or less
Adult (normal calcium intake): 100-300 mg/day or SI: 2.5-7.5 mmol/day
Adult (low calcium intake): 50-100 mg/day or SI: 1.25-3.75 mmol/day
Adult (calcium-free diet): 5-40 mg/day or SI: 0.13-1 mmol/day