Dermatologic problems
 Just the facts
Just the factsIn this chapter, you’ll learn:
anatomy and physiology of the integumentary system
tests used to diagnose dermatologic problems in children
treatments and procedures for children with skin problems
dermatologic disorders that may affect infants, children, and adolescents.
Anatomy and physiology
The integumentary system, which consists of the skin and its components, is the largest organ system in the body. At birth, the skin is only 1 mm thick; the dermal layer of the skin doubles in thickness at maturity.
The great protector
The skin protects most of the other organ systems by acting as a mechanical barrier. Other functions include sensory perception, temperature regulation, vitamin synthesis, and excretion of wastes through sweating.
|
Structures of the skin
The skin is composed of layers of tissue. Appendages of the skin include the hair and glands.
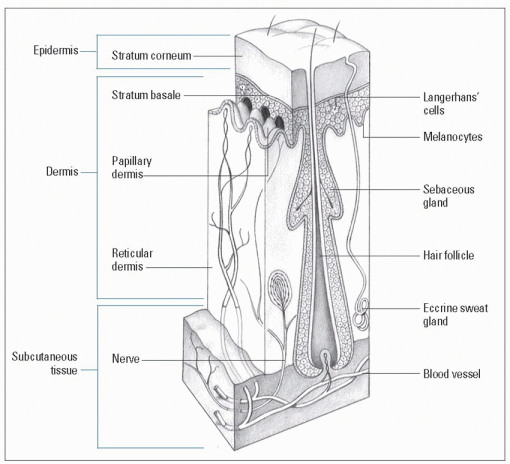
Skin layers
The skin consists of two layers and a sublayer, the hypodermis or subcutaneous tissue:
The epidermis, or outermost covering, provides a protective barrier to external trauma and limits the loss
of body contents to the environment; dermatologic problems are characteristically evident on the epidermis.
The dermis consists of connective tissue that gives the skin strength and elasticity; it contains blood vessels, lymphatics, and nerves.
The hypodermis lies below the dermis and is composed of loose connective tissue, or adipose tissue. It contains larger blood vessels, lymph channels, and nerve trunks. This layer attaches the skin to the underlying bones, acts as a cushion and temperature insulator, and determines the skin’s contours. (See Structure of the skin.)
Thin-skinned
Skin layers act to prevent water loss, which varies with environmental temperature and humidity as well as the proportion of body surface exposed. Thus, fluid loss in the preterm neonate is greater than in an adult because the neonate’s skin is thinner.
Hair
Hair changes markedly during the stages of development.
Fetal comb-over
Fine body hair, or lanugo, is found in utero over most of the fetus but decreases as the fetus approaches full-term. The neonate’s scalp hair varies greatly in amount and is usually lost before growth of permanent hair, which gradually thickens.
Growth spurt
Puberty causes additional growth of hair in the axilla and pubic regions of both genders; boys experience facial hair growth.
Glands
The main glands of the skin are:
sebaceous glands, or sebum-producing glands, which contain the hair follicles and keep the skin supple by minimizing water loss. They’re more prevalent on the scalp, forehead, nose, chin, and genitalia.
sweat glands, which may be eccrine (function as the body’s heat-regulating mechanism by producing sweat) or apocrine (mature at puberty and cause the unpleasant body odor associated with sweating).
Structure of the skin
Major components of the skin include the epidermis, dermis, and epidermal appendages (hair and glands).
|
Diagnostic tests
Various tests are used to help diagnose skin problems and related systemic diseases and to identify the causes of the disorder.
Potassium hydroxide preparation
Potassium hydroxide (KOH) preparation is an alkalinizing agent that’s used to prepare clinical specimens for microscopic examination needed to help diagnose fungal disorders.
Fungus finder
A drop of 20% KOH is added to skin scrapings to dissolve debris before the scrapings are placed on a slide. When the slide is heated, the skin cells dissolve, leaving fungal elements visible on microscopic examination.
Nursing considerations
Explain the procedure to the parents and the child. Tell the child what to expect, including discomfort he may experience, and suggest coping strategies such as distraction techniques.
|
Skin biopsy
Skin biopsy is the removal of a section or an entire lesion for microscopic analysis to determine its cell structure and make a diagnosis. (See Recognizing skin lesions.) A skin biopsy specimen can be obtained by:
shave biopsy
punch biopsy
excisional biopsy.
The closest shave
In a shave biopsy, the protruding portion of the growth is excised at skin level and the specimen is sent for microscopic examination.
Pulled and punched
In a punch biopsy, the skin surrounding the lesion is pulled taut, and the punch is introduced firmly into the lesion. The punch is then rotated to obtain a tissue specimen, or plug. The plug is lifted with forceps or a needle and the surgeon severs as deeply as possible into the fat layer. The wound is then sutured closed.
Out, out, darn lesion
In an excisional biopsy, a scalpel is used to excise the lesion completely.
Nursing considerations
Explain the procedure to the parents and child. Tell the child what to expect, including discomfort he may experience, and suggest coping strategies such as distraction techniques.
Need help remembering what to assess when evaluating a skin lesion? Just think about your ABCDs.
Asymmetry
Border
Color and configuration
Diameter and drainage.
Post punch, shave, and excise
After the procedure:
Apply a pressure dressing to the site.
Observe the site for bleeding.
Administer analgesics for pain as ordered.
Recognizing skin lesions
These illustrations depict the most common primary and secondary skin lesions.
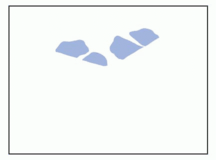
Macule
Flat, pigmented, circumscribed area less than 1 cm in diameter (freckle, rubella, petechiae)
|
Papule
Firm, inflammatory, raised lesion up to 0.5 cm in diameter, may be same color as skin or pigmented (acne papule, lichen planus, wart, basal cell carcinoma)
|
Plaque
Circumscribed, solid, elevated lesion more than 1 cm in diameter; elevation above skin surface occupies larger surface area compared with height (psoriasis, mycosis fungoides)
|
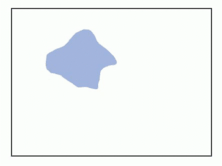
Patch
Flat, pigmented, circumscribed area more than 1 cm in diameter (herald patch [pityriasis rosea], Mongolian spots, vitiligo)
|
Nodule
Firm, raised lesion; deeper than a papule, extending into the dermal layer; 0.5 to 2 cm in diameter (intradermal nevus, keloid, lipoma)
|
Tumor
Elevated, solid lesion more than 2 cm in diameter, extending into dermal and subcutaneous layers (dermatofibroma, hemangioma)
|
Wheal
Raised, firm lesion with intense localized skin edema, varying in size and shape; color ranging from pale pink to red, disappears in hours (hive [urticaria], insect bite)
|
Comedo
Plugged pilosebaceous duct, exfoliative, formed from sebum and keratin (blackhead [open comedo], whitehead [closed comedo])
|
Cyst
Semisolid or fluid-filled encapsulated mass extending deep into the dermis (sebaceous cyst, cystic acne)
|
Vesicle
Raised, circumscribed, fluid-filled lesion less than 0.5 cm in diameter (chickenpox, herpes simplex)
|
Pustule
Raised, circumscribed lesion usually less than 1 cm in diameter; containing purulent material that makes it a yellow-white color (acne pustule, impetigo, furuncle)
|
Bulla
Fluid-filled lesion more than 2 cm in diameter; also called a blister (severe poison oak or ivy dermatitis, bullous pemphigoid, second-degree burn)
|
Atrophy
Thinning of skin surface at site of disorder (striae, aging skin)
|
Erosion
Circumscribed lesion involving loss of superficial epidermis (rug burn, abrasion)
|
Ulcer
Epidermal and dermal destruction may extend into subcutaneous tissue; usually heals with scarring (pressure ulcer)
|
Scale
Thin, dry flakes of shedding skin (psoriasis, dry skin, newborn desquamation)
|
Crust
Dried sebum, serous, sanguineous, or purulent exudate overlying an erosion or weeping vesicle, bulla, or pustule (impetigo, secondarily infected dermatitis)
|
Excoriation
Linear scratched or abraded area, usually selfinduced (abraded acne, eczema)
|
Fissure
Linear cracking of the skin extending into the dermal layer (hand dermatitis [chapped skin], interdigital tinea pedis)
|
Lichenification
Thickened, prominent skin markings from constant rubbing (chronic atopic dermatitis)
|
Scar
Fibrous tissue caused by trauma, deep inflammation, or surgical incision; red and raised (recent), pink and flat (6 weeks), and depressed (old) (on a healed surgical incision)
|
Tzanck test
Tzanck test is a microscopic examination of cells taken from skin lesions to aid in the diagnosis of vesicular diseases. Cells are scraped from the base of a vesicle to obtain moist, cloudy debris, or exudate. The cells are then placed on a slide, air-dried, and stained with Wright’s or Giemsa stain. Multinucleated giant cells are indicative of either herpesvirus or varicella.
Nursing considerations
Explain the procedure to the parents and the child. Tell the child what to expect, including discomfort he may experience, and suggest coping strategies such as distraction techniques.
Treatments and procedures
Management of skin disorders may include a variety of therapeutic procedures, including laser surgery and skin grafting.
Laser surgery
Laser is the common term for light amplification by simulated emission of radiation. Lasers are used in surgery to divide adhesions or to treat lesions of the skin. The most common types of lasers used are the pulsed dye laser, the argon laser, and the carbon dioxide laser, each of which emits light at a different wavelength.
Complications
Complications associated with laser surgery include secondary infections, keloid or pyrogenic granuloma formation, localized dermatitis, and hyperpigmentation or hypopigmentation.
Nursing considerations
Explain the procedure to the parents and the child and prepare the child for discomfort he may experience. Make sure to prepare the child (and the parents) for the appearance of the treated area after laser surgery because it will probably look much worse than it does before treatment (some laser treatments leave skin raw and oozing). Reassure the child that this is normal and the area will heal quickly.
Skin grafting
During skin grafting, a section of skin is separated from its blood supply and implanted over an area where skin has been lost due to burns, injury, or surgical debridement of diseased tissue.
‘Tis better to give than receive
The area from which the skin is removed is referred to as the donor site. For donor areas in which appearance or joint movement is important, the graft is transplanted intact. In flat areas where appearance is less critical, the graft may be meshed (fenestrated) to cover up to three times its original size. It’s then placed on what’s known as the recipient site.
A healthy loan
Skin from the patient’s own healthy skin (autograft) may be used. If an autograft isn’t available, a homograft (cadaver skin) or xenograft (pigskin) may be surgically attached.
Keys to success
The skin graft may be a split-thickness graft (involving the epidermis and superficial dermis) or a full-thickness graft (involving the epidermis and all layers of dermis). To be successful, grafts must have a sufficient blood supply, have contact with the recipient area, be free from infection and mechanical trauma, and have minimal bleeding or fluid accumulation.
Nursing considerations
Explain the procedure to the parents and the child. Prepare the child for the postgrafting appearance of the donor site and the recipient site. Reassure the child that the sites will heal, but tell him that this may take some time.
After graft
After grafting, follow these steps:
Observe the donor and graft sites dressings for fluid drainage and odor; if these occur, notify the doctor.
Observe the child for pain at the graft sites because this may indicate infection.
Monitor the child’s temperature every 4 hours because a rise in temperature may also indicate the present of infection.
Instruct the parents on the care of the donor and recipient sites and include them in the child’s care as much as possible (including dressing changes).
Teach parents to recognize the signs of infection (such as pain, a rise in temperature, fluid drainage and odor) and instruct them to report these signs immediately.
Stress to the parents (and the child) the importance of protecting the donor and recipient sites from trauma.
Encourage the parent to hold and comfort the child despite the presence of the bulky dressings; reassure them that the dressings allow them to hold their child without hurting him.
Dermatologic disorders
Dermatologic disorders that may affect children and adolescents include acne, burns, contact dermatitis, and scabies.
|
Acne
Acne is a chronic skin disorder of the pilosebaceous unit, which consists of sebaceous glands that produce sebum (an oily substance) and open onto the skin surface. Comedones, pustules, nodules, and nodular lesions characterize this inflammatory disease.
Facing up to acne
Acne is the most prevalent pediatric skin condition especially among adolescents and is typically observed on the face, chest, upper arms and back, and neck, where a large number of sebaceous glands are located. It appears predominantly during middle to late adolescence often paralleling puberty and with a peak incidence at ages 16 to 17 in girls and ages 17 to 18 in boys. It’s a common skin problem in all ethnic populations and affects males more severely than females. Neonatal acne takes approximately 1 month to resolve spontaneously.
Lasting legacy
Even though acne is self-limiting, the psychosocial impact and significance of acne on the quality of life of adolescents can have a negative effect on their self-esteem.
What causes it
Although the exact etiologic mechanism remains unknown, many factors affect the pathogenesis of the inflammatory response that’s evident in acne:
Androgenous hormones play a role in the development of acne; circulating androgens stimulate the production of sebum.
Many adolescent girls have an increased incidence of acne before their menstrual periods, also suggesting a hormonal link.
Genetic factors seem to play a role because acne appears to run in families.
Certain medications are known to aggravate acne, including corticosteroids, phenytoin, lithium, androgens, and hormonal contraceptives containing norethindrone and norgestrel.
Adolescents commonly cite stress as a precipitating factor, but there’s no evidence of a clear association.
Ingestion of specific foods, such as chocolate, hasn’t been found to be associated with the tendency to develop acne.
How it happens
Acne results from a combination of factors causing a keratin plug to develop within the follicular canal that opens onto the skin’s surface.
During adolescence, androgens stimulate sebaceous gland growth and production of sebum, which is secreted into dilated hair follicles that contain bacteria. The resulting environment permits the overgrowth of gram-positive bacteria known as Propionibacterium acnes and Staphylococcus epidermidis.
|
Volcanic eruption
Continued accumulation of follicular contents results in perforation of the follicular wall; the contents leak into surrounding tissue and cause an inflammatory reaction and the characteristic skin lesions of acne.
In full view
Inspection reveals acne lesions, most commonly on the face, neck, shoulders, chest, and upper back. The area around the infected follicle may appear red and swollen. The rupture or leakage of an enlarged plug into the dermis produces inflammation and characteristic acne pustules, papules, or, in severe forms, acne cysts or abscesses. If the patient has previously picked or squeezed the lesions, scars may be visible.
Acne classification
Classification of acne is based on the type of lesions observed. Mild acne involves primarily noninflammatory lesions with or without a limited number of inflammatory papules or pustules. Moderate acne involves noninflammatory lesions with more inflammatory papules and pustules present. Scarring is usually nonexistent or mild. Severe acne involves noninflammatory lesions along with numerous extensive inflammatory papules, pustules, and nodules. Scarring is more prevalent and usually dictates oral therapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access