Chapter 12. Drugs affecting the kidney and renal function
At the end of this chapter, the reader should be able to:
• give a definition of diuretics
• list the factors that cause fluid retention
• describe the basic sites of diuretic action in the nephron
• list the main classes of currently used diuretics
• explain the mechanism of action and uses of the diuretic drugs
• enumerate the risk factors associated with diuretics and potassium loss
• state the three examples of potassium-sparing diuretics
• explain the dangers associated with diuretic use in liver cirrhosis and elderly patients
Introduction to diuretics
Diuretics are drugs that cause increased urine production. They are useful in patients who are suffering from retention of water and sodium chloride (salt), which usually accumulates in the tissue spaces and is called oedema. Note that diuretics are not used in patients who cannot empty their bladders; this is called urinary retention.
Oedema
Oedema occurs most commonly in heart failure, the nephrotic syndrome (severe loss of protein in the urine) and cirrhosis of the liver. Ankle oedema may also develop in individuals sitting with their legs dependent, a common example being elderly people who are confined to their chairs for long periods. It can also complicate the use of calcium channel blockers (see p. 76).
Factors causing fluid retention
The factors that cause fluid retention are various and depend on the underlying disease. They include:
• Lowered cardiac output and underfilling of the vascular system (hypovolaemia), which activates the renin–angiotensin system with increased secretion of aldosterone by the adrenal cortex, leading to salt and water retention by the kidney. This occurs in heart failure, cirrhosis of the liver and the nephrotic syndrome.
• Raised pressure in the veins and capillaries. This leads to increased exudation of fluid from the blood to the tissue spaces, and occurs in heart failure, liver cirrhosis, and oedema due to prolonged immobility with legs dependent.
• Low plasma proteins. This is found in the nephrotic syndrome, where it is due to protein loss in the urine, and cirrhosis of the liver, where there is a failure to make protein.
Renal function
The role of the kidney is to excrete the waste products of metabolism, drugs, etc., and maintain the correct amounts of water and electrolytes in the body by getting rid of any excesses that may be absorbed or produced by the body. This is effected in two stages (Fig. 12.1):
• glomerular filtration
• tubular reabsorption.
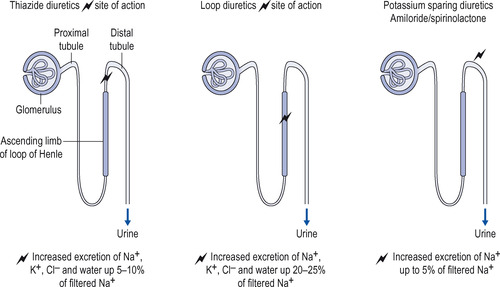 |
| Figure 12.1 Sites of action of diuretics. |
Glomerular filtration
At the glomeruli, water along with soluble substances is filtered from the blood. The volume of this filtrate is about 100 litres of water per day and it contains glucose, electrolytes, urea and other substances.
Tubular reabsorption
In the renal tubules a selective reabsorption occurs. Glucose is normally completely reabsorbed. Water and electrolytes (including sodium, potassium, chloride and hydrogen carbonate) are partially reabsorbed, whereas urea is almost entirely excreted. The exact amount of each substance finally excreted in the urine is controlled so that the composition of the body fluids remains constant.
Diuretic drugs
All diuretic drugs produce their effect by decreasing the reabsorption of water and electrolytes by the renal tubules and thus allowing more water and electrolytes to be excreted. The diuretic drugs fall into various classes, depending on their site and mechanism of action:
• osmotic diuretics
• thiazide diuretics
• loop diuretics
• potassium-sparing diuretics.
Water
It is common experience that, in a normal person, increased ingestion of water results in an increased urine flow. When water is absorbed, it causes the plasma to become more dilute and this in turn decreases the release of antidiuretic hormone (ADH) by the posterior lobe of the pituitary gland (see p. 176). Less ADH reaches the kidney and this causes the tubules to reabsorb less water, so that more is excreted as the urine. In those with fluid retention, for example in heart failure, the normal response to water disappears and so it is of no use as a diuretic under these circumstances.
Osmotic diuretics
Any substance that passes through the glomeruli and is not reabsorbed by the renal tubules will increase the concentration of the urine within the tubules. This prevents the reabsorption of sodium chloride and water from the tubule back into the blood and the water is then passed out and produces a diuresis. Osmotic diuretics are now little used to treat oedema. They are more commonly used during cardiovascular surgery to sustain urinary function. A commonly used example is mannitol.
Mechanism of action
The osmotic diuretics are filtered by the glomerulus and increase the osmotic pressure in the tubules. This inhibits the passive reabsorption of water from the tubules. Water is normally able to pass back into the body from the proximal tubule, the descending limb of the loop of Henle and from the collecting ducts, which are therefore the sites of action of the osmotic diuretics. Some sodium is lost as well, but not enough to make the osmotic diuretics useful in conditions associated with salt retention.
The osmotic diuretics must meet certain criteria for use:
• they must be pharmacologically inert
• they must be freely filterable by the glomerulus
• they must not be reabsorbed from the tubules.
Mannitol
Administration and therapeutic uses
Mannitol and other osmotic diuretics are usually given intravenously. Mannitol is sometimes used:
• during cardiovascular surgical procedures when urine flow through the kidneys needs to be maintained
• to lower raised intracranial pressure after a head injury or in a patient with a cerebral tumour
• to reduce the intraocular pressure in glaucoma.
Adverse effects
These include headache, nausea and vomiting. Osmotic diuretics can cause pulmonary oedema or heart failure in patients who are unable to produce urine.
Thiazide diuretics
Thiazide diuretics comprise:
• bendroflumethiazide (bendrofluazide)
• chlorothiazide
• hydrochlorothiazide
• indapamide
• metolazone
• xipamide
• Chlortalidone.
Clearly there are several diuretics in this group. Although there are marginal differences in their actions, the general pattern of their effects is the same and they will be described together. They are all absorbed from the intestinal tract and are therefore effective orally.
Mechanism of action
The actions of thiazide diuretics on the kidney are:
• There is an increased excretion of potassium by the kidney (see more on potassium secretion below). This takes place because sodium is normally reabsorbed in the collecting ducts in exchange for potassium; therefore, the more sodium is presented to the collecting ducts, the more will be exchanged for potassium, which is excreted.
Therapeutic uses
The therapeutic uses of thiazide diuretics are:




• mild cardiac failure
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
