Chapter 16 Diabetes and hemodialysis
More than 23.6 million people, or 7.8% of the population, in the U.S. have diabetes (National Diabetes Information Clearinghouse, 2007). Diabetes mellitus continues to be the leading cause of chronic kidney disease (CKD) in this country; however, the rate has slowed considerably since the mid-1990s. The most recent data show that, in 2007, 108,891 new patients entered the end-stage renal disease (ESRD) program, and 527,283 were under treatment on December 31 of that year. Medicare was providing renal replacement therapy for 47,778 diabetic patients, 44% of the ESRD patient population (U.S. Renal Data Systems, 2007). In 2009 a total of 160,346 people with ESRD due to diabetes were living on chronic dialysis or with a kidney transplant. The percentage of new cases of ESRD caused by diabetes is highest among African-Americans. In 2007 the rate per million population for whites was 128, compared with 151 for Asians, 176 for Latinos, 333 for African-Americans, and 256 for American Indians (U.S. Renal Data Systems, 2009).
What are the two types of diabetes?
Type 2 diabetes, previously known as adult-onset diabetes or non–insulin-dependent diabetes mellitus (NIDDM), accounts for more than 90% of diabetes cases in the United States. This number is increasing because of the growth in the more susceptible minority populations. In this condition, insulin requirements are greater than the supply, or the patient’s cells are insulin resistant and require help using insulin. Dietary control, exercise, and weight loss are important factors in lowering insulin requirements and increasing insulin use. Family history, obesity, hypertension, and smoking are major risk factors for this type of diabetes. African-Americans, Latinos, and Asians are at a particularly higher risk for this type of diabetes.
How is diabetes treated?
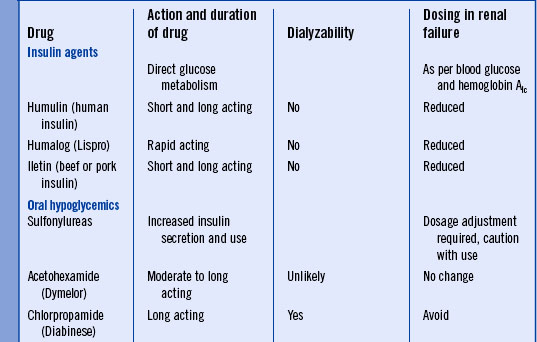
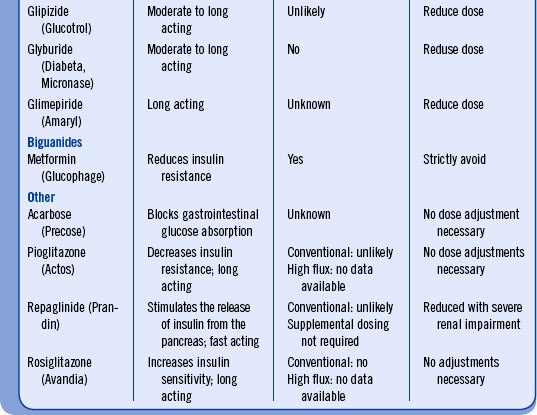
Diabetes is best managed with a multidisciplinary approach, in which the physician, nurse, and dietitian plan and implement a comprehensive plan of care. Often these professionals specialize in diabetic care and work with the primary care physician. The diabetologist (physician) determines the severity of the disease and assesses its effects. Other specialists, such as nephrologists and ophthalmologists, are consulted periodically for assessment of organ damage and for treatment. Annual visits to the ophthalmologist are necessary for all diabetic patients. A podiatrist should be consulted early to treat existing foot problems, assess risk of future problems, and recommend appropriate footwear. The medical goal is to arrest tissue and organ damage by normalizing the blood sugar. Among adults with diagnosed diabetes, 13% take both insulin and oral medications while 14% take only insulin. Oral medications alone are taken by 57% of those diagnosed with diabetes, and 16% do not take either insulin or oral hypoglycemics. (National Diabetes Information Clearinghouse, 2007). For the type 1 patient, glycemic control is achieved through diet, exercise, and insulin administration via subcutaneous injection or insulin pump. For the type 2 patient, the treatment varies and can be diet and exercise alone or may include an oral hypoglycemic agent and/or insulin injections. Monitoring of blood glucose values dictates the need for medication or dosage adjustments (Table 16-1). The dietitian creates a meal plan based on the American Diabetes Association guidelines and the individual’s lifestyle preferences. In addition, the dietitian teaches and counsels the patient about the vital role that diet and exercise play in the patient’s long-term outcomes. The nurse coordinates care, educates the patient and family about all aspects of care, and assesses all parameters of the patient’s health, including psychosocial adjustments, response to medication, diet and exercise, foot care, and other follow-up assessments as needed.
How is blood sugar measured and what is normal?
There are four blood sugar tests used for diagnosing and monitoring diabetes.
• A fasting blood glucose is measured after an eight-hour fast. For a nondiabetic patient, the range is 60 to 115 mg/dL. A value greater than 126 mg/dL on repeated studies may indicate diabetes.
• A random blood glucose greater than or equal to 200 mg/dL is diagnostic if accompanied by classic signs and symptoms.
• The oral glucose tolerance test measures both blood and urine glucose after the patient drinks a 75-g glucose solution. Normal blood values are less than 200 mg/dL after two hours. A value of 200 mg/dL or higher confirms a diagnosis of diabetes. The term impaired glucose tolerance is used if the value is between 140 and 190 mg/dL.
• Nurses teach patients or family members to perform a fingerstick blood sugar for ongoing monitoring and evaluation. It is not used to diagnose diabetes. As implied by the name of the test, blood is obtained from a finger stick, and the amount of glucose is measured by a handheld device called a glucometer.
What is diabetic nephropathy?
Diabetic nephropathy occurs in five stages:
Stage 1. Increased blood flow through the kidney (hyperfiltration) results in enlarged kidneys (renal hypertrophy).
Stage 2. This hyperfiltration of the glomeruli damages the membrane, causing it to leak larger molecules that normally would not pass across. The leak of albumin from the blood into the urine is known as microalbuminuria. As the loss of this and other proteins increase, the clearance of such waste products as urea and creatinine decreases.
Stage 3. Microalbuminuria exceeds 200 mcg/min.
Stage 4. Glomerular filtration rate (GFR) has dropped to 75 mL/min or less, proteinuria is significantly increased, and the patient has become hypertensive. This stage is called advanced clinical nephropathy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree