Chapter 6. Drugs used for blood pressure
LEARNING OBJECTIVES
At the end of this chapter, the reader should be able to:
• describe blood pressure control
• list the causes of hypertension
• give examples of drugs that:
lower total peripheral resistance
lower cardiac output
decrease blood volume
act centrally
• describe the treatment of hypertensive emergencies and hypertension in pregnancy
• discuss the principles and practical aspects of taking blood pressure
• describe the treatment of hypotensive shock and the problems treating peripheral vascular disease
The normal control of blood pressure
The blood pressure depends on:
• the peripheral vascular resistance
• the output of blood from the heart
• the volume and viscosity of the blood.
By changing one or more of these factors it is possible to change the blood pressure.
The peripheral vascular resistance depends on the cross-section of the smaller arteries (arterioles). The walls of these arteries contain circular muscle fibres, which are controlled by the sympathetic nervous system (see p. 40). Stimulation of this system releases noradrenaline, which causes these muscles to contract and leads to narrowing of the arterioles and a rise in blood pressure. As a counterbalance, the cells lining the blood vessels are continually producing nitric oxide, which acts as a vasodilator and thus tends to lower blood pressure. Angiotensin (see below) also causes constriction of blood vessels and a rise in blood pressure.
The output of blood from the heart, or the cardiac output, depends on several factors, but one important control is again the sympathetic nervous system, which, by releasing adrenaline, causes a rise in pulse rate and output of blood.
The volume and viscosity of the blood is ultimately controlled by the kidneys. There are receptors which ‘sense’ changes in the blood volume; if it falls, the kidney secretes a substance called renin, which, via a complex series of changes, leads to retention of salt and water by the kidneys (Fig. 6.1) and the formation of angiotensin II, which causes vasoconstriction, both of which raise the blood pressure.
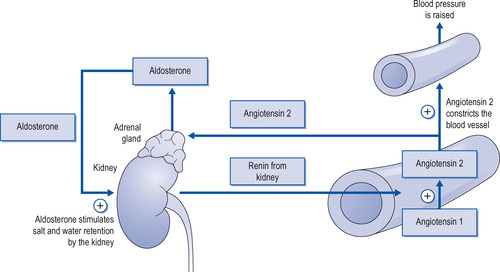 |
| Figure 6.1 Diagram showing how blood pressure is raised and water and salt are converted by the kidneys when blood pressure falls due to the actions of renin, angiotensin and aldosterone. |
In addition to reducing volume, drugs such as the diuretics are used to reduce the body’s stores of sodium, which is believed to contribute to hypertension by increasing blood vessel stiffness, possibly through a sodium–calcium exchange that increases intracellular calcium.
Measurement of blood pressure
When blood pressure is measured, two values are noted: namely, the systolic and diastolic pressures. The systolic pressure is the blood pressure at systole, when the ventricles contract and pump blood into the arterial circulation. Here, the pressure of the pumping heart is a major component of the value recorded. The diastolic pressure is the pressure recorded at diastole, when the heart is filling, and the value obtained reflects predominantly the total peripheral resistance (TPR) in the vascular beds.
Nursing point
Nursing point
TPR, here used as an acronym for total peripheral resistance, is also an acronym for temperature, pulse and respiration.
A typical ‘normal’ value obtained might be, for example, 120/75 mmHg (millimetres of mercury), where 120 is the systolic pressure and 75 is the diastolic pressure. Diastolic values of 90 or more are generally accepted to be a red flag, indicating an abnormally high peripheral resistance. Blood pressures measured during periods of stress will often give spuriously high systolic values and the nurse should be aware of the patient’s state of mind when taking readings.
Hypertension
Hypertension is the term used to describe blood pressure that is chronically raised above acceptable levels for health. In certain people, the blood pressure is consistently raised above normal limits. This is due to a raised peripheral resistance secondary to vasoconstriction, although the kidneys also play a part.
Causes of hypertension
In the majority of patients the cause is not known, although there are probably inherited and environmental factors, and the condition is then called essential hypertension.
Much more rarely, raised blood pressure is secondary to kidney or endocrine disorders. For example:
• phaeochromocytoma, a catecholamine-secreting tumour of the adrenal medulla, which is usually treated surgically by removal of the tumour
• renal artery constriction
• Cushing’s disease (see p. 206)
• primary aldosteronism (see p. 204).
The actual elevation of blood pressure, unless severe, rarely produces symptoms, but over a period of time it damages the brain, heart, blood vessels, retina and kidneys, which leads eventually to coronary thrombosis, heart failure, blindness, strokes and less often to renal failure. It is therefore logical to prevent these complications by lowering the blood pressure and drugs can achieve this.
How drugs can lower blood pressure
Drugs can lower the blood pressure in a number of ways as they can:
• lower the total peripheral resistance
• lower cardiac output
• reduce blood volume and body sodium stores
• act centrally (in the central nervous system).
Drugs which lower total peripheral resistance
• Sympathetic blocking drugs
• Vasodilators
• Angiotensin-converting enzyme (ACE) inhibitors.
Sympathetic blocking drugs
• Prazosin
• Doxazosin
• Terazosin.
Mechanism of action and uses
• Prazosin, doxazosin and terazosin block the vasoconstrictor sympathetic nerve supply to the small arteries and arterioles by blocking α 1 receptors on the blood vessels, and the resulting vasodilatation causes a fall in blood pressure. With these drugs there is little compensatory rise in pulse rate or cardiac output.
• The fall in blood pressure is inclined to be postural (greater on standing than lying).
• Prazosin is short-acting and dosage is required two or three times daily, which makes control of blood pressure difficult. Doxazosin and terazosin have a longer action, so once-a-day dosage is adequate.
• α-Blockers improve the flow of urine in patients with bladder neck obstruction and are used in mild cases of prostatic enlargement. These drugs may be combined with other hypotensive agents. Adverse effects are unusual except for postural hypotension. Occasionally, these drugs cause urinary incontinence, particularly in women.
Vasodilators
Vasodilators comprise the following:
Calcium channel blockers (calcium antagonists)
Mechanism of action
The entry of calcium ions into the muscle cell is necessary for muscle fibres to contract. This group of drugs blocks the entry of calcium ions into the muscle cells in the arterial walls, resulting in relaxation of the muscle and dilatation of the arteries.
Uses
• Calcium antagonists are used to lower blood pressure in hypertension, to dilate coronary arteries in angina (see p. 99) and one calcium antagonist (verapamil; see below) slows conduction in the atrioventricular (AV) node and is used to treat cardiac arrhythmias.
• At present there is no clearly preferred drug for hypertension, although the longer-acting preparations are more convenient for patients.
• Calcium channel blockers may be used alone or combined with other hypotensive drugs; for example, nifedipine plus a β-blocker is a popular combination.
• Although their actions and uses are similar, calcium channel blockers differ in their duration of action. They are all given orally and are broken down by the liver.
Short-acting calcium antagonists used for hypertension or angina
• Nifedipine
• Nicardipine
• Diltiazem.
These need to be administered twice or three times daily.
Long-acting calcium antagonists used for hypertension or angina
• Amlodipine
• Felodipine.
These drugs are usually administered once daily.
Calcium antagonists used for hypertension only
• Isradipine
• Lacidipine.
Calcium antagonist used for hypertension, angina and cardiac arrhythmias
• Verapamil.
Adverse effects of calcium antagonists
• Headache, flushing and ankle oedema due to vasodilatation can occur with all these drugs, but are more common with nifedipine and nicardipine. Verapamil has been reported to cause constipation.
• Depression of cardiac function is bound to be a feature of calcium antagonists since they antagonize the entry of calcium ions into the cardiac muscle cell. This effect is particularly marked with verapamil and to a lesser extent with others. For this reason, verapamil should not be given intravenously to patients receiving β-blockers, since these block the sympathetic cardiac β 1 receptors.
• Great care is necessary if calcium channel blockers are given to patients with heart failure, as this may be made worse.
• There is some evidence of increased mortality in patients taking large doses of the short-acting preparation of nifedipine, particularly in patients with coronary artery disease. The longer-acting preparations appear safe but ACE inhibitors (see below) are to be preferred in hypertensive patients with diabetes.
Drug interactions
The actions of nifedipine and nicardipine are increased by cimetidine, a drug used to treat gastric ulcers (see p. 113).
Diazoxide
Diazoxide is a drug that is chemically similar to the thiazide diuretics (see p. 163), but it has no diuretic activity. It is, however, a potent dilator of arteries.
Mechanism of action and pharmacokinetics
• Diazoxide appears to exert its direct vasodilator effect by opening arteriolar potassium channels, and this has the effect of stabilizing the muscle cell membrane at resting levels.
• Diazoxide is extensively bound to plasma proteins, which extends its half-life in the circulation. It is excreted unchanged.
Uses of diazoxide
• Diazoxide is used to treat hypertensive emergencies.
• It is administered by injection or continuous infusion and is relatively long lasting with a half-life of approximately 24 hours.
• Virtually all patients given diazoxide will respond by the third or fourth dose.
• Diazoxide is extensively protein-bound in the blood, and smaller doses should be administered to patients with renal failure.
Adverse effects of diazoxide
• Diazoxide is potent and can result in excessive hypotension, and caution should generally err on the side of smaller and perhaps more frequent doses. See the British National Formulary (BNF) for dosages.
• The marked hypotensive effect may be accompanied by reflex tachycardia, an increased cardiac output and angina. Patients with ischaemic heart disease may suffer cardiac failure, and the drug should be avoided in these patients.
• Diazoxide inhibits release of insulin from the pancreatic islets, possibly through its action in opening potassium channels. This action of diazoxide renders it generally inadvisable in patients with hyperglycaemia, which is associated with renal failure. This insulin release-inhibiting action makes diazoxide useful in the treatment of hypoglycaemia secondary to an insulinoma.
• Rarely, diazoxide causes salt and water retention.
Hydralazine
Hydralazine is chemically a hydrazine derivative, which has been clinically available for several years.
Mechanism of action and pharmacokinetics
• Hydralazine directly dilates arterioles but not veins to produce its antihypertensive effects.
• The hypotensive action of a given dose becomes successively less effective, a phenomenon known as tachyphylaxis. This limits the sole use of hydralazine for hypotension and it is usually prescribed together with other drugs.
• It is administered orally and is well absorbed but rapidly metabolized during first pass metabolism. This reduces its bioavailability considerably.
• The metabolism of hydralazine is partly by acetylation. The general population consists of those who are either fast or slow acetylators of drugs; therefore, fast acetylators will derive less benefit from a single dose than will slow acetylators.
• The half-life of hydralazine is 2–4 hours, although the hypotensive effect may persist after plasma levels have declined. This is because the drug binds tightly to arteriolar tissue.
Use of hydralazine
• Hydralazine is generally not used alone but in combination with other drugs – for example, β-blockers – to enhance its action and help counteract the reflex tachycardia associated with its use.
• Hydralazine has now been largely replaced by new hypotensive drugs, but is still used in serious hypertension during pregnancy.
Adverse effects of hydralazine
• Nausea, headaches, palpitations (due to reflex tachycardia) and anorexia are the most common side-effects.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
