Chapter 5. Drugs acting on the heart
Cardiac arrhythmias65
The normal cardiac cycle 65
Some useful definitions 66
Disorders of cardiac rhythm 66
Drugs used to treat arrhythmias 68
Vaughan Williams classification of antiarrhythmic drugs 70
Direct current cardioversion 70
Electrolytes and arrhythmias 70
Treatment of individual arrhythmias 71
The Wolff–Parkinson–White (WPW) syndrome 72
Arrhythmias due to conduction defects 72
Newer treatments in the pipeline 72
LEARNING OBJECTIVES
At the end of this chapter, the reader should be able to:
• list the factors that determine cardiac output
• describe the causes and consequences of heart failure
• describe the main approaches to the treatment of heart failure and the major types of drugs used
• give an account of the mechanism of action, use, and the toxic and adverse effects of digoxin
• describe the overall strategies for care as well as drug treatment of patients with heart failure
• give an account of the normal cardiac cycle of the spread of electrical excitability and muscle contraction
• discuss the nature of arrhythmias due to cardiac overexcitability and conduction defects in the bundle of His
• list the names of drugs used to treat different types of arrhythmias, how they are classified and their basic mechanism of action
Drugs can treat two major disorders of the heart. These disorders are:
• cardiac failure
• cardiac arrhythmias.
Cardiac failure
The cardiac output
The heart is a muscular pump receiving blood from the systemic and pulmonary veins and driving it, under pressure, into the pulmonary arteries and the aorta. The volume of blood passing through the heart each minute is known as the cardiac output. This is largely determined by four factors:
• The preload – the pressure in the venous system filling the heart and stretching the cardiac muscle. In health, a rise in venous pressure causes a rise in cardiac output.
• The afterload – the arterial pressure that is the resistance against which the heart must pump.
• The heart rate – an increase in rate leads to an increased output, except in heart failure, when an increased rate decreases cardiac efficiency.
• The contractile efficiency of the cardiac muscle.
In good health, the cardiac output varies considerably depending on the needs of the body, being low at rest and rising with exercise. The healthy heart has a great functional reserve and can cope with demands for increased output that occur from time to time.
Causes of cardiac failure
The contractility of the cardiac muscle is reduced through disease:
• The heart muscle may be damaged by previous coronary thrombosis or by cardiomyopathy.
• High blood pressure or valve disease may cause an increased workload over a long period, which ultimately causes the heart to fail.
Consequences of cardiac failure
• The ventricles fail to empty properly and the heart becomes enlarged.
• The muscle becomes thicker and stiffer and, in diastole, fails to relax completely; thus, filling of the ventricles is diminished.
• The heart and neck veins become distended with blood and cannot respond to the increased filling pressure (preload) by raising output. At first this is only apparent on exercise, but later occurs at rest.
• The pump becomes insufficient for the needs of the body, and various organs receive an inadequate blood and oxygen supply. This is particularly important in the kidney, where it activates the renin/angiotensin system (see p. 74), causing the kidney to retain salt and water.
• Oedema of dependent parts and of the lungs develops, the latter being responsible for marked dyspnoea (shortness of breath), which is a common feature of cardiac failure. Angiotensin is also responsible for arterial constriction, which increases the work (afterload) of an already labouring heart. This is further aggravated by an increase in sympathetic activity, causing additional vasoconstriction and tachycardia.
• The low cardiac output carries less oxygen to the tissues. The oxygen supply to the heart and brain is kept up at the expense of other organs, which are starved of oxygen, and this accounts for the fatigue, which may be a prominent symptom (Fig. 5.1).
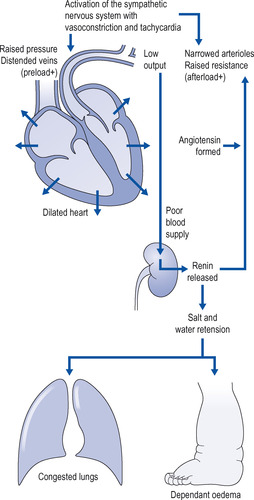 |
| Figure 5.1 Processes in cardiac failure. |
Drugs in congestive cardiac failure
Two main approaches are used, either alone or together:
• increase cardiac contractility
• decrease the workload of the heart.
Five main groups of drugs are used:
• Diuretics, which cause the kidney to excrete excess salt and water (see p. 161).
• ACE inhibitors, which act by suppressing the angiotensin/renin mechanism, which is overactive in cardiac failure. (ACE is the acronym for angiotensin-converting enzyme.)
• Positive inotropic drugs, which are drugs that improve the function of the cardiac muscle so that the heart contracts more powerfully and it empties more completely, thereby raising the cardiac output. This is called a positive inotropic effect.
• Vasodilators, which lower peripheral resistance and thus reduce cardiac work.
• β-Blockers, which reduce inappropriate sympathetic activity.
Diuretics
Diuretics increase urine flow. They are considered in detail on p. 161. Both thiazide and loop diuretics are used in cardiac failure.
Mechanism of action
• They help to get rid of oedema and pulmonary congestion by increasing the excretion of salt and water.
• They relieve distension of the heart by reducing blood volume.
Disadvantages
• Renin release by the kidney is activated by reduced blood volume, and this may partially reverse the diuretic’s beneficial effects by stimulating the kidney to retain fluid.
• Vasoconstriction will occur in response to reduced blood volume, and this will increase the work of the heart.
• Potassium loss: both thiazide and loop diuretics increase potassium loss via the kidney. If small doses are used, this is unlikely to require correction, but can occur if large doses of diuretic are used, if dietary potassium is deficient (e.g. in those whose diet is poor, or in the elderly), or if concurrent digoxin is given.
Nevertheless, the benefits usually outweigh the disadvantages and diuretics are widely used for the relief of chronic cardiac failure. For mild heart failure, thiazide diuretics may be adequate, but more severe heart failure will require a loop diuretic such as furosemide. Non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin will reduce the efficacy of diuretics.
Nursing point
Nursing point
Digoxin is associated with potassium loss. Potassium deficiency increases digoxin toxicity. Supplementary potassium or a potassium-sparing diuretic should be added to the regimen (see p. 166). When patients with heart failure are prescribed thiazides or loop diuretics, the plasma potassium concentration should be monitored and kept above 3.2 mmol/litre.
Angiotensin-converting enzyme (ACE) inhibitors
This group of drugs, which is also used to treat hypertension, has emerged as an important addition to the management of chronic heart failure. ACE inhibitors have considerably improved the treatment of cardiac failure and have prolonged survival.
Mechanism of action
ACE inhibitors block the overactive renin/angiotensin mechanism. This results in a reduction of salt and water retention by the kidneys; in addition, by dilating arterioles, ACE inhibitors lower the resistance to blood flow from the heart (afterload), reduce cardiac work and raise cardiac output.
Disadvantages
The initiation of treatment requires much care. The main danger is a profound fall in blood pressure after the first dose, which is especially liable to occur in patients already taking diuretics, and is due to vasodilatation and a low blood volume resulting from the diuretic treatment.
Nursing point
Nursing point
Nursing point
The initial dose of ACE inhibitor should be low and the blood pressure should be closely monitored (4 hourly) for 24 hours. ACE inhibitors should not be given to patients with renal failure or in pregnancy. Renal function should be measured at regular intervals for those on long-term treatment.
Nursing point
When monitoring the blood pressure following the first dose of an ACE inhibitor, it should be remembered that the fall after captopril only lasts a few hours but that after enalapril may be delayed for up to 8 hours and last up to 30 hours.
Positive inotropic drugs: digoxin
Digoxin is at present the only really effective drug for directly strengthening the heartbeat, but is used more these days to treat arrhythmias. Doctors have used this drug for hundreds of years. In 1785 William Withering of Birmingham described the use of foxglove in dropsy (oedema) and noted that it appeared to act on the heart. Digoxin was originally extracted from the foxglove plant but is now produced synthetically. (In older textbooks, the term ‘digitalis’ is used because it refers to the mixture of active principles extracted from the foxglove plant.)
Mechanism of action
Digoxin has two actions on the heart:
• direct
• indirect.
Direct action
Digoxin acts directly on the heart to strengthen the heartbeat. The strengthening of the heartbeat is called a positive inotropic effect of the drug. Interestingly, these powerful inotropic actions of digoxin are observed only on the failing heart.
Indirect action
At lower doses, digoxin slows the heart through activation of the parasympathetic division of the autonomic nervous system, which slows it down. The indirect action is important, especially in atrial fibrillation, because the slowing of the heart allows for slower and more regular contractions, which increases cardiac output.
Effects of digoxin on the failing heart
• Increased force of contraction of the ventricular muscle (Fig. 5.2). This action is due to an increase in calcium ions in cardiac muscle cells (direct action; see above). In large doses this may be associated with increased excitability of the ventricle.
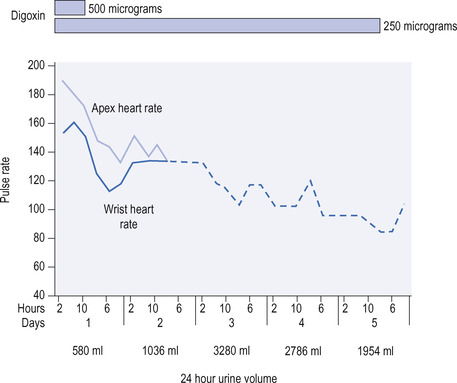 |
| Figure 5.2 The effect of digoxin in a patient with atrial fibrillation and heart failure. Note the difference between the heart rate at the apex and the rate at the wrist due to weak contractions failing to produce a pulse at the wrist. The difference disappears on treatment with digitalis. |
• Depression of conduction in the atrioventricular (AV) node and the bundle of His (Fig. 5.3). This action does not affect the heart in sinus rhythm, but in atrial fibrillation it decreases the number of impulses reaching the ventricles from the fibrillating atria, and thus decreases the rate of ventricular contraction.
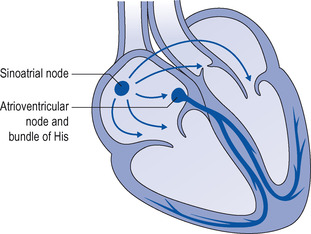 |
| Figure 5.3 The heart, showing the sinoatrial node and conducting system (atrioventricular node and bundle of His). |
• Slowing of the heart rate, partially due to increased activity of the vagus nerve (indirect action; see above) and partly to a direct action on the sinoatrial (SA) node.
Diuretic effects of digoxin
Digoxin may cause a powerful diuresis after administration to patients with heart failure. This effect is not seen in patients with healthy hearts. The diuretic effect is due to the inotropic action of digoxin. In patients with heart failure, the increased preload (venous pressure) pushes fluid out of the capillary beds into the tissues and causes oedema. The restored power of the heart reduces the preload, which in turn allows extravascular fluid to re-enter the circulation and be eliminated through normal fluid control via the kidneys.
Plasma monitoring of digoxin
Plasma levels of digoxin should be monitored, the correct therapeutic range being between 0.9 and 2 micrograms/litre (the sample is taken at least 6 hours after dosing). There is, however, considerable interpersonal variation and the estimation of plasma levels is more useful to confirm non-compliance or overdose than in the control of treatment, where clinical observation is usually adequate. It will be noted that the action of these drugs lasts for several days. This is due not only to slow elimination but also because, once bound to cardiac muscle, their action is prolonged.
Adverse effects and toxicity of digoxin
There is a relatively small difference between the therapeutic dose of digoxin and the toxic dose, i.e. digoxin has a low therapeutic index, so dosage should be carefully regulated. Elderly patients, especially those with renal impairment and with hypothyroidism, are more liable to suffer adverse effects. The nurse should keep a watch for toxicity and should know the common manifestations of overdose:




• Undue slowing of the heart due to excessive effect on the conducting system or the SA node. A pulse rate below 60 indicates that the drug should be omitted for a day or two.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
