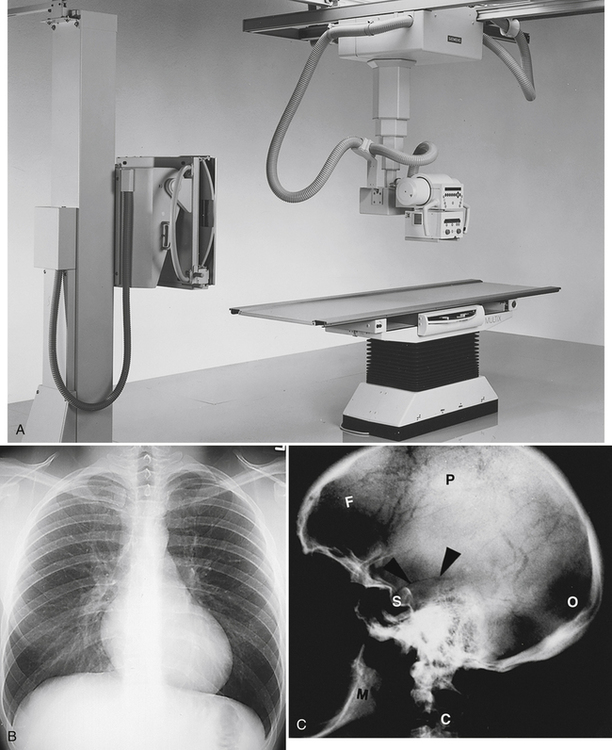
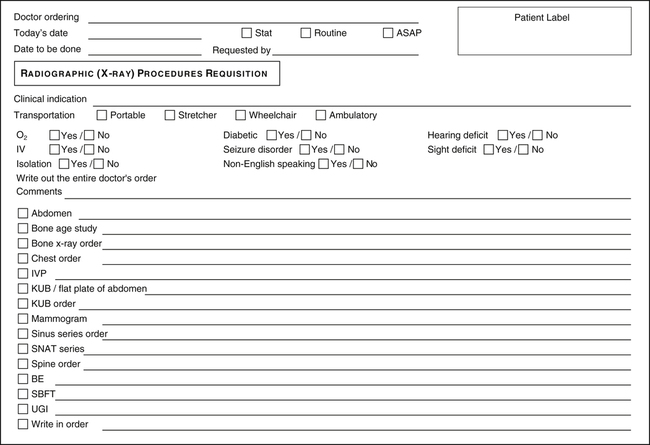
On completion of this chapter, you will be able to: 1. Define the terms in the vocabulary list. 2. Write the meaning of the abbreviations in the abbreviations list. 3. Explain how the health unit coordinator’s responsibilities regarding diagnostic imaging orders differ with the implementation of the electronic medical record and computer physician order entry versus use of the paper chart. 4. List the information regarding the patient that the health unit coordinator must include when ordering procedures to be performed by the diagnostic imaging department. 5. Explain the respective roles of a radiographer and a radiologist. 6. Explain the benefits of picture archiving and communication systems for the patient and the doctor. 7. Name five patient positions that may be included in a diagnostic imaging order. 8. Identify diagnostic imaging orders that do not require routine preparation. 9. Explain when a patient would be required to sign an informed consent before a diagnostic imaging procedure. 10. Explain why contrast media are used, and list types commonly used. 11. Discuss sequencing or scheduling of multiple diagnostic imaging procedures ordered for the same patient. 12. Identify four diagnostic imaging procedures that would require routine preparation, and explain the importance of preparing the patient before these procedures. 13. Explain the purpose of special invasive x-ray and interventional procedures, and list at least three procedures performed in this division of the radiology department. 14. Describe an instruction the doctor would include when ordering computed tomography (CT), and list at least three CT procedures. 15. Describe the purpose of ultrasonography procedures, and list at least three procedures performed in the ultrasonography department. 16. Discuss the purpose of magnetic resonance imaging (MRI) procedures and the purpose of magnetic resonance angiography (MRA) procedures. 17. Discuss the importance of a patient’s nurse completing the interview form before the patient undergoes MRI or MRA, and list contraindications that would exist for patients because of the strength of the magnet. 18. Discuss the purpose of nuclear medicine procedures, and list at least three nuclear medicine procedures. A mobile fluoroscopy unit used in surgery or at the bedside. An agent that causes evacuation of the bowel (laxative). Use of a digital imaging plate rather than film. Magnetic Resonance Angiography Use of magnetic resonance to study blood vessels. The process by which tumor cells spread to distant parts of the body. A branch of medicine that uses radioactive isotopes for the diagnosis and treatment of disease. Picture Archiving and Communication Systems (PACSs) An x-ray study taken with a mobile x-ray machine that is moved to the patient’s bedside. The process of obtaining film records (radiographs) of internal structures of the body. Special Invasive X-ray and Interventional Procedures The diagnostic imaging department may also be called medical imaging. Many modalities, including radiography, nuclear medicine, ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI), are included in the diagnostic imaging department. Diagnostic imaging procedures are performed to diagnose conditions and/or diseases (or to rule them out) and to assist the doctor in determining treatment. When the electronic medical record (EMR) with computer physician order entry (CPOE) is implemented, the doctors’ diagnostic imaging orders are entered directly into the patients’ EMR and are automatically sent to the diagnostic imaging department. When paper charts are used the diagnostic imaging orders are communicated by the ordering step of transcription via computer or by completion of a downtime requisition form (Fig. 15-1). Because the patient usually is transported to the diagnostic imaging department for the procedure, it is important to indicate the mode of transportation—wheelchair or gurney (stretcher). The patient may be transported by the diagnostic imaging department staff, transport service, or nursing department staff. When ordering the diagnostic procedure, indicate the following information about the patient: • reason for procedure (clinical indication) • whether patient is receiving intravenous fluids • whether patient is receiving oxygen • whether patient needs isolation precautions • whether patient has a seizure disorder • if patient does not speak English • whether patient is sight or hearing impaired • whether patient is pregnant or if pregnancy test results are pending This information will assist personnel in the diagnostic imaging department to provide better care for the patient (see Fig. 15-1). The doctor may write the name of the radiologist who will perform an invasive procedure. The health unit coordinator (HUC) should include this information when entering the order or scheduling the test. Following is a list of the positions used most frequently in the writing of x-ray orders: • AP position: This view may be taken while the patient is standing or lying on the back (supine); the machine is placed in front of the patient. • PA position: This view may be taken while the patient is standing or lying on the stomach (prone) with the x-ray machine aimed at the patient’s back. • Lateral position: This view is taken with the patient standing or lying on the side. • Oblique position: This picture is taken with the patient standing or lying halfway on the side in the AP or the PA position. • Decubitus position: In this view, the patient is lying on the side with the x-ray beam positioned horizontally. X-rays can penetrate solid material, such as bone; this in turn produces a shadow that is recorded on film. Procedures that require the filming of bone structures or that are ordered to determine the position of other organs in relation to these structures can be performed by qualified radiology personnel without the need for preparation for the procedure (Fig. 15-2). Following are x-ray studies as they commonly are written on a doctors’ order sheet.
Diagnostic Imaging Orders
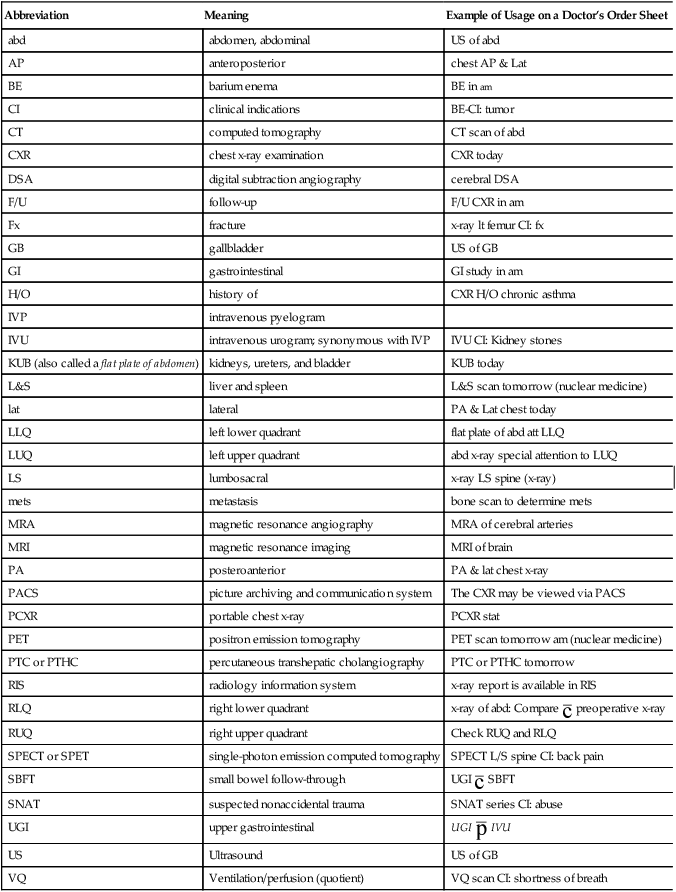
Abbreviation
Meaning
Example of Usage on a Doctor’s Order Sheet
abd
abdomen, abdominal
US of abd
AP
anteroposterior
chest AP & Lat
BE
barium enema
BE in am
CI
clinical indications
BE-CI: tumor
CT
computed tomography
CT scan of abd
CXR
chest x-ray examination
CXR today
DSA
digital subtraction angiography
cerebral DSA
F/U
follow-up
F/U CXR in am
Fx
fracture
x-ray lt femur CI: fx
GB
gallbladder
US of GB
GI
gastrointestinal
GI study in am
H/O
history of
CXR H/O chronic asthma
IVP
intravenous pyelogram
IVU
intravenous urogram; synonymous with IVP
IVU CI: Kidney stones
KUB (also called a flat plate of abdomen)
kidneys, ureters, and bladder
KUB today
L&S
liver and spleen
L&S scan tomorrow (nuclear medicine)
lat
lateral
PA & Lat chest today
LLQ
left lower quadrant
flat plate of abd att LLQ
LUQ
left upper quadrant
abd x-ray special attention to LUQ
LS
lumbosacral
x-ray LS spine (x-ray)
mets
metastasis
bone scan to determine mets
MRA
magnetic resonance angiography
MRA of cerebral arteries
MRI
magnetic resonance imaging
MRI of brain
PA
posteroanterior
PA & lat chest x-ray
PACS
picture archiving and communication system
The CXR may be viewed via PACS
PCXR
portable chest x-ray
PCXR stat
PET
positron emission tomography
PET scan tomorrow am (nuclear medicine)
PTC or PTHC
percutaneous transhepatic cholangiography
PTC or PTHC tomorrow
RIS
radiology information system
x-ray report is available in RIS
RLQ
right lower quadrant
x-ray of abd: Compare  preoperative x-ray
preoperative x-ray
RUQ
right upper quadrant
Check RUQ and RLQ
SPECT or SPET
single-photon emission computed tomography
SPECT L/S spine CI: back pain
SBFT
small bowel follow-through
UGI  SBFT
SBFT
SNAT
suspected nonaccidental trauma
SNAT series CI: abuse
UGI
upper gastrointestinal
UGI  IVU
IVU
US
Ultrasound
US of GB
VQ
Ventilation/perfusion (quotient)
VQ scan CI: shortness of breath
Communication with the Diagnostic Imaging Department
Patient Positioning
Radiographic (X-ray or General Diagnostic ) Procedures
X-ray Examinations that Do Not Require Preparation (Plain Radiographs or Plain X-ray Images)
Diagnostic Imaging Orders
Get Clinical Tree app for offline access