Chapter 37 Disturbances in the rhythm of labour
Learning outcomes for this chapter are:
1. To analyse the causes, identification, effects and management of disturbances in the rhythms of labour and birth
2. To critically discuss the evidence that supports common medical interventions in birth
3. To describe the ways in which midwives work to keep birth culturally, emotionally and physically safe when disturbances in the rhythms of labour occur.
absolute cephalopelvic disproportion
cephalopelvic disproportion (CPD)
latent and active phases of labour
The anatomical structures, physiology and biosciences underpinning disturbances in the rhythms of labour are covered only briefly in this chapter. Therefore it is important that readers who may be unfamiliar with these concepts refer to a specialised text such as Blackburn (2007) and/or Stables and Rankin (2005 2nd edn) to enable them to apply this material to the content of this chapter. In addition, Chapter 23 provides an excellent overview of physiological changes during labour.
INTRODUCTION
Many midwives do not subscribe to an interventionist model of maternity care. For example, in New Zealand, the Midwifery Council’s Scope of Practice statement (Midwifery Council of New Zealand 2004) clearly places emphasis on the midwife supporting the physiological processes of normal birthing, and this is evident throughout the Council’s competency requirements for registration as a midwife (Midwifery Council of New Zealand 2007) and the New Zealand College of Midwives’ (NZCOM 2006) Consensus Statement on Normal Birth. Similarly in Australia, one of the cues of Competency Five of the Australian Nursing and Midwifery Council’s Competency Standards for Midwifery is that midwives ‘promote the understanding that childbirth is a normal, physiological process and a significant life event for most women’ (ANMC 2006).
As Powell-Kennedy and Shannon (2004) discovered in a qualitative study, the support of normalcy is fundamental to a midwifery model of care, one that is prefaced by a view that birth for most women should be a normal process (even though some labours are more difficult than others) and that women’s bodies are physiologically prepared for labour and birth (Powell-Kennedy & Shannon 2004). The midwives described to these researchers how they reassured birthing women that even though their labour might be long and painful, it was still normal. Moreover, they ‘embraced a tolerance for wide variations in normal labour and for sustaining as much normalcy as possible, even when pathology had been identified’ (Powell-Kennedy & Shannon 2004, p 256). These midwives believed, as does the World Health Organization (WHO) (1997), that there should always be a valid reason for intervention in the natural process of birth.
A review of the literature concerned with labour and birth reveals that since the 17th century, clinicians have endeavoured to differentiate between a ‘normal’ and an ‘abnormal’ labour and birth. Certainly, the history of midwifery and obstetrics suggests that across time and place, clinicians have created, eliminated and re-worked descriptions of ‘normal’ labour. Many of these are still in use, although they are not supported by scientific or research-based evidence, and more often than not have been created according to the authors’ hunches, opinions, cultural beliefs or convenience. Gross and colleagues (2005) comment on the difficulties associated with determining the precise onset of labour and the duration of each of its phases and stages. As yet there is no consensus about the appropriate length of each stage of labour, or how to differentiate between a ‘normal’ and an ‘abnormal’ labour with its identified risk factors. For instance, despite a paucity of evidence, an unengaged fetal head in a nullipara at the beginning of labour has long been held to be a risk factor for cephalopelvic disproportion (CPD) and therefore is cited as an indication for a ‘trial’ of labour or caesarean section. This is despite research by authors such as Takahashi and Suzuki (1982) and Diegmann et al (1995) who found no significant differences in labour outcomes between nulliparas with an engaged fetal head at the beginning of labour and those with an unengaged fetal head. Similarly, medical and midwifery students are often introduced to notions of specific time intervals expected from each phase of labour, and this knowledge is reinforced by what they see in the hospital environment—even though these are arbitrarily timed. Walsh (2005, 2007) suggests that extraneous factors—a woman-unfriendly birth environment combined with a medical model of practice premised on pathology, and an institutional requirement to keep the birthing assembly line moving—have led to the overdiagnosis of labour ‘dystocia’.
The Greek word for ‘difficult’ or abnormal labour is ‘dystocia’, and this topic is the focus of this chapter. Irrespective of where they practise every midwife will at some time be confronted with complications in labour or deviations from a normal labour. Midwives must know how to recognise these variations and instigate appropriate action until they are resolved, or make a referral and transfer care to a specialist lead carer. Irrespective of the place of birth, the composition of the healthcare team or planned interventions, midwives always work in partnership with each woman to create a space for birth that is culturally, emotionally and physically safe (Powell-Kennedy & Shannon 2004).
Midwives who are evidence-informed and reflective practitioners often find that obstetric interventions such as the induction of labour, especially if there are no accepted medical indications for the procedure, pose ethical and professional dilemmas that need to be addressed. Indeed, the ANMC Code of Ethics for Midwives in Australia (2008) states that ‘midwives have a responsibility not to interfere with the normal process of pregnancy and childbirth unless it is necessary for the safety of the woman and infant(s)’. The NZCOM Consensus Statement (2006) on normal birth recognises that ‘each action the midwife makes, from her first interaction with the woman, needs to support keeping birth normal thereby supporting the normal cascade that occurs when labour and birth happen physiologically. Any and every interaction/decision affects this natural cascade in a positive or negative way.’
RHYTHMS OF LABOUR
Midwives’ and women’s perceptions of the expected length of labour have been seriously undermined by dominant medical hegemony (Bates 2004). This has culminated in the overuse of protocols such as the ‘active management of labour’ and guidelines focused on a predetermined timeline, such as those from the National Institute for Health and Clinical Excellence (NICE 2007) on intrapartum care. Even though authors such as Thornton as early as 1996 argued there was (and still is) scant evidence to support active management of labour, this practice is still used in many maternity units.
REVISION
Before you embark on an exploration of disturbances in the rhythms of labour make sure that you refresh your understandings about what is known about the causes of the onset of labour and its processes (see Stables & Rankin 2005 and/or Blackburn 2007 as well as Chapter 23 of this text).
Box 37.1 Active management of labour
In the late 1970s and early 1980s, two Irish clinicians, O’Driscoll and Meagher (1980), introduced to maternity units in Dublin a ‘package’ of care that they termed ‘active management’, which, they argued, resulted in a reduced incidence of prolonged labour and a caesarean section rate of less than 7%. The package included: antenatal education; one-to-one midwifery care; precise criteria for the diagnosis of the onset of labour; two-hourly timed vaginal examinations; and early use of high doses of synthetic oxytocin (Syntocinon) that achieved a rate of cervical dilation of at least 1 cm/hour.
Across the world this model of care was welcomed and widely accepted. Even today, few randomised studies have evaluated the efficacy of ‘the active management of labour package’. Frigoletto and colleagues (1995) found no significant differences between the ‘active management’ group and a ‘usual-care’ control group in the rate of caesarean sections. However, the median duration of labour was shorter in the ‘active management’ group by 2.7 hours. Nevertheless, the authors concluded that there was no justification for the universal recommendation of ‘active management of labour’. Moreover, beginning in the mid-1980s, research confirmed what midwives intuitively knew—that constant social support during labour is associated with shorter labours, higher rates of vaginal births, and a reduction in the amount of pharmaceutical analgesia used in labour (Hodnett 2003; Klaus et al 1986). In other words, the same outcomes may have been achieved by midwifery one-to-one support without the other arms of the ‘package’.
Critical thinking exercise
The following list identifies the assessments a midwife makes and records in every labour:
• fetal heart rate—by intermittent auscultation, or continuous electronic fetal heart rate monitoring
• cervicogram—rate of cervical dilation and descent of the fetus through the pelvis
• uterine contractions—quantification of frequency, duration and strength
• amniotic fluid (if the membranes have broken)—state of fluid; presence of meconium
• maternal urine production—assessed for the presence of ketones and protein
• maternal adaptation to labour—blood pressure, pulse rate and temperature
• hydration and nutrition—fluid and dietary intake and output
• maternal wellbeing—behaviour and response to labour, levels of fatigue, pain and coping ability
Slower than expected progress in labour, and midwifery support
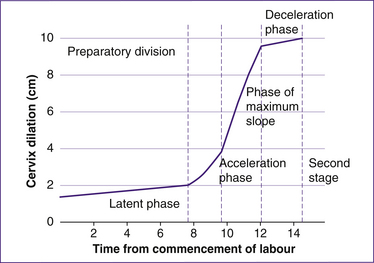
The first clinician to provide a definitive instrument, a cervicograph, for the assessment of individual labours was US obstetrician Emanuel Friedman (1954), and this remained the basis for defining the normal progress of labour until challenged in 1996 (Albers et al). Friedman set the normal progress of labour as a cervical dilation rate of 1.2 cm/hour for primigravidas and 1.5 cm/hour for multigravidas (Friedman 1954). He depicted labour as a sigmoid curve, with the first stage of labour divided into two distinct phases: latent and active (Fig 37.1). The active stage begins at 3–4 cm of cervical dilation and can be further subdivided into three sequential phases: acceleration, maximum slope and deceleration.
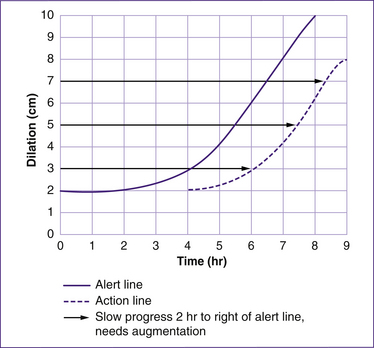
In an attempt to improve maternity outcomes in Rhodesia, Philpott and Castle (1972) refined Friedman’s work. They described the active phase of labour as progressing in a straight line and at a cervical dilation rate of 1 cm/hour, with no distinction for parity. They also placed an alert line on the cervicograph (Fig 37.2). The alert line, unlike the sigmoid curve described by Friedman, was a straight line and was calculated on a rate of cervical dilation of 1 cm/hour irrespective of parity. A second parallel line, known as the ‘action line’, was later drawn on the cervicograph (partogram), four hours to the right of the alert line. Despite the paucity of good-quality research testing these assertions, cervicographs with warning and action lines are still in use in many maternity settings even if there are no indications that maternal or fetal wellbeing is jeopardised.
To date, no trial has demonstrated that the routine use of the partograph/cervicograph has lowered the rate of interventions during labour or has improved outcomes. A 2008 Cochrane review of the routine use of the partogram in labour at term proposes that its contents should rather form the basis of a discussion between women and their clinicians (Lavender et al 2008). Research by Albers (1999) and Zhang et al (2001) have challenged Friedman’s theories on the duration of labour.
Research findings
In the United States, Cesario (2004) conducted a cross-sectional survey aimed at reassessing the average length of each phase of labour associated with a good outcome. The goal was to learn whether there was a consensus among nurses about whether to revise Friedman’s labour curve.
Moreover, Albers and others (Albers 1999; Albers et al 1996) have revealed that normal labour can and does last much longer than is commonly believed. Such labours are not inevitably associated with increased morbidity in mothers or infants. Indeed, the complications often linked to prolonged labours may be caused as much by interventions—repeated vaginal examinations, artificial rupture of membranes (NZCOM 2008), augmentation of labour, epidural analgesia, operative delivery—as by so-called prolonged labours. Of note is an emerging theory that maternal obesity and increasing fetal weight also influence length of gestation and labour without necessarily increasing poor outcomes (Walsh 2007).
Slow progress in the latent phase of labour
During the latent phase of labour, uterine contractions become more regular and increase in intensity; there is slow but gradual cervical dilation. The precise duration of this phase is difficult to determine and probably the best option is to ask the woman when her labour began, and believe her (Walsh 2007). Gross et al’s (2003, 2006) research into the ‘latent’ phase of labour radically challenges the accepted textbook descriptions of how labour begins. Their work established that for less than 60% of women, contractions are the starting point of labour.
Work by Burvill (2002) and Chayne et al (2006) suggests that there are multiple factors that influence midwives’ decisions about determining when labour starts—workloads, guidelines and protocols, risk-management strategies, the need to justify actions to others, institutional constraints and the desire to provide a degree of continuity of care; all of which interfere with the woman’s validation of her lived experience.
Women empowered to take control of their birth experience will alert the midwife of changes in their labour and are best placed to determine whether they are ‘in’ or ‘not in’ labour. Indeed, Walsh (2003, 2007) makes the point that in a partnership of reciprocal respect and trust, women’s fear of intervention during the usual ebb-and-flow patterns of labour can be minimised.
Slow progress in the active phase of labour
According to traditional medical dictum based upon Friedman’s concepts from his research, the validity of which have been subsequently disputed, the active phase of labour is characterised by increasing frequency and intensity of contractions, progressive descent of the presenting part and dilation of the cervix of 1 cm/hour. It covers the period from the end of the latent phase (3–4 cm of cervical dilation) to complete dilation of the cervix (10 cm of cervical dilation). Figure 37.2 shows how a partogram is used to plot the expected progress of labour and the typical pattern of prolonged labour based on Friedman’s ‘ideal’ of normal labour. On the other hand, using Alber’s work (1999) as a guide, the usual rate of cervical dilation in this stage for nulliparas is 0.5 cm/hour in the absence of complicating factors, and the mean duration of active labour is 7.7 hours. For the duration of labour, the upper limit is 17.5 hours. In multiparas the mean duration is 5.6 hours and the upper duration 13.8 hours. Thus there are wide variations in the duration of women’s labours, and these do not fit the expected Friedman-style pattern.
A misdiagnosis of slower than expected labour progress in the active phase can lead to unnecessary obstetric intervention, such as augmentation of labour using oxytocic drugs and artificial rupture of the membranes (ARM). Empowered, knowledgeable women will alert the midwife to an apparent slowing-down in the pattern of contractions once labour has established. Midwives do not need to perform two- to four-hourly vaginal examinations to assess the progress of labour unless there is good evidence that progress has halted. Less-invasive methods to determine the progress of labour include the evaluation of contraction patterns by gentle abdominal palpation to track the descent of the fetus through the birth passage, combined with careful assessment of the strength, regularity and duration of contractions and are effective techniques. However, these assessments are also subjective, and should always be considered along with the patterns in the woman’s behaviour and her reactions to each contraction. Findings are confirmed by vaginal examination if necessary. The pattern of contractions can be altered by factors that include fear, anxiety and uncontrolled pain rather than problems in what are often called the ‘passages—disproportion between the pelvis and the fetus’. Maternal fears about transfer to hospital will often slow labour down. Similarly, labour often slows just before the second stage of labour begins, probably to give the mother a much needed rest before the work of the second stage begins.
MATERNAL DEHYDRATION, KETOSIS AND THE PROGRESS OF LABOUR
Labour is hard work, and the body needs energy to work effectively. However, in industrialised countries, the costs and benefits of restricting fluids and food in labour remain controversial issues. Restricting women’s oral intake to fluids or ice chips during labour is a widely accepted obstetric tradition, which began about 50 years ago when women frequently gave birth under general anaesthesia and were therefore at risk of aspiration pneumonia (Mendelson’s syndrome). However, modern anaesthesia has improved, and in any case general anaesthesia is rare in 21st century obstetrics. Moreover, no period of fasting guarantees an empty stomach, and clear liquids leave the stomach almost immediately. Some authors argue, with scant evidence to support their hypothesis, that fasting increases ketosis and dehydration, which leads to more painful contractions, slower labours and fatigue. However, preventing the woman from meeting her body’s calorific requirements and consequent suboptimal functioning of vital organs caused by fasting may slow the progress of labour. In addition, the effect of malnourishment on the woman’s psyche needs to be addressed. A woman in active labour requires up to 47 kCal/hour (197 kJ/hour) to prevent ketosis (Hall et al 2006) (see Ch 21). Routine administration of intravenous fluids to reduce ketosis is not supported by evidence (Hall et al 2006). Administration of intravenous glucose to women in labour risks fluid overload and lactic acidosis in the mother and hyponatraemia in the fetus (Ames et al 1975). For these reasons, many healthcare providers no longer restrict eating and drinking during a normal labour or routine IV fluid infusions. Nonetheless, some studies have shown that eating food during labour is likely to increase the duration of the labour (Parsons et al 2007).
Sports medicine isotonic calorific drinks (e.g. Gatorade® 105 kJ/100 mL) administered in labour reduce the incidence of ketosis without increasing gastric volume (Kubli et al 2002).
ANXIETY AND FEAR
The relationships between continuous support in labour, fear, anxiety and the progress of labour are described elsewhere in this text (e.g. Ch 22). In brief, anxiety, excessive pain and fear increase the amount of catecholamines (‘fight-or-flight’ hormones) released into the maternal circulation, and these influence the effectiveness of uterine contractions. For centuries, midwives and women have known that uncontrollable anxiety and fear increase the pain of labour and inhibit its progress. There is now qualitative and quantitative evidence to support this ancient knowledge. Moreover, we now know that women who feel in control of their bodies, their labour and what is happening to them are less likely to experience uncontrollable pain (Hunter 2002). Women who experienced sexual abuse in childhood or have had prior traumatic birth experiences, or have strong ‘control’ issues, may sometimes have difficulty surrendering to the power of their labour (Hofberg & Brockington 2000; Sjogren & Thomassen 1997). Indeed, maternal fear of childbirth is the most common reason for nulliparous women’s request for caesarean delivery (Hildingson et al 2002). Women with extreme fear of labour (tocophobia) may develop post-traumatic stress disorder if they feel ‘forced’ to go through vaginal birth, but may benefit from counselling or psychiatric consultation (Hofberg & Brockington 2000).
Clinical point
Strategies to prevent, or support women in dealing with, anxiety and fear in labour are:
• one-to-one midwifery care in which a trusting relationship has been established
• eating and drinking to avoid fatigue and dehydration, which may slow labour
• massage, acupressure and warm tub baths or showers to ease pain and induce relaxation, which may enhance progress
• warm water immersion, which has been called the ‘midwives’ epidural’
• talk, which provides comfort, reassurance and encouragement, and aims to relieve anxiety and explore the psychological or emotional issues or adverse environmental elements that might be causing the ‘slow’ labour.
INEFFECTIVE CONTRACTION PATTERNS
Incoordinate uterine action
Incoordinate uterine action is characterised by asynchronous, hypotonic or hypertonic uterine contractions, which, because they do not begin in the uterine fundus and do not pass in a wave downwards to the cervix, result in ineffective contractions. It is associated with frequent, painful contractions often combined with constant backache and pain that persists well after the contraction has finished. There is a loss of fundal polarity, and in hypertonic incoordinate uterine action there is an increased uterine resting tone. Consequently, placental blood flow is reduced and fetal compromise may occur (Liu et al 2003). Two variations of hypertonic incoordinate uterine activity are the so-called ‘colicky uterus’ and ‘constriction ring dystocia’. In the former, various parts of the uterus contract independently and this is combined with generalised and severe pain. An extreme form of incoordinate uterine action occurs with a localised spasm of one part of the uterus. However, constriction ring dystocia is rarely seen in developed countries. In association with ineffectual uterine contractions it occurs when an annular spasm arises at the junction between the upper and lower uterine segment, usually in late first stage or early in the second stage of labour. Unlike Bandl’s pathological retraction ring, constriction rings are not associated with obstructed labour and cannot be palpated abdominally (see Table 37.1). Often, constriction rings arise from injudicious use of oxytocin or during intra-uterine manipulation such as an internal podalic version. Relaxants, including inhalation of amyl nitrate, terbutaline or deep anaesthesia with a drug such as halothane, may eliminate the localised myometrial spasms, but as a last resort caesarean section with a vertical incision may be required.
Table 37.1 Patterns of incoordinate uterine action
| Bandl’s pathological retraction ring | Constriction ring |
|---|---|
| Primarily occurs in second stage | Occurs in the first, second or third stage |
| Always occurs at the junction of the thinned lower uterine segment and the thick retracted upper uterine | Occurs at any level of the uterus |
| Rises up cephalad | Does not change its position |
| Felt and seen abdominally | Felt only vaginally |
| Uterine pain is constant and the fetal parts cannot be felt | The uterus is not tonically retracted and the fetal parts can be felt |
| Maternal distress and evidence of fetal compromise or death | Maternal and fetal compromise may not be present |
| Relieved only by delivery of the fetus (caesarean section) | May be relieved by anaesthetics or antispasmodics |
Hypotonic uterine contractions
Ineffective contractions are commonly associated with a poorly fitting presenting part on the cervix. Hypotonic uterine action (contractions are short in duration and of weak intensity) result in a slower than expected rate of cervical dilation and in prolonged labour. The pattern may occur in early labour (primary), or later after a normal contraction pattern has been established (secondary). Typically this pattern is observed after the administration of epidural or narcotic analgesia, but is frequently associated with some degree of cephalopelvic disproportion. There is also evidence that women are genetically predisposed to hypotonic uterine action (Dizon-Townson & Ward 1997). Once the presence of factors that preclude the use of oxytocics are eliminated, many clinicians advocate augmentation of labour with an artificial rupture of membranes (ARM) and oyxtocin (Syntocinon) infusion. However, studies of the effectiveness of amniotomy have not demonstrated that it significantly improves outcomes or reduces the duration of labour (Andress & Rankin 2007).
Hypertonic uterine contractions
A precipitated labour is defined as one with a total duration of less than two hours. For some women this may be their normal pattern, but the most common cause of hypertonic uterine action is the injudicious use of oxytocic drugs. Fetal welfare may be compromised when the intensity of uterine contractions is increased, resting intervals are shortened and the duration of the contractions is increased. Hypertonic contractions may also cause maternal trauma—including uterine rupture or perineal damage. A combination of excessively forceful uterine contractions and minimal soft-tissue resistance can give rise to precipitate labour, fetal anoxia and cerebral trauma, maternal lacerations, and postpartum haemorrhage caused by uterine atony. Early recognition of the problem, timely preparation for birth under controlled conditions, and properly administered analgesia or anaesthesia may minimise these risks.
Working with women experiencing ineffective contraction patterns
Walsh (2007) suggests that a greater understanding of labour physiology and hormonal control, referred to as the ‘dance of labour’ (Buckley 2004), enables midwives to appreciate the purpose of an apparent imbalance in endogenous oxytocin release during labour. A longer than expected labour for the woman and her birth supporters can affect her ability to cope, leading to an increased release of catecholamines (stress hormones), which causes the labour to slow. The midwife will need to use all her skills in supporting women in a long labour, in particular taking care to avoid maternal dehydration and moderate ketosis, which is best determined by documentation of fluid input and output and urinalysis. Ketosis and dehydration may exacerbate ineffective contraction patterns and dysfunctional labour (Newton & Raynor 2000). However, gastric emptying (increasing the risk of aspiration) is delayed in women who receive more than 100 μg fentanyl by epidural infusion (Porter et al 1997).
It is important for the woman to avoid a full bladder because this may inhibit descent of the presenting part into the pelvis and delay the second stage of labour, and potentially result in a postpartum haemorrhage. Observation and assessment of the rhythms of normal labour are useful to detect the onset of complications. Simple measures such as midwives encouraging the woman to ambulate, frequent changes of position, creating a restful birthing environment and the presence of supportive birth companions assist the birth process (Deakin 2001). Research by authors such as Cluett et al (2004) indicates that labouring in water may alleviate the effects of dystocia.
Research findings
Obesity and anaesthesia
‘Obesity’ featured prominently in the most recent CEMACH report (Lewis 2007), concerning respiratory problems following anaesthesia which resulted in maternal death. While aspiration was not cited as the direct cause of death in these particular cases, with a greater risk of airway problems in obese mothers, aspiration is a significant danger. It is noteworthy that the body mass index (BMI) of women described in this report is by current norms relatively low, with 27% of mortalities involving a BMI of only 30 or greater.
Moreover, fasting, enforced bed rest, intravenous therapy and continuous electronic fetal monitoring imply notions of loss of control, sickness and helplessness, which may also interfere with the progress of labour and necessitate intervention such as augmentation of labour, epidural analgesia and operative delivery (Broach & Newton 1988).
Collaborative interventions
The primary goal of all clinicians working with women as they labour is to provide the safest outcome for both mother and infant. It is crucial that midwives have the skills and knowledge required to assess labour and contraction patterns that pose risks for the mother and fetus. Once dystocia is recognised, it is important to identify its cause and, if possible, correct it or minimise the harmful effects it may have on the mother and her baby, treating the causes of the dystocia in partnership with the woman. Frequently, dystocia can be relieved by simple measures such as alleviating intolerable pain. In most cases this will include transferring primary care to a multidisciplinary team. The lead midwife should avail herself of support from her back-up midwife in primary settings or support from the midwifery staff in secondary/tertiary hospitals, so that the lead carer can take regular breaks and have adequate rest while continuing to provide continuity of care in partnership with the woman (NZCOM 2005).
Amniotomy (artificial rupture of membranes)
For most women, once labour has been established, it advances without medical intervention. Artificial rupture of membranes (ARM) is a surgical intervention and thus requires the woman’s consent. As Vincent (2005) suggests, this seemingly ‘routine’ procedure may not always be beneficial and has associated risks. According to the latest available evidence, ARM is no longer recommended as a routine practice for shortening spontaneous labour (Smyth et al 2007). In this review, amniotomy was associated with an increased risk of delivery by caesarean section compared with women in the control group, although the difference was not statistically significant. Neither was there any statistical difference in length of the first stage of labour, maternal satisfaction with childbirth experience, or Apgar scores less than 7 at five minutes. Consequently,
the New Zealand College of Midwives (2008) does not support the use of routine ARM if labour is progressing physiologically. Until recently, early amniotomy was advocated as a component of the active management of labour, to accelerate the progress of labour by increasing the frequency and quality of contractions (Fraser et al 1999).
Complications of ARM
As soon as the membranes are ruptured there is an increased risk of umbilical cord prolapse, fetal compromise and chorioamnionitis. Once an ARM has been performed, birth should occur within 24 hours. Pre-labour rupture of the membranes at or near term (term PROM) increases the risk of infection for the woman and her baby. The routine use of antibiotics for women at the time of term PROM may reduce this risk. However, a systematic review (Flenady & King 2002) found that the use of antibiotics resulted in a statistically significant reduction in maternal infectious morbidity (chorioamnionitis or endometritis), but no statistically significant differences were shown for outcomes of neonatal morbidity. The authors caution that no clear practice recommendations can be drawn from the results of this review because of the paucity of reliable data. Nonetheless, many clinicians still prescribe intravenous antibiotics if the membranes are ruptured for more than 12 hours; this is not common practice in New Zealand hospitals. If the baby is at risk of infection from Group B Streptococcus (NZCOM 2008), intravenous antibiotics are recommended after rupture of membranes for longer than 18 hours.
The amniotic sac and its liquor protect the fetal head; once the membranes rupture, this effect is removed. Compression of the fetal head leads to increased moulding and changes in the fetal heart rate—variable decelerations are often apparent on the electronic fetal heart rate trace because the fetal head is no longer cushioned by the amniotic fluid (Vincent 2005).
Fetal risk factors:
Contraindications for amniotomy
• Presentation unknown or unstable.
• Non-vertex position of the fetal head.
• Woman refuses the procedure.
Clinical point
Before performing an ARM, the midwife:
• ensures the woman has consented to the procedure
• ensures that there is indication for the intervention and no contraindications
• performs an abdominal palpation and vaginal examination to determine the stage of labour, presentation, position, cervical dilation and position of the fetal head relative to the ischial spines
• during a vaginal examination, assesses the progress of labour by cervical dilation. Unless the fetal head is well engaged in the pelvis, ARM is not advocated.
• introduces the amniohook through the cervix and makes a small tear in the membranes lying in front of the fetal head.
After the procedure, the midwife:
Augmentation of labour with synthetic oxytocin
Labour augmentation usually involves the stimulation of uterine contractions to hasten birth after the onset of labour as well as ARM. However, at least 10% of women are diagnosed with ‘prolonged’ labour and about 40% to 60% of these women have their labour augmented with oxytocin (Syntocinon) due to slow progress or other reasons in the first stage of labour (Impey et al 2000).
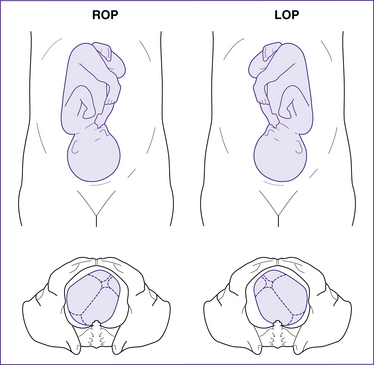
MALPOSITION
There is only one malposition—an occipitoposterior (OP) position of the fetus (Fig 37.3). In about 10%–25% of pregnancies, the fetal head enters the maternal pelvis with the occiput lying in the posterior segments of the pelvis. In most cases the architecture of the pelvis is normal, but in others the pelvic diameters may be reduced. OP positions are more common in the presence of long, narrow pelvic walls (oval-shaped pelvis) or with convergent pelvic side walls and prominent ischial spines. For the baby lying in a right occipitoposterior (ROP) position to rotate to a right occipitoanterior (ROA) one, the head must rotate 135° from an ROP to a right occipitolateral (ROL), then to ROA and then, as the head begins to birth, to a direct OA (DOA). Thus, lengthy labours are associated with an OP position. In nearly two-thirds of cases, the fetal head spontaneously achieves this rotation. However, in about 15% of cases the fetal attitude is one of deflexion, and the sinciput becomes the denominator. If this happens, the sinciput, not the occiput, rotates to the front of the pelvis so that the fetal head completes a short rotation of 45° and the head is born ‘face-to-pubes’. With a deflexed fetal head, the presenting diameter is 12.5 cm—much larger than the 9.5 cm of the suboccipitobregmatic diameter of the well-flexed head, and so as the head births there is a much higher chance of perineal lacerations. In 20% of cases the fetal head attempts the ‘long rotation’ but arrests at the level of the ischial spines—known as deep transverse arrest.