Chapter 6 Dialyzers, dialysate, and delivery systems
Parallel plate dialyzers
What are characteristics of parallel plate dialyzers?
Parallel plate dialyzers are assembled in layers, like a sandwich. Sheets of membrane are placed between supporting plates, which have ridges, grooves, or crosshatches to support the membrane and allow the flow of dialysate along it. The blood flows through the sheets of the membrane. The contained volume of blood is small, and heparin requirements are also usually small. A disadvantage of parallel plate dialyzers is that they are compliant. This means that the volume of blood that they hold increases as the transmembrane pressure (TMP) increases. The main disadvantage of parallel plate dialyzers is that they are not well suited for reuse.
Hollow-fiber dialyzers
What serves as the semipermeable membrane in the hollow-fiber artificial kidney?
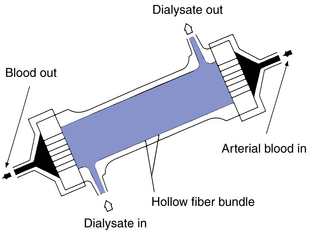
Tiny hollow fibers of about 150 to 250 μm in diameter are used. Blood flows through these tens of thousands of hollow fibers. They are formed from a variety of materials, both cellulosic and synthetic. Wall thickness may be as little as 7 μm, although some synthetics have walls of 50 μm or more (Fig. 6-1).
What are disadvantages of the hollow-fiber artificial kidney?
Meticulous deaeration of the fiber bundle is required before beginning a dialysis procedure. Otherwise, fibers may air lock and not admit blood. There may be uneven distribution of blood at the inflow header space, with reduced perfusion of some of the center fibers. Hollow-fiber dialyzers may be sterilized with ethylene oxide (ETO). Residual toxic products of ETO sterilization retained in the potting material of the headers can cause adverse patient reactions. Patient may require higher heparin doses to keep hollow fibers from clotting.
Membranes for hemodialysis
What are some cellulosic membranes now used in hemodialysis?
Cuprophan has been widely used. The cellulose is treated with ammonia and copper oxide during manufacture; cuprammonium rayon and Hemophan are modifications. Saponified cellulose ester, cellulose acetate, and triacetate are other widely used cellulose materials.
What are negative aspects of synthetic membranes?
Synthetic membranes have several negative aspects, including the following:
• They are expensive in comparison with cellulosic membranes.
• Automated ultrafiltration control is required because of the very high water permeability.
• Adsorption of proteins to the membrane surface can be a problem.
• The high permeability creates a risk of backfiltration from dialysate to blood.
Membrane biocompatibility
How does one measure the level of inflammatory response resulting from blood-membrane interaction during hemodialysis?
The intensity of the reaction is measured by the level of complement generation following initiation of hemodialysis. Markers used to evaluate complement activation are C3a, C5a, and the “membrane attack complex”—C5b through C9—in the patient’s blood.
Which membranes induce the highest levels of complement activation?
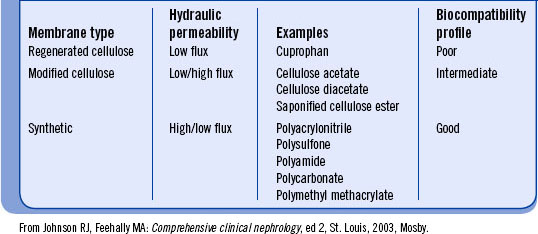
Cellulose and cellulose-based membranes induce more complement activation than do synthetic membranes (Table 6-1). The chemical composition of the cellulosic surface is similar to that of the cell wall of bacteria: both are chains of polysaccharide structures. The body responds to blood-cellulose contact in much the same way as it does to invasion by bacteria. Free hydroxyl groups on the membrane surface are likely the primary source of the intense complement activation. Chemical alterations to buffer the free hydroxyl groups are used to create “modified cellulosic membranes,” such as cellulose acetate and Hemophan. Membranes of cellulose acetate have some of the surface hydroxyl linked with acetyl groups. Hemophan membranes have amino groups attached to the reactive sites to buffer them. Both of these modifications reduce the amount of complement generated; however, these membranes are still less effective than synthetic membranes in minimizing complement production.
What are some of the long-term considerations when selecting a membrane for hemodialysis?
Malnutrition is a major contributor to morbidity and mortality of patients on hemodialysis. Even with adequate protein intake, malnutrition is a problem and seems to relate to an accelerated catabolic process, most evident on dialysis days. A catabolic effect associated with bioincompatible membrane is well documented. However, recent studies have demonstrated an increase in protein catabolism during hemodialysis with synthetic membranes as well (Ikizler et al., 2002). β2AD is important in long-term morbidity. Clinical manifestations include arthropathies, bone lesions and pathologic fractures, soft tissue swelling, and carpal tunnel syndrome. Patients being dialyzed with cellulosic bioincompatible membranes exhibit more pronounced clinical symptoms of amyloidosis (Schiffl et al., 2000). Possible reasons for the difference include the following:
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree